All published articles of this journal are available on ScienceDirect.
Antibiotic Prophylaxis in Orbital Fractures
Abstract
Purpose:
To determine whether prophylactic antibiotic use in patients with orbital fracture prevent orbital infection.
Design:
Retrospective cohort study.
Participants:
All patients diagnosed with orbital fracture between January 1, 2008 and March 1, 2014 at The George Washington University Hospital and Clinics.
Main Outcome Measures:
Development of orbital infection.
Results:
One hundred seventy-two patients with orbital fracture met our inclusion and exclusion criteria. No orbital infections were documented. Twenty subjects (12%) received no prophylactic antibiotic, and two (1%) received only one dose of antibiotics pre-operatively for surgery. For primary antibiotic, 136 subjects (79%) received oral antibiotics, and 14 (8%) received intravenous (IV) antibiotics (excluding cefazolin). Cephalexin and amoxicillin-clavulanate were the most prescribed oral antibiotics that are equally effective. Five-to-seven day courses of antibiotics had no increased infections compared to ten-to-fourteen day courses. Calculated boundaries for effectiveness of prophylactic antibiotics ranged from a Number Needed to Treat (NNT) of 75 to a Number Needed to Harm (NNH) of 198.
Conclusion:
Antibiotics for prevention of orbital infection in patients with orbital fractures have become widely used. Coordination between trauma teams and specialists is needed to prevent patient overmedication and antibiotic resistance. Should antibiotics be used, shorter courses and avoidance of broad spectrum agents are recommended. Additional studies are needed.
INTRODUCTION
The use of antibiotics for prophylaxis of orbital infection after an orbital fracture is widespread. A survey on rates of prophylactic antibiotic use in Britain in 2000 reported that 47% of Ear, Nose, and Throat (ENT) physicians prescribed antibiotics at time of diagnosis [1]. Unfortunately, little to no evidence exists that such use of antibiotics has any therapeutic effect [2], and reports of bacterial resistance have become increasingly common [3]. Thus, all practitioners should review the evidence to support their prescribing habits. We aim to provide the largest and most thorough study to date analyzing the evidence for antibiotic use in prevention of orbital infection after an orbital fracture.
METHODS
Institutional Review Board approval was obtained, and the study was HIPPA compliant. A medical record review was performed of all patients who were treated at The George Washington University (GWU) Department of Ophthalmology and Otolaryngology (ENT) clinics for an orbital fracture between January 1, 2008 and March 1, 2014. A computer database search using ICD-9 codes 802.0, 802.1, 802.4, 802.5, 802.6, 802.7, 802.8, and 802.9 generated a list of potential subjects; two independent researchers subsequently reviewed each chart, and discordant results were double checked for accuracy. Inclusion criteria consisted of having an orbital fracture (medial, lateral, floor, and/or orbital roof fracture) diagnosed with Computerized Tomography (CT) imaging at the GWU Emergency Department or at a different emergency department if adequate scanned records were present. Subjects were excluded from the study if they had co-morbid conditions necessitating the use of therapeutic antibiotics not solely for the purpose of orbital infection prophylaxis. Additionally, ICD-9 codes of 376.00 and 376.01 were searched to make sure no cases of orbital infection were missed.
Prophylactic antibiotics were defined as antibiotic use for the prevention of orbital infection started within five days of diagnosis of orbital fracture. Corticosteroid use was documented if more than one dose of oral or IV steroids were given within the first week of diagnosis of orbital fracture. All CT findings were collected from the radiologist’s final report. Statistical analysis was performed using the one-tailed two-proportion z-test using Microsoft Excel.
RESULTS
Patients in our study ranged in age from 17 to 91, with an average age of 39 years. One hundred twenty-two patients (70%) were male, and 50 (30%) were female.
One hundred ninety-four cases of orbital fracture were identified. Fourteen patients received antibiotics not solely for the purpose of prophylaxis and thus were excluded. We excluded an additional eight cases due to inadequate records; all of these cases received initial treatment at an emergency department other than GWU. Thus, 172 cases met our inclusion and exclusion criteria. No cases of orbital infection were identified in our study. Thirty percent of patients had follow up longer than 3 months, 20% between 1 and 3 months, 18% between 2 weeks and 1 month, 20% between 1 and 2 weeks, and 12% less than 1 week.
Sixty-one subjects received a course of steroids to reduce swelling, and one patient was on prednisone chronically, resulting in 62 patients that were immunosuppressed. Patients who received steroids were more likely to receive antibiotics: One of 20 patients (5%) who did not receive antibiotics received steroids, and 61 of 152 patients (40%) who received antibiotics also received steroids.
