All published articles of this journal are available on ScienceDirect.
The Pattern, Presentation and Risk Factors of Ocular Trauma Among Patients Treated at Hawassa University, Referral Hospital
Abstract
Background:
Ocular trauma is a significant public health problem which may lead to permanent visual impairment. Being preventable, the visual impairment can occur at any age in either sex and has significant socioeconomic burden especially in developing countries.
Objective:
To assess the pattern, presentation and risk factors of ocular trauma in patients treated at Hawassa University, Referral Hospital, South Ethiopia
Methods:
The study was conducted from August 01, 2014 to July 31, 2015, and all patients who visited Hawassa University, Referral Hospital for ocular trauma were included in the study. Data entry and analysis was done using SPSS version 20 and the descriptive and analytic statistics were carried out.
Results:
A total of 335 patients were included into the study. Ocular trauma was observed mostly in children (65.67%) and rural dwellers (76.12%). Assault trauma and surgery, secondary to trauma, were associated with open globe injury (P = 0.021, AOR = 43.17 and P = 0.006, AOR = 25.67, respectively). The corneal tear was the most frequently observed finding (59.70%). Most of the patients (>90%) presented after 6 hours from time of ocular trauma and the treatment was commenced also after 6 hours in >95% of them. Among all patients included in the study, 59.71% of them were with visual acuity of <3/60 at presentation.
Conclusion:
Ocular trauma was high in males, children, rural dwellers and low income families and most of the patients (>90%) presented after 6 hours from time of ocular trauma.
1. INTRODUCTION
The eye is the third most common organ affected by trauma, after hands and feet. But it represents only 0.27% of the total body surface area and 4% of the facial area [1].
Ocular trauma is a significant preventable public health problem especially in developing countries and it may lead to permanent visual impairment [1-7]. Ocular trauma may occur at any age in either sex [1, 4], especially among pediatric and elderly population [1]. According to both hospital and population based studies, males are more affected by ocular trauma [1, 2, 4, 7].
As estimates of World Health Organization (WHO), the global annual incidence of ocular trauma is around 55 million [3, 6, 8]. Globally, blindness in 1.6 million people is due to ocular trauma [1, 7-9].
Corneal tear, sclera tear and lens damage were the most frequently observed morbidities of ocular trauma and lid and canalicular laceration, uveal prolapse, anterior chamber abnormality, retinal detachment and optic nerve avulsion were also repeatedly observed [1, 2, 8, 10, 11].
Majority of the patients were presented to eye health facilities after 24 hours from time of trauma [1-3, 5, 6, 10, 12]. Patients reported within 24hrs of eye injury showed better visual outcome after treatment than patients reported after 24hrs [2].
Ocular trauma has a direct and an indirect impact on the social and economic importance of human being and millions of dollars will be lost annually due to visual impairment caused by ocular injury [1, 5, 6].
In a study conducted in Grarbet, Ethiopia, most of the patients (67.6%) were presented for the treatment of ocular trauma on the third day and later [5]; however, no studies had been carried out on the pattern, presentation and risk factors of ocular trauma in the study area. So, in view of public health importance, this study will provide information for respective stack holders for planning and implementing preventive and curative measures.
2. MATERIALS AND METHODS
Hospital based study was conducted from August 01, 2014 to July 31, 2015 in Hawassa University, Referral Hospital, Ophthalmology Department. Hawassa University, Referral Hospital is found in Hawassa town, South Ethiopia, about 275Kms from Addis Ababa, the capital city of Ethiopia. The tertiary eye care center was established in 2005 by the support of Orbis International-Ethiopia. This tertiary eye care center serves approximately 14 million people of a catchment area. With pediatrics, retina and binocular vision and refraction clinics comprehensive eye care services are being provided in the center, both in outpatient and inpatient departments. There are 3 ophthalmologists, 10 optometrists, 1 ophthalmic officer, 1 cataract surgeon, 8 ophthalmic nurses and 3 primary eye care workers providing the service.
The study included all patients who visited Hawassa University, Referral Hospital, Ophthalmology Department for ocular trauma from August 01, 2014 to July 31, 2015. Patients who were unable/ unwilling to respond for the questions were excluded from the study.
