CASE REPORT
Use of Radiofrequency Diathermy for the Treatment of Chronic Corneal Neovascularization with Lipid Keratopathy
George D. Kymionis1, *, Nafsika Voulgari1, Michael A. Grentzelos1, Konstantinos Aliferis1, Kate Hashemi1, Dimitrios Mikropoulos2
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 65
Last Page: 67
Publisher ID: TOOPHTJ-13-65
DOI: 10.2174/1874364101913010065
Article History:
Received Date: 12/05/2019Revision Received Date: 5/8/2019
Acceptance Date: 23/09/2019
Electronic publication date: 15/11/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose:
To present the use of radiofrequency diathermy for the management of chronic resistant corneal neovascularization with lipid keratopathy.
Methods:
Two post keratitis patients with chronic corneal neovascularization and lipid keratopathy refractory to conventional treatment underwent radiofrequency diathermy. (Klöti, Oertli ®, Switzerland) on an outpatient basis under topical anesthesia at the slit lamp biomicroscope.
Results:
No intra- or postoperative complications were encountered. After the procedure, significant regression of neovascularization with decrease in lipid deposition and improvement in corneal opacification was observed in both patients during the 12-month follow-up. Corrected distance visual acuity improved from 20/200 preoperatively to 20/80 postoperatively in the first case while remained stable at 20/20 in the second case. Significant symptomatic improvement regarding photophobia and discomfort was noted in both patients.
Conclusions:
Radiofrequency diathermy seems to represent an effective and safe minimally invasive treatment for chronic resistant corneal neovascularization with lipid keratopathy.
1. INTRODUCTION
Pathophysiological mechanisms of neovascularization include an imbalance between pro and anti-angiogenic factors. Many antiangiogenic and angioregressive therapeutic modalities have been proposed with variable results. [1] Currently, there is no consensus on the most effective approach, especially in the treatment of established mature corneal vessels.
Radiofrequency diathermy was originally described by Klöti et al. for infantile cataract surgery capsulorrhexis [2]. This surgical micro-instrument coagulates and cuts the anterior capsule in a precise manner using a platinum tip heated at approximately 160°C by a high-frequency current of 500 kHz [3]. We evaluated the safety and efficacy of radiofrequency diathermy in two patients with chronic resistant corneal neovascularization and lipid keratopathy.
2. CASE REPORT
2.1. Case 1
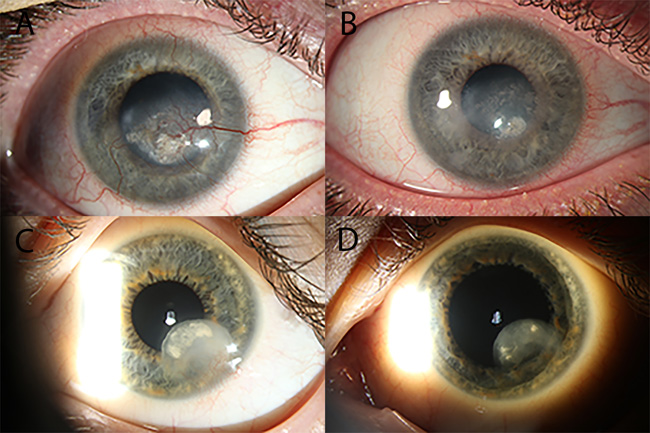
A 25-year-old male was referred to our institute for the management of persistent corneal neovascularization due to recurrent herpes simplex viral keratitis (HSK) in his right eye. His past ocular and medical history were otherwise unremarkable, and he did not take any medications. The patient was followed by his ophthalmologist since the age of 11-years-old for HSK for which he had received topical steroids without effect on the progression of the corneal opacification. Prior to the presentation, he had undergone two Argon laser sessions in a period of 6 months followed by topical steroid treatment gradually tapered over 2 months with recurrence of corneal neovascularization. Due to resistance to conventional treat- ment, we decided to apply a new therapeutic approach for the management of corneal neovascularization with accompanying lipid keratopathy by radiofrequency diathermy. At that time, Corrected Distance Visual Acuity (CDVA) was 20/200. The patient complained of ocular discomfort and photophobia. Slit-lamp examination showed central stromal scarring and lipid keratopathy with associated feeder vessels (Fig. 1A). Fundus examination was within normal limits.
2.2. Surgical Procedure
The procedure was performed by a senior cornea specialist (GK) on an outpatient basis using a slit lamp biomicroscope. The Klöti (Oertli ®, Switzerland) bipolar unit for capsulotomy, hemostasis, endodiathermy and coaptation was used. It was set to the capsulotomy mode to 4-6 W.