Since many subjects in our study received more than one antibiotic, the longest course given was recorded as the primary antibiotic. As shown in Table 1, additional courses were recorded as well. Twenty subjects (12%) received no prophylactic antibiotic, and 2 (1%) received only one dose of antibiotics pre-operatively for surgery. For primary antibiotic, 136 (79%) received oral antibiotics, and 14 (8%) received intravenous (IV) antibiotics (excluding cefazolin). Cefazolin was counted separately from other stronger IV antibiotics to avoid misrepresenting the percentage of broad-spectrum IV antibiotics prescribed. A total of 29 subjects (14%) received IV antibiotics at some point during the first week for prophylaxis. In addition, 25% of subjects received two different antibiotics, 7% received three antibiotics, and one subject received four antibiotics.
| Type | Primary | 1st Additional | 2nd Additional | 3rd Additional |
|---|---|---|---|---|
| No Antibiotic | 20 | |||
| OR Antibiotics | 2 | 9 | 3 | 0 |
| Penicillin | 1 | 0 | 0 | 0 |
| Azithromycin | 1 | 0 | 0 | 0 |
| Cefazolin | 5 | 22 | 2 | 0 |
| Cephalexin | 55 | 2 | 2 | 0 |
| Amoxicillin | 12 | 0 | 1 | 0 |
| Amoxicillin-Clavulanate | 46 | 1 | 1 | 0 |
| Ciprofloxacin | 1 | 0 | 0 | 0 |
| Levofloxacin | 1 | 0 | 0 | 0 |
| Cefdinir | 1 | 0 | 0 | 0 |
| Clindamycin | 14 | 1 | 2 | 0 |
| Clindamycin-IV | 10 | 7 | 2 | 0 |
| Ampicillin/Sulbactam | 1 | 4 | 0 | 0 |
| Piperacillin/Tazobactam | 2 | 0 | 0 | 0 |
| Ceftriaxone | 1 | 0 | 1 | 0 |
| Vancomycin | 0 | 0 | 0 | 1 |
The most common primary antibiotics prescribed were cephalexin (55 subjects) and amoxicillin-clavulanate (46 subjects). Table 2 shows the duration of antibiotic course for the four most commonly prescribed antibiotics. Based on our data, a five-to-seven day course was as effective as a ten-to-fourteen day course.
| Antibiotic | 5 day | 7 day | 10 day | 14 day |
|---|---|---|---|---|
| Cephalexin | 3 | 30 | 13 | 2 |
| Amoxicillin-Clavulanate | 3 | 25 | 15 | 1 |
| Amoxicillin | 1 | 5 | 3 | 1 |
| Clindamycin | 1 | 6 | 6 | 0 |
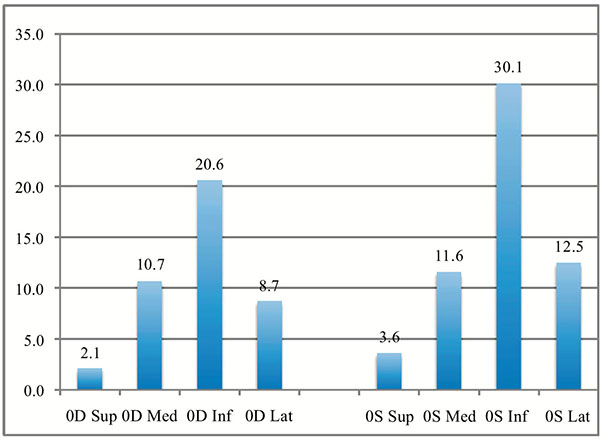
Sup = superior wall, Med = medial wall, Inf = inferior wall, Lat = lateral wall
All 194 patients were included for orbital fracture analysis. The most common fracture by location was the orbital floor (20.6% and 30.1% on the right and left, respectively). Interestingly, all left-sided fractures were more common than right-sided fractures when analyzed in aggregate (p<0.01), as depicted in Fig. (1). When each wall was analyzed separately, only lateral (P<0.05) and inferior (p<0.01) orbital fractures were significantly more common on the left compared to the right. Although the medial wall of the orbit is much weaker than the lateral wall, both were fractured at nearly identical rates, possibly due to the lateral wall’s increased vulnerability to trauma (such as a fist). Table 3 shows the breakdown by type of fracture and location.
| Right Orbit | Left Orbit | |||||||
|---|---|---|---|---|---|---|---|---|
| Superior | Medial | Inferior | Lateral | Superior | Medial | Inferior | Lateral | |
| Unknown | 0 | 3 | 3 | 0 | 0 | 2 | 2 | 0 |
| Non-displaced | 4 | 15 | 12 | 9 | 7 | 17 | 33 | 16 |
| Displaced | 2 | 8 | 16 | 5 | 2 | 9 | 21 | 10 |
| Comminuted | 1 | 10 | 38 | 15 | 3 | 11 | 45 | 16 |
| Total | 7 | 36 | 69 | 29 | 12 | 39 | 101 | 42 |
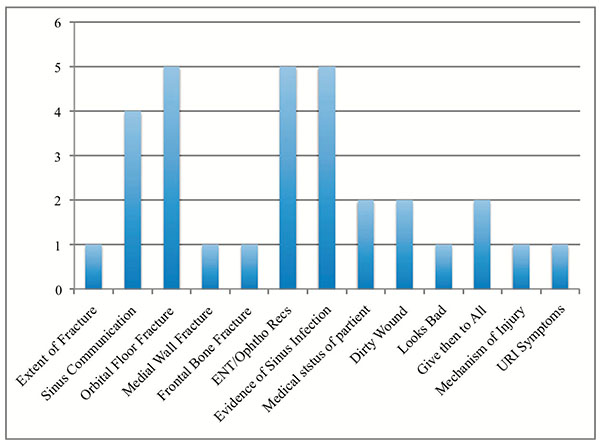
In addition to our retrospective study, we surveyed doctors from Ophthalmology, ENT, and Emergency Medicine about antibiotic use. Reported rates of antibiotic use ranged from 0-100%, with an average of 61%. Among specialties, Emergency Medicine reported the highest rate of antibiotic use (70%), while ENT and Ophthalmology had lower reported rates of use (52% and 42%, respectively). In addition, providers were asked how they determined to whom to give antibiotics, with responses shown in Fig. (2).