The dependent variable was ocular trauma and the independent variables were socio-demographic data (sex, age, residence, religion, occupation, level of education, income), the distance from hospital, place where trauma occurred, type of object that causes trauma, occasion of trauma, time of presentation, time of intervention and Visual Acuity (VA) (at presentation and after treatment).
Data abstraction form and questions were developed based on the literature, to obtain information on socio-demographic characteristics and other factors. This form was pretested in 5% of the sample and modified accordingly.
The data collection was performed using questioner and through observation. There were five optometrists, four ophthalmic nurses and one ophthalmic officer for data collection and one ophthalmologist for supervision.
The collected data was checked out for the completeness, accuracy and clarity by principal investigator and supervisor on daily basis. The supervisor checked the filled data daily and amendments were done at the spot. Data clean up, double entry and cross-checking were done before analysis.
After coding, the data was entered and analyzed using SPSS version 20. The descriptive statistics, bivariate and multivariate logistic regressions were carried out. The variables that were found being significant (p ≤0.2) in bivariate logistic regression were entered into multivariate logistic regression model. A P-value <0.05 was considered statistically significant.
Before conducting the study, ethical clearance was obtained from the Institutional Review Board of Hawassa University, College of Medicine and Health Sciences. Official permission from the hospital was obtained. Though people were not either exposed to unnecessary risk or inflicted harm during primary data collection, an oral and written informed consent of each participant was taken after explaining the purpose of the study. For children, the consent was done through their legal representatives. Confidentiality of the information was maintained thoroughly by excluding names as identification in the questioner and data abstraction form and keeping their privacy during data collection. Their charts were returned to chart room soon after collecting the necessary data. No one had access to the non-coded data except investigators, data collectors and supervisor due to responsibilities associated with the study.
3. RESULTS
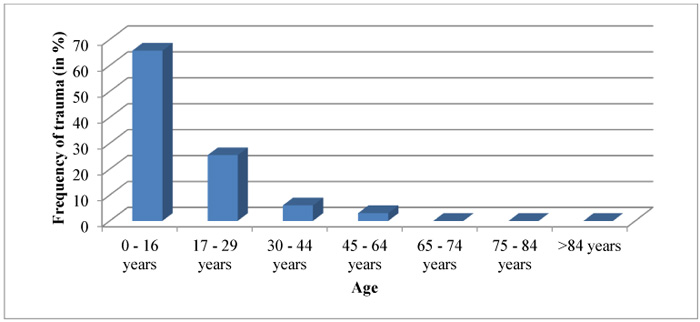
A total of 335 patients (73% males and 27% females) presented with ocular trauma were examined and interviewed using structured questioner. From 2 months to 64 years old patients visited during the study period were included in the study. Ocular trauma was occurred mostly in children (65.67%), followed by adolescents (25.37%). The occurrence of ocular trauma is relatively low as the age increases (Fig. 1).
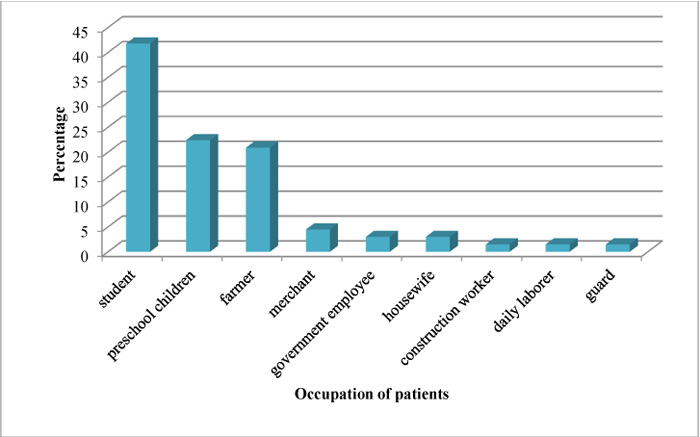
Ocular trauma was frequently observed in urban residents (76.1%, n=255) as compared to rural dwellers (23.9%, n=80). From all patients visited for ocular trauma, most of them (38.81%) were Islamic religion followers, followed by Protestants (35.82%). The occurrence of trauma was frequently observed in students (41.79%) (Fig. 2).
