All published articles of this journal are available on ScienceDirect.
Atypical Christmas Eye Disease: A Case Report and Literature Review
Abstract
Background:
Christmas Eye Disease (CED), also known as the “Albury-Wodonga syndrome” or “Harvester's Keratitis”, is a seasonal acute corneal ulceration syndrome, which is geographically limited to Australia, specifically in the south-west region of New South Wales (NSW) and north-east region of Victoria. The mechanism of injury is unknown, but the secretions from native beetles of the genus Orthoperus have been implicated. There remains a dearth of literature on CED, particularly with atypical disease presentations. We present the first reported case of CED in the upper Blue Mountains Region, presenting atypically with mild pain and foreign body sensation. We also aim to explore the possible entomological precipitants of the disease.
Case Presentation:
A 77-year-old man with a 1-day history of a mildly painful red eye was found to have acute corneal ulceration. He experienced mild discomfort in his right eye while asleep and woke the following morning with persistent blur, foreign body sensation, and photophobia. He had no history of ocular trauma or chemical exposure. He reported going for daily bushwalks in the upper Blue Mountains region but did not recall any exposure to environmental or entomological precipitants.
Clinical Findings and Outcomes:
Slit-lamp examination revealed a substantial corneal epithelial loss in the right eye with fluorescein staining, revealing a characteristic ‘green splash’ over 90% of the cornea. Other clinical findings included marked corneal edema, moderate conjunctival injection, mild palpebral swelling, and mild papillae. No anterior uveitis was observed, and the posterior segment examination was normal. There was a considerable reduction in his right visual acuity from baseline. He was empirically treated with 1% tropicamide ocular drops, 1% chloramphenicol ointment, and lubricant ocular drops. The bacterial and viral conjunctival swabs were unremarkable. Clinical progression was self-limiting, and complete resolution of the ulcer was achieved after one month.
Conclusion:
CED is a clinical diagnosis, and medical practitioners should be aware of atypical features, such as the absence of debilitating pain. Additionally, our case demonstrates that the geographic distribution of CED appears to be far more extensive than previously thought, thereby raising the possibility of disease manifestation in regions not commonly associated with it. Entomological precipitants of this condition remain circumstantial and warrant further validation.
1. INTRODUCTION
Christmas Eye Disease (CED), also known as the “Albury-Wodonga syndrome” or “Harvester's Keratitis”, is a seasonal acute corneal ulceration syndrome, which is geographically limited to Australia, specifically in the south-west region of New South Wales (NSW) and north-east region of Victoria [1-3]. First described in 1974 by Walker, this syndrome of acute corneal ulceration was called “Christmas Eye” due to its peak incidence in southern hemisphere summer, i.e., between mid-December and mid-February [1]. CED is classically a monocular ailment characterised by debilitating pain and a large but shallow uniform ulcer, frequently covering over 70% of the corneal surface. Common clinical features include severe ocular pain, palpebral swelling, conjunctival injection, epiphora, photophobia and decreased visual acuity [1-4]. Patients are typically woken by severe pain in the early hours of the morning, having been outdoors amongst vegetation (e.g., hay, grass, leaves) around dusk or sunset the previous day [1, 3]. The mechanism of injury is unknown, but the secretions from native beetles of the genus Orthoperus have been implicated [1, 2]. We present the first reported case of CED in the upper Blue Mountains Region, presenting atypically with mild pain and foreign body sensation.
2. CASE PRESENTATION
A 77-year-old man presented to our clinic with a 1-day history of mildly painful red eye. He was referred from a local emergency department with an acute corneal ulcer. He had fallen asleep while watching television the preceding evening and was occasionally woken by mild pain in his right eye. The following morning, he developed redness and foreign body sensation in his right eye with associated blur, photophobia, and upper palpebral swelling. He had no significant ophthalmic history, such as Recurrent Corneal Erosion Syndrome (RCES), herpetic corneal ulcers, corneal dystrophies, or diabetic retinopathy. He did report any ocular trauma or chemical exposure, particularly to alkaline or acidic substances. No other visual or systemic symptoms were reported. Co-morbidities included well-controlled type 2 diabetes mellitus with no known vascular or neuropathic complications, hypertension, and hypercholesterolemia. His medications included dapagliflozin, metformin, gliclazide, lisinopril, simvastatin, and aspirin. Although he did not recall any insect bites, he mentioned going for daily morning bushwalks, including on the day before his symptom manifestation.
The right visual acuity was reduced to 6/18–1 with no improvement with pinholes. His left visual acuity was 6/9 and 6/6, with pinholes. His baseline right visual acuity was 6/6 without correction, as per the records from four years earlier. Intraocular Pressure (IOP) measurements and ocular motility tests were normal. His visual field was normal with confrontation testing. Bilateral corneal reflex testing was normal, indicating intact trigeminal nerves. There was a moderate conjunctival injection, mild palpebral swelling, mild conjunctival papillae, and substantial corneal epithelial loss in the right eye with fluorescein staining, revealing a characteristic ‘green splash’ over 90% of the cornea (Fig. 1). There was also marked corneal edema with Descemet’s folds. There were no corneal epithelial microcysts or epithelial ‘sloughing’ to suggest underlying RCES. Seidel’s test was negative. The anterior chamber was deep and quiet, with no iris abnormalities. The pupils were normal, with no relative afferent pupillary defects or anisocoria. There were no ocular foreign bodies, including sub-tarsal or intraocular debris. There were no other clinical signs to suggest globe rupture or penetrating ocular injury. Bilateral fundus examination results were normal. There was no regional lymphadenopathy or involvement of the contralateral eye. The bacterial and viral conjunctival swabs were unremarkable.
