CASE REPORT
Bilateral Idiopathic Sclerochoroidal Calcifications
Venkatesh L. Brahma1, *, Sumit P. Shah1, Nauman A. Chaudhry2, Jonathan L. Prenner1
Article Information
Identifiers and Pagination:
Year: 2017Volume: 11
First Page: 76
Last Page: 79
Publisher ID: TOOPHTJ-11-76
DOI: 10.2174/1874364101711010076
Article History:
Received Date: 30/06/2016Revision Received Date: 20/12/2016
Acceptance Date: 15/03/2017
Electronic publication date: 27/04/2017
Collection year: 2017

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Sclerochoroidal calcification (SCC) is a rare and benign condition found mostly in middle-aged and elderly Caucasian men, characterized by multiple yellow-white lesions seen most commonly in the temporal regions of the fundus. While they may be concerning for benign tumors, primary neoplasias or metastases, SCCs most commonly present as asymptomatic findings during routine ophthalmologic testing and have a very good prognosis as they rarely cause visual deficits.
Objective:
To report and describe the findings in a case of bilateral idiopathic sclerochoroidal calcifications.
Methods:
A retrospective case report.
Results:
Repeated ophthalmological exams, including fundoscopic examination, ultrasonography, optical coherence tomography and fluorescein angiography, were all consistent bilateral idiopathic sclerochoroidal calcifications.
Conclusion:
While most cases of idiopathic sclerochoroidal calcifications represent a benign ophthalmological condition, there are known associations with other systemic conditions, such as hyperthyroidism, hyperparathyroidism, Bartter’s syndrome and Gitelman’s syndrome. It is for this reason that these patients warrant a full systemic work-up in addition to careful ophthalmological monitoring.
CASE REPORT
A 71-year old white male was referred for hyperopic refractive shift. On exam, best corrected visual acuity was 20/25 in both eyes. Anterior segment exam was unremarkable. Fundus examination revealed multiple (around 2-3) yellowish elevated choroidal lesions in both eyes, the largest one with a diameter of approximately 10 mm. seen throughout the superotemporal macula as well as the superotemporal periphery. There was no associated subretinal fluid, heme or significant retinal pigment epithelium changes. B-scan ultrasonography showed moderate solid appearing elevations (<4mm), as well as high internal reflectivity. Systemic work up for potential associations was negative; the patient underwent extensive systemic workup including a complete blood count, comprehensive metabolic panel (including serum calcium testing), phosphorus and magnesium levels, all of which were within normal limits.
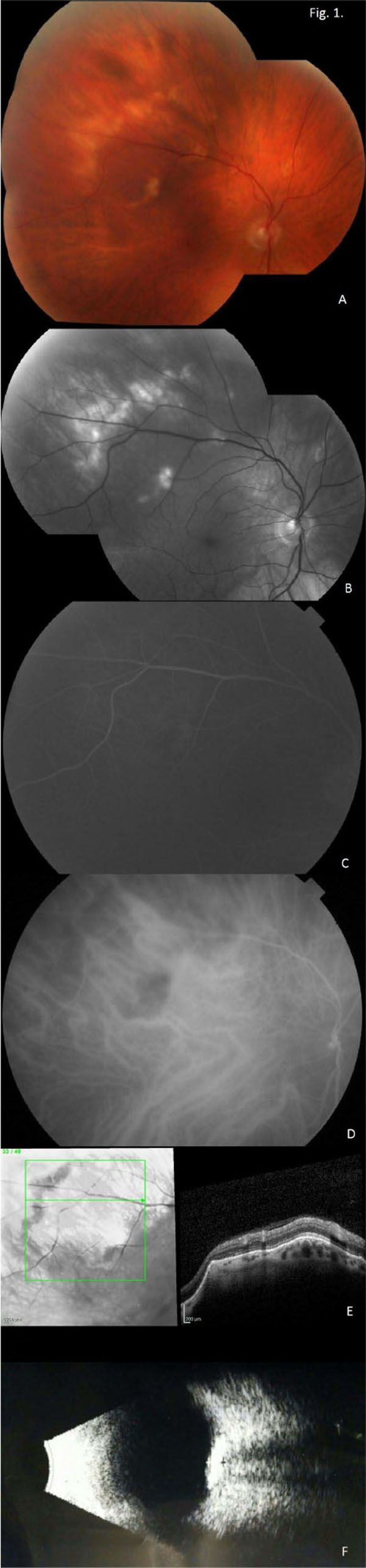
Montage fundus photographs show yellow-white lesions in the superotemporal macula and periphery of the right and left eyes (Figs. 1A and 2A, respectively). Red-Free montage images highlight the lesions in the right and left eyes (Figs. 1B and 2B, respectively). Fluorescein angiogram shows staining in the late phase of the right and left eyes (Figs. 1C and 2C, respectively). Indocyanine green angiography showed hyper-fluorescence in the corresponding regions of the right and left eyes (Figs. 1D and 2D, respectively). Optical coherence tomography images show an elevated lesion of the choroid in the right and left eyes (Figs. 1E and 2E, respectively), with maintenance of the normal retinal architecture. Lastly, B-scan ultrasonography showed solid appearing hyper-echoic elevations in the sclera and choroid with posterior shadowing in the right and left eyes (Figs. 1F and 2F, respectively).