After administration of topical anesthesia with propara- caine HCL 0.5% eye drops (Alcaine; Alcon Laboratories Inc, Fort Worth, TX, USA), the standard capsulotomy tip was brought into contact with the corneal neovessel at 1 mm from the limbus and radiofrequency diathermy was applied until occlusion of the vessel was obtained. When applied on cornea, the curved shape of the diathermy tip provides a less than 500 μm protrusion, which serves as a safety barrier to avoid corneal perforation. After obstruction of the blood flow was confirmed, the application was repeated to the neighbor feeder vessels individually. Following the procedure, a compressive patch was applied on the eye for one day. Medication consisted of moxifloxacin (Vigamox, Alcon Laboratories, Inc) four times per day for one week and dexamethasone 0.1% (Dexafree, Thea Laboratories, Inc.) four times per day gradually tapered over two weeks.
Cauterization was first successfully applied on October 2017 with occlusion of the main feeder vessels. Retreatment was required two weeks after the procedure due to recanalization, followed by another cauterization session at 1-month due to opening of collateral vessels. The procedure was uneventful. There was no corneal haemorrhage, corneal perforation, burn at the site of diathermy or recurrence of herpetic keratitis. Monthly visits thereafter showed continuous regression of neovascularization and lipid deposition. No recurrence of corneal neovascularization was observed after the 3rd treatment session and during the one-year follow-up period. (Fig. 1B) CDVA improved to 20/80 with subjective sympto- matic improvement as to ocular discomfort and photophobia since the first-month post-treatment.
2.3. Case 2
A 29-year-old female was referred to our Institute for the evaluation of her left eye one year after keratitis due to pseudomonas aeruginosa. Her past ocular and medical history were otherwise unremarkable, and she did not take any medications. At the time of referral, CDVA was 20/20 and slit-lamp examination revealed corneal neovascularization associated with peripheral stromal scarring and lipid keratopathy (Fig. 1C). Fundus examination was without particularities. The patient had been unsuccessfully treated with topical steroids over a period of 12 months. The application of radiofrequency diathermy was chosen for the management of corneal neovascularization.
2.4. Surgical Procedure
The procedure was performed as described above.
Cauterization was applied on the feeder vessels and repeated after 1 week due to incomplete obstruction of blood flow. No complications such as corneal hemorrhage, perforation or burn were encountered, and the procedure was well tolerated by the patient. Follow-up examinations on day 1, week 1, 1st month, 3 months, 5 months, 8 months and 1st year showed gradual resolution of lipid deposits and corneal opacification since the first week, whereas no recurrence of corneal neovascularization was observed after the 2nd treatment session. (Fig 1D) Visual acuity remained stable at 20/20. The patient noted a subjective improvement in photophobia and ocular comfort since the first-week post-diathermy.
3. DISCUSSION
Corneal neovascularization involves a complex pathophy- siological process related to a dysregulation of pro-angiogenic and anti-angiogenic agents that normally preserve avascularity and transparency of the cornea [1]. Topical nonsteroidal and corticosteroid medications, anti-vascular endothelial growth factors (anti-VEGFs), topical immunomodulators such as cyclosporine, argon laser photocoagulation, photodynamic therapy (PDT), cautery and fine-needle diathermy have been advocated for the management of neovascularization [1].
As regards established mature neovessels, therapeutic options are limited, and insults such as chemical burn, trauma and infectious keratitis may result in significant corneal opacification or in the case of cornea transplantation, may jeopardize graft survival. Topical steroids appear to have limited angioregressive effect on established vessels [4]. Anti-VEGF treatment, although useful in newly forming vessels, seems ineffective in mature chronic vessels [5] Argon laser photocoagulation has been successful for obliteration of mature vessels, however it is unsuccessful for deep vessels or extensive corneal neovascularization and may be associated with corneal endothelial injury, lens damage, corneal hemorrhage or iris atrophy due to the high laser energy required [6]. PDT has been reported effective in lymphatic vessels regression, but its limited availability restricts the application of this approach [7]. Moreover, fine needle diathermy was found effective in occluding established vessels, but its limited reproducibility and potential adverse events, such as corneal micro-perforation, intracorneal hemorrhage and opacification, discourage its routine use [8].
The need for an effective, affordable and safe treatment for chronic corneal neovascularization prompted us to evaluate the efficacy and safety of high-frequency diathermy. In our cases, application of radiofrequency diathermy on corneal neovessels using Klöti (Oertli ®, Switzerland) resulted in significant regression of neovascularization from the first postoperative months and without any sign of recurrence during the 12-month follow-up. Moreover, a significant reduction in lipid deposition and clearing of corneal opacification were observed at 12 months postoperatively with improvement in visual function and ocular comfort in both patients. No intra- or postoperative complications were encountered in any of the cases during the follow-up period. The procedure was well tolerated on an outpatient basis. No case of corneal haemorrhage, corneal perforation, burn at the site of diathermy or recurrence of herpetic keratitis was observed. Although the underlying mechanism is not fully understood, it seems that obliterating the feeder vessels halts further transport and deposition of lipids while the remaining may gradually resolve through efflux [9].
To the best of our knowledge, these two cases are the first on the use of radiofrequency diathermy for the treatment of resistant corneal neovascularization associated with lipid keratopathy. This minimally invasive procedure seems effective and safe for the management of these cases with encouraging results. A large case series with longer follow-up is required to thoroughly evaluate this innovative treatment.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from all the participants prior to publication.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.