CASE REPORT
Corneal Toxicity Following Exposure to Asclepias Tuberosa
Lauge Hjorth Mikkelsen1, Hassan Hamoudi2, Cigdem Altuntas Gül2, Steffen Heegaard1, 2, *
Article Information
Identifiers and Pagination:
Year: 2017Volume: 11
First Page: 1
Last Page: 4
Publisher ID: TOOPHTJ-11-1
DOI: 10.2174/1874364101711010001
Article History:
Received Date: 07/07/2016Revision Received Date: 20/12/2016
Acceptance Date: 02/01/2017
Electronic publication date: 31/01/2017
Collection year: 2017

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution-Non-Commercial 4.0 International Public License (CC BY-NC 4.0) (https://creativecommons.org/licenses/by-nc/4.0/legalcode), which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Purpose:
To present a case of corneal toxicity following exposure to milky plant latex from Asclepias tuberosa.
Methods:
A 70-year-old female presented with blurred vision and pain in her left eye after handling an Ascepias tuberosa. Clinical examination revealed a corneal stromal oedema with small epithelial defects. The corneal endothelium was intact and folds in Descemets membrane were observed. The oedema was treated with chloramphenicol, dexamethasone and scopolamine.
Results:
The corneal oedema had appeared after corneal exposure to the plant, Asclepias tuberosa, whose latex contains cardenolides that inhibit the Na+/ K+-ATPase in the corneal endothelium. The oedema resolved after 96 hours. After nine months the best corrected visual acuity was 20/20.
Conclusion:
Corneal toxicity has previously been reported for plants of the Asclepias family. This is a rare case describing severe corneal toxicity caused by exposure to latex from Asclepias tuberosa. Handling of plants of the Asclepias family should be kept as a differential diagnosis in cases of acute corneal toxicity.
Asclepias tuberosa (Fig. 1), also known as butterfly weed or orange milkweed, is a common garden plant native to North America. In traditional medicine Asclepias species have been used as treatment for bronchitis, tumours, and inflammation [1]. The milky latex of the plant is known to contain a mix of cardenolides, pregnane glycosides, and other cardiac glycosides [2]. The latex of A. tuberosa seems to be different from other members of the Asclepias family due to the fact that even though cardenolides are normally considered present in Asclepias species, these cardenolides have not been found in A. tuberosa. Instead some unique pregnane glycosides are found in A. tuberosa [2]. The toxic effect of the milky latex of A. fructicosa and A. curassavica on corneal endothelium has previously been described in two case reports [3, 4]. It is presumed that cardiac glycosides are able to penetrate the corneal epithelium leaving it intact and only being toxic to the endothelium [3, 4]. The slightly different composition of the Asclepias tuberosa latex seems to be toxic to corneal endothelium along with corneal epithelium.
CASE REPORT
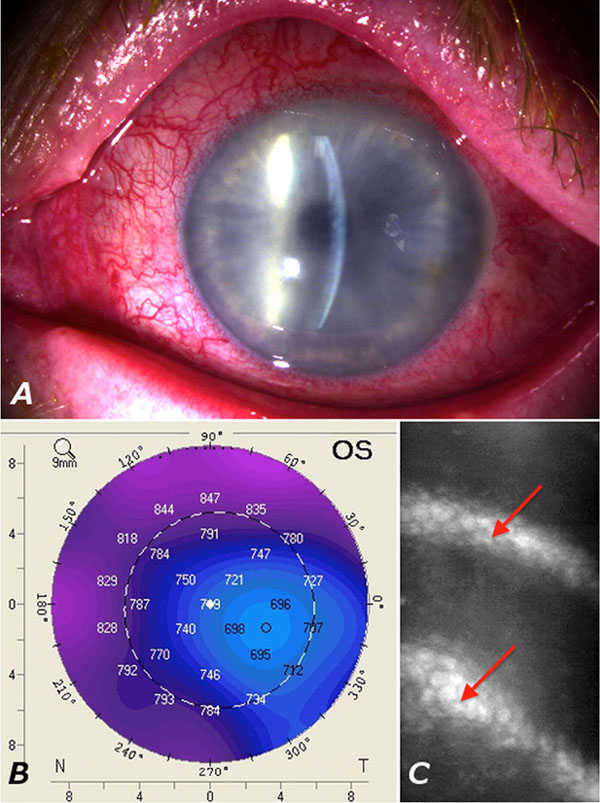
A 70-year-old female consulted the emergency department complaining of pain and blurred vision in her left eye. The evening before she handled an A. tuberosa and by accident got the latex in her left eye. This caused an immediate ocular discomfort. The pain and the blurred vision persisted during the night. On examination, the best-corrected visual acuity (BCVA) was 20/20 in the right eye and 20/400 improving to 20/125 with pinhole in the left eye. Slitlamp microscopy of the left eye revealed conjunctival and ciliary hyperaemia, stromal corneal oedema with folds in Descemets membrane together with small punctuate erosions of the epithelium (Fig. 2A). The anterior chamber could not be assessed in details due to the severe corneal oedema involving the entire cornea, but no hypopion was observed. Slitlamp examination of the right eye was normal. Applanation tonometry showed an intraocular pressure of 18 mmHg and pH measured in the inferior conjunctival fornix was 7.5 (measured with pH paper) in both eyes. Pentacam cornea topography showed a maximum central corneal thickness of 750 μm and a maximum peripheral corneal thickness of 847 μm (Fig. 2B). Topographical measurements of the right cornea were 580 μm and 705 μm respectively. Confocal microscopy confirmed the oedema in the stroma including folds in Descemets membrane in the left eye. Corneal endothelial cell density measurement was not possible due to the stromal oedema (Fig. 2C). The oedema resolved after 96 hours. After 3 weeks of observation and application of topical chloramphenicol 0.5%, dexamethasone 0.1% and scopolamine 0.2%, the patient had no pain or discomfort. The BCVA had improved to 20/63 in the left eye and the cornea was clear with intact epithelium. Nine months later the BCVA improved to 20/20 in both eyes. Lubricants were not used for the management of corneal oedema in the present case.