Most of the patients who visited the hospital for ocular trauma had dropped their education at primary school (59.70%, n=200) and 28.4% (95) were illiterates. No report of ocular trauma of first degree holders and above. Nearly 87% of patients were from a family whose household monthly income is up to 3,000 Ethiopian birr (177$) and the rest were from a family whose household monthly income is >3,000 Ethiopian birr (Table 1).
| Monthly household income (in birr) | Frequency (%) |
|---|---|
| 0-499 | 50(14.9) |
| 500-999 | 85(25.4) |
| 1000-1999 | 75(22.4) |
| 2000-2999 | 80(23.9) |
| 3000-5000 | 25(7.5) |
| >5000 | 20(6.0) |
| Total | 335(100) |
The health facility was found in <20 Km for 90.63% (304) patients, in 20-100 Km for 7.81% (26) patients and in >100Km for 1.56% (5) patients from their residence area. But, about 80% health facilities where the patients visited for ocular trauma were not providing eye care services. From 20% health facilities where eye care services were available; in 38.46% (26) of them only patching service was provided, in 30.77% (21) of them medical treatment was given and in 23.08% (16) of them nothing was done.
The occurrence of ocular trauma at mid day and at evening was found to be proportional (41.79% each) and at morning it was 13.43% as well as at night it was 2.99%. In 31.34% (105) patients, the trauma occurred at street (Table 2). From a total females who visited the hospital, 50.0% of trauma occurred at home and there was no a trauma occurrence at farm place. On the other hand, from total males, proportional trauma occurrence was observed both at home and at farm place (18.4% each).
| The place where ocular trauma was occurred | Frequency (%) |
|---|---|
| Street | 105(31.3) |
| Home | 90(26.9) |
| Compound | 80(23.9) |
| Farm place | 45(13.4) |
| Public building | 15(4.5) |
| Total | 335(100) |
In 47.76% (160) patients ocular trauma was caused by wood/ stick (Fig. 3). About 87% (291) of trauma occurred accidentally and 13% (44) of them by assault. Assault trauma was associated with open globe injury (P = 0.021, AOR = 43.167).

Most of the patients (71.64%, n=234) have travelled >100Km to get a treatment at Hawassa University, Referral Hospital; 19.40% (65) patients have travelled 20-100 Km and 8.96% (30) patients have got a treatment travelling only < 20 Km. Most of the ocular injuries were open globe (65.67%) (Table 3).
| Type of injury | Frequency (%) | ||
|---|---|---|---|
| Open globe injury | Laceration | Penetrating globe injury | 145(43.3) |
| IOFB | 25(7.5) | ||
| Perforating globe injury | 40(11.9) | ||
| Rupture | 10(3.0) | ||
| Closed globe injury | Contusion | 93(27.8) | |
| Lamellar laceration | 22(6.6) | ||
| Total | 335(100) | ||
All ocular structures, from anterior to posterior segment, were affected by trauma. Among all (335) cases, corneal tear was the most frequently observed case (59.70%), followed by lens damage and anterior chamber abnormalities (25.37% each) (Table 4).
| Pattern of ocular trauma | Frequency (%) |
|---|---|
| Corneal tear | 200(59.7) |
| Lens damage | 85(25.4) |
| Anterior chamber abnormality | 85(25.4) |
| Uveal prolapse | 75(22.4) |
| Eyelid damage | 40(11.9) |
| Scleral tear | 35(10.5) |
| Corneal FB | 20(6.0) |
| Sub-conjunctival haemorrhage | 20(6.0) |
| Others | 35(10.5) |
In most of the patients, more than three ocular structures were affected by trauma. Out of 335 patients, in 25 of them; corneal tear, anterior chamber abnormality, uveal prolapse and lens damage were observed.
Majority of patients (92.54%, n=310) who encountered ocular trauma were presented to Hawassa University, tertiary eye care center after six hours from time of trauma and 47.76% (160) of them presented to the hospital after three days from time of trauma (Fig. 4).