DISCUSSION
In 1991, Westfall et al. extrapolated from the general surgery literature that wounds involving preexisting infection would have an infection rate of 40% and thus recommended that antibiotic prophylaxis be used based on wound classification [4]. Current guidelines have hardly improved and defer the use of prophylactic antibiotics to the prescribing physician [5], and a recent systematic review of antibiotics for perioperative facial fractures concluded use of antibiotics for upper facial fractures is not supported by literature [6]. As our study shows, these lack of concrete guidelines leads to high rates of antibiotic use with 90% of patients receiving antibiotics, 25% receiving two antibiotics, and 7% receiving three different antibiotics solely for prophylaxis. This is exemplified in literature as studies recommend antibiotics are part of a conservative approach to managing non-operative fractures [7]. Possible explanations for such high rates of use in absence of quality evidence include physician overestimation of antibiotic effectiveness, the desire to avoid litigation, and poor coordination among subspecialties. Patients with orbital trauma are treated by a variety of subspecialties including ophthalmology, otolaryngology, general surgery, and emergency medicine physicians. If communication is poor, each team may prescribe additional antibiotics due to a lack of awareness of what the other teams may have prescribed. Our survey data exemplifies this, as individual providers reported much lower rates of antibiotic use than the actual rate patients received.
Twenty patients in our study received no prophylactic antibiotics without consequence, and an additional two patients received only one dose of oral antibiotics without consequence. Although these patients were less likely to receive steroids, there was no statistical difference in fracture complexity between those that did and did not receive antibiotics. Furthermore, there was no consequence to using cephalexin instead of stronger antibiotics such as amoxicillin-clavulanate or clindamycin, and shorter five-to-seven day courses were as effective as longer ten-to-fourteen day courses.
As our survey revealed, in the absence of a treatment paradigm, current use of antibiotics is haphazard at best. The most common reasons for using antibiotics were evidence of sinus infection, ENT/Ophthalmology recommendations (which highlights the importance of developing treatment guidelines), and presence of a floor fracture. Based on published case reports since 1980, 6 out of 10 reported cases of post-traumatic cellulitis were associated with an upper respiratory infection [8-11]. At our hospital, this reason was one of the lowest reported for antibiotic use.
Since no cases of orbital infection were identified in our study, we were unable to calculate directly the effectiveness of prophylactic antibiotics, however, by extrapolating our study findings we were able to indirectly calculate them. In an Australian study from 2005, Ben Simon et al. reported on four cases of post-traumatic orbital infection out of 497 fractures, with a rate of infection of 0.8% [9]. Unfortunately, Ben Simon et al. did not report on the rate of antibiotic use in their study. With assumptions, though, one can calculate the boundaries of antibiotic effectiveness. Three of the four cases of infection in their study received antibiotics; if one assumes reasonable rates of antibiotic use, the number needed to treat (NNT) and the number of preventable infections in the US can be calculated as shown in Table 4 [8]. Based on these calculations, the maximum effectiveness of prophylactic antibiotics is a NNT of 75. Even with an assumption of maximal effectiveness, antibiotics fall short of FDA standards [12]. It is possible, however, that antibiotics actually are harmful (with a number needed to harm of 198), meaning for nearly every 200 patients who were prescribed antibiotics, one infection was caused. This last calculation should be quite alarming: Antibiotics not only can be ineffective but also could be harmful to patients. Reasons for this may be due to impairment of normal host flora or selection for more resistant strains.
| % Given Atbx | NTT | Preventable Infections in US |
|---|---|---|
| 90% | 75 | 1105 |
| 80% | 398 | 207 |
| 75% | 0 | 0 |
| 60% | -198 | -414 |
In summary, antibiotics use has become very common for prophylaxis of infection after orbital fracture without strong evidence to support their use. Our study highlights the importance of communication amongst specialties to prevent multiple agents being given to the same patient. Furthermore, it appears that for low risk patients (those without URI and not using steroids), antibiotics may be withheld; should antibiotics be prescribed, we recommend shorter five to seven day courses of cephalexin. More studies are needed to evaluate the role of antibiotic use after orbital fracture.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No Animals/Humans were used for studies that are base of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