DISCUSSION
The corneal endothelium is crucial to the maintenance of corneal transparency by removing water from the corneal stroma. This function is carried out by several active transport mechanisms that involve HCO3-, Cl- and carbonic anhydrase activity. The main driving potential for these transport mechanisms is produced by the Na+/K+-ATPase, and any disturbance of the enzymatic activity or the amount of Na+/K+-ATPases will result in corneal oedema [5].
Cardiac glycosides are effective inhibitors of Na+/K+-ATPase, where they bind to the α1-subunit [6]. Pregnane glycosides are potential precursors for cardenolides and both belong to the family of cardiac glycosides – the family also includes digitoxin. It is known that Asclepias species contain different cardiac glycosides and it seems that the plants concentrate these glycosides to the highest degree in their milky latex [6]. Thus, corneal exposure to Asclepias latex causes swelling of the cornea due to inhibition of the Na+/K+-ATPase. This resembles the effect seen after topical application of digitoxin that causes digitalis keratopathy [3]. Due to intercellular sealing of the corneal and conjunctival epithelia, steroids, pregnane glycosides and other lipophilic molecules are only partly able to pass paracellularly in the epithelium. In addition, some transcellular transport through the corneal epithelium takes place [7, 8].
In the present case, immediate discomfort subsequent to plant latex exposure was seen together with later onset of pain and blurred vision in the affected eye. Pain and corneal epithelial damage were observed in our case – these features were absent in previous reports. In previous cases BCVA after three weeks of observation ranged from 20/20 to 20/40 in the affected eyes [3, 4]. BCVA in the present case was only 20/63 in the affected left eye and 20/20 in the unaffected right eye after 3 weeks. It is possible that the specific pregnane glycosides of A. tuberosa are more potent inhibitors of the Na+/K+-ATPase than the cardenolides found in other Asclepias species. Another explanation may be that some chemical substance or a physical property in the plant latex of A. tuberosa also has a toxic effect on the corneal epithelium. Epithelial damage makes a route for glycosides to reach the endothelium in higher concentrations. The previous cases showed complete remission of the oedema after 48-72 hours with lubricant eye drops alone or in combination with dexamethasone [3, 4]. Dexamethasone increases the Na+/K+-ATPase activity by increasing the expression of the α1-subunit as well as increasing the α1-subunit enzymatic activity [9].
A case in which corneal exposure to milky plant latex of Asclepias tuberosa caused corneal oedema and toxicity is reported. In the present case, the oedema resolved completely after 96 hours. The toxicity was treated with application of topical antibiotics, scopolamine and dexamethasone. The remission time is 24 hours later than previously reported cases. The prolonged remission time may be due to the presence of epithelial damage in the present case. The slightly different composition of the milky latex of A. tuberosa compared to other members of the Asclepias family may result in toxicity to the corneal epithelium along with the corneal endothelium. Exposure to plant latex from the Asclepias family should be kept as a differential diagnosis in cases of acute corneal toxicity. The effect of the topical treatment with dexamethasone on the spontaneous remission of the condition is questionable but should be administered to hasten the resolution of corneal epithelial toxicity and oedema. A detailed history and plant description in future cases of corneal toxicity due to plant exposure would be helpful in pointing out towards more species capable of causing potential corneal toxicity.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
We acknowledge the kind help received from the gardeners Jimmi Olsen and Johnny Busch, Botanical Garden, Natural History Museum of Denmark, University of Copenhagen, Copenhagen, Denmark.