The reason for delayed presentation assumed that treatment in health centers is enough (34.33%) and the distance from referral hospital is (29.85%) (Table 5). But there was no variable associated with the time of presentation.
| The reason for delay | Frequency (%) |
|---|---|
| Assuming treatment in health center is enough | 115(34.3) |
| Distance from referral hospital | 100(29.9) |
| Shortage of money | 45(13.4) |
| Lack of awareness | 20(6.0) |
| Unavailability of transportation | 10(3.0) |
| Others | 30(9.0) |
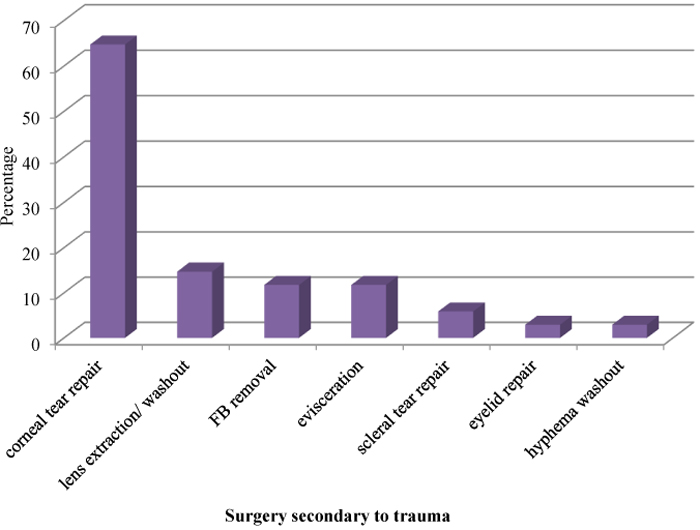
Most of the patients (95.52%) who presented for ocular trauma were intervened after 12 hours from the time of trauma. Only 1.49% of the total patients were treated immediately/ within 6 hours. Delayed presentation due to the distance from eye care center, lack of awareness and shortage of money were the common reasons for delayed intervention (76.12%). Ocular surgery secondary to trauma was performed in 50.8% (170) patients and among all; corneal tear repair was the most frequently performed surgery (64.7%), followed by crystalline lens extraction/ lens fragment washout (14.70%) (Fig. 5). Surgery, secondary to trauma, was associated with open globe injury (P = 0.006, AOR = 25.67)
The presentation VA was 6/6 only for 4.48% (15) patients and it was under blindness category (VA<3/60) for 59.71% (200) patients. At first day, after treatment, the VA was 6/6 only for 7.46% (25) patients and it was under blindness category (VA<3/60) for 47.76% (160) patients.
4. DISCUSSION
The result showed that the occurrence of ocular trauma is high in males (73.1%) and this is supported by other studies conducted around the globe; in Peshawar, Pakistan males accounted 80%, in Lahore, Pakistan-75%, in Nepal-69.3%, in Uttarakhand, India, male to female ratio-1.93:1 and in Grarbet, Ethiopia the male to female ratio was 3:1 [3, 5, 8-10]. This might be due to the reason that males are mainly engaged in outdoor activities where trauma will be highly encountered.
Among patients presented for ocular trauma, children (65.67%) followed by adolescents (25.37%) had accounted more than 80% and this is in agreement with other studies; Pakistan, <30 years old-69% (Peshawar), 18-29 years old-31% (Lahore); Kashmir valley, 16-26 years old-75% [8, 10, 13].
Majority of the patients reported for ocular trauma in this study were rural dwellers (76.12%) and similarly on the study conducted in western Nigeria, more than half (52.53%) patients were from rural area [1].
In this study, open globe injury has accounted 65.67% and closed globe injury was 32.84%. Closed globe injury is in line with the finding of Uttarakhand, India (31.9%) [6]. Penetrating globe injury was the highest finding among open globe injuries (43.28%) and this finding was reported as 12.1% in Nigeria [1]. Globe rupture of the present study is 2.99%, but in a study conducted in Egypt, it was found to be 31.4% [12].
In this study, corneal tear was the most frequently observed case (59.70) which is much higher as compared to a study done in western India (15.2%) [2]. Anterior chamber abnormality was 25.37% and this finding was higher in Pakistan; Jinnah (84%) and Peshawar (>50%) [8, 10]. In contrast, the findings were lower in Nigeria (5.9%) and western India (8.29%) [1, 2]. Uveal prolapse was 22.39% in this study, but it was 10% of all cases in Jinnah, Pakistan [8]. About 25% lens damage was observed in this study and the higher as well as the lower values were noticed in other studies [2, 8, 10]. The discrepancies might be due to the differences in the type of object that causes ocular trauma.