CONCLUSION
Sclerochoroidal calcifications warrant a full ophthalmologic and systemic workup as a minority of the cases of SCCs are associated with endocrinologic pathology including hyperthyroidism and hyperparathyroidism [1]. Associations have also been reported with nephrologic pathology such as Bartter’s [2] and Gitelman’s syndromes [3]. Therefore, thyroid hormone levels, calcium and phosphorus levels, magnesium levels, and BUN and creatinine are all recommended for patients suspected to have sclerochoroidal calcifications. Additionally, these patients should undergo routine ophthalmological evaluation to assess for any further progress of the disease process.
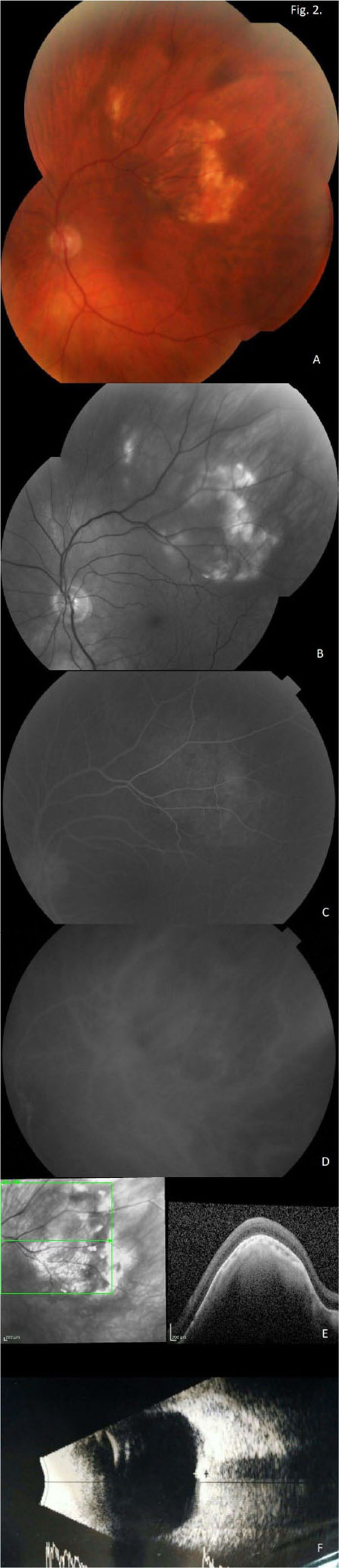 |
Fig. (2). Respective left eye images. |
LIST OF ABBREVIATION
| SCC | = Sclerochoroidal Calcification |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No Animals/Humans were used for studies that are base of this research.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
None of the authors have any financial/conflicting interests to disclose.
AUTHORS’ CONTRIBUTIONS
VLB helped draft the manuscript. SPS, NAC and JLP identified the patient, performed physical examination and necessary ophthalmological exam, and helped draft the manuscript.
ACKNOWLEDGEMENTS
Declared none.