Only 1.49% patients were presented in the hospital within hour/ immediately, but in a study of Lahore, Pakistan, 23% of patients were reported within one hour after ocular trauma [8]. In a study conducted in Nigeria and Lahore, Pakistan, similar numbers of patients (38%) were presented for ocular trauma within 24 hours and in Uttarakhand, India 52.27% patients were reported within this time. But in our study, only 19.4% patients were presented within 24 hours [1, 3, 8]. From 1st to 7th days, 41.79% patients were reported for ocular trauma in this study, but in Nigeria, 32.5% patients and in Uttarakhand, India, 12.7% patients were reported in the same period [1, 6]. After 7 days, 23.8% patients were presented for ocular trauma and in this time 6%, 12.7%, 29.5% and 63.61% patients were reported in Egypt, India, Nigeria and Pakistan, respectively [1, 6, 10, 12]. The variations in presentation time might be due to the differences in distance from eye care center, poverty, awareness and transportation system across the countries.
From 335 patients visited the hospital for ocular trauma, 95.52% of them reported availability of health facilities around their area, but 79.69% of these facilities were not providing eye care service. And hence, 71.64% of patients travelled > 100 kilometers to get eye care service in Hawassa University, Referral Hospital. Also, 19.40% of patients have crossed 20-100 kilometers for Hawassa, but only 8.96% patients were from < 20 kilometers. On contrary to this, the majority of patients were from nearby in other studies; in Nigeria, 61.4% patients were from <20 kilometers, 21.2% patients were from 20-50 kilometers, 12.95 patients were from 50-100 kilometers and 4.5% patients were from >100 kilometers, in Grarbet, Ethiopia, 44.4% patients were from < 20 kilometers and 55.6% patients were from > 20 kilometers [1, 5]. This might be due to the variations in availability of eye care centers/ specialized eye care centers around.
The common cause of ocular trauma in this study was wood/ stick (47.76%), but in other studies road traffic accident (western India-38%, Uttarakhand, India-32.7% and 26.66%) and stone (Kashmir valley-48.3%) were the main causes of ocular trauma [2, 3, 6, 13].
At presentation, 4.48% patients were with VA of 6/6 and 59.71% were with VA of <3/60 in our study. Similarly, in a study conducted in Uttarakhand, India 56.5% patients were presented with VA of <3/60 [6]. Many of our patients have missed post intervention follow ups and due to this post intervention visual outcome could not be analyzed.
CONCLUSION
The ocular trauma was high in males, children, rural dwellers and low-income families and the common object that causes the trauma was wood/ stick. Most of the patients (>90%) presented after 6 hours from time of ocular trauma and the treatment was commenced also after 6 hours in >95% of them. Most of the patients (>70%) were from a distance of >100 kilometers from hospital. The cornea was the most commonly affected ocular structure by trauma.
Among variables entered into multivariate logistic regression; surgery, secondary to trauma, was associated with open globe injury (P = 0.006, AOR = 25.67). Assault trauma was also associated with open globe injury (P = 0.021, AOR = 43.17).
CONSENT FOR PUBLICATION
A written informed consent and assent was obtained from all patients when they were enrolled.
CONFLICT OF INTEREST
The study was sponsored by Orbis International-Ethiopia and authors declare no conflict of interests in this work.
ACKNOWLEDGEMENTS
We would like to express our heartfelt gratitude to Zelalem Mekonnen, Orbis project coordinator at Hawassa University, for her unreserved support. Also, we want to extend our appreciation to Orbis International-Ethiopia for its financial support and we would like to express our great thanks to the department of ophthalmology and optometry colleagues for their help during research progress.
Authors' contributions: Kindie Desta has made substantial contribution to performing research/study, analyzing the data and writing the paper; Samson Tesfaye has been involved in analyzing the data and fund acquisition; Bekalu Getahun has been involved in original draft preparation and writing the paper; Demoze Delelegn has made substantial contribution to designing the research and analyzing the data.