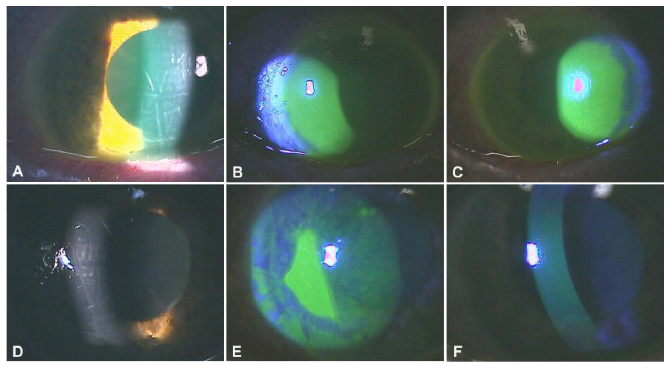
(A) Descemet’s membrane folds due to extensive corneal edema on Day 1. (B) and (C) “Green splash of paint” ulcer covering over 90% of right corneal surface on Day 1. (D) Mild improvement in corneal odema and Descemet's membrane folds on Day 5. (E) Reduction in size of corneal ulcer by about 75% on Day 5 with diffuse punctate epithelial erosions (PEE). (F) Minimal-moderate PEE on Day 14.
Initial treatment comprised twice daily topical 1% tropicamide and four times-a-day topical 1% chloramphenicol ointment. A combination lubricant eye drop of 0.4% polyethylene glycol-400 and propylene 0.3% glycol was added on day 5. Follow-up appointments were organised every 48 h for the first week and weekly until complete resolution of the ulcer was achieved. Twice daily 1% tropicamide was ceased after a week, and the four-times-a-day 1% chloramphenicol ointment was ceased after 2 weeks. There was a considerable reduction in the size of the ulcer (> 75%) after 1 week. Mild ocular ache, photophobia, foreign body sensation, and conjunctival congestion also resolved. Ulceration and visual acuity exhibited a protracted recovery, and normalised after a month. The clinical progression of his right acute corneal ulcer is shown in Table 1. A diagnosis of atypical Christmas Eye Disease (CED) was established, considering the history of presenting complaint, characteristic “green splash” ulceration, self-limiting clinical progression of the ulceration, absence of debilitating ocular pain, and atypical geographic incidence. Informed consent was obtained from our patient for the purpose of publication.
3. DISCUSSION
Christmas Eye Disease (CED) has no known aetiology and exhibits certain characteristic features which allow for a clinical diagnosis. It is a recognised seasonal syndrome within the communities of Albury-Wodonga and Canberra. Although epidemiological data on the disease remain limited, one report indicated over 227 cases of CED in rural southeastern Australia between October 1992 and February 1993 [5]. The typical occurrence of CED, as illustrated in Fig. (2), appears to be limited by the Great Dividing (Mountain) Range to the east and south, to the west by a line connecting Corowa, Wagga Wagga, and Young [1, 5], and to the north by towns as far as Gulgong and Mudgee (G Barker & C Borg, 2021, personal communication, 22nd July). Cases have also been uncommonly reported in Adelaide and Northern Tasmania [4, 5]. As the name implies, CED tends to manifest during the southern hemisphere summer months when the climate is hot and dry, with peak incidences in December and January [1, 3].

| - | Right VA | Right IOP | The Appearance of Cornea Under Fluorescein Stain | AC | On-going Treatment |
|---|---|---|---|---|---|
| Day 1 | 6/18-1 ph NI | 18 |
 Ulcer involving over 90% of the right corneal area. 3+ diffuse corneal odema. 5/10 mild ache with significant Ulcer involving over 90% of the right corneal area. 3+ diffuse corneal odema. 5/10 mild ache with significantforeign body sensation. Normal epithelium, stroma, endothelium, and tear film in left. eye. |
d+q | 1. Tropicamide 1% eye drops BD 2. Chloramphenicol 1% ointment QID |
| Day 3 | 6/24+1 ph NI | 16 |
 Reduction in size of ulcer by 25% with associated PEE. 2+ diffuse corneal odema. Normal epithelium, stroma, Reduction in size of ulcer by 25% with associated PEE. 2+ diffuse corneal odema. Normal epithelium, stroma,endothelium, and tear film in the left eye. |
d+q | 1. Tropicamide 1% BD 2. Chloramphenicol 1% ointment QID |
| Day 5 | 6/24-1 ph NI | 16 |
 Ulcer 75% smaller as compared to the size Ulcer 75% smaller as compared to the sizeon Day 1. Ulcer coverage about 20% of the right cornea. Diffuse PEE over the remainder of the cornea. 3/10 ache with mild foreign body sensation. Normal epithelium, stroma, endothelium, and tear film in the left eye. |
d+q | 1. Tropicamide 1% BD 2. Chloramphenicol 1% ointment QID 3. Polyethylene glycol-400 0.4% + propylene glycol 0.3% eye drops BD |
| Day 7 | 6/24+1 ph NI | 11 |
 A few small, scattered ulcers with diffuse PEE. No pain or FBS. Normal epithelium, stroma, endothelium, and tear film A few small, scattered ulcers with diffuse PEE. No pain or FBS. Normal epithelium, stroma, endothelium, and tear filmin the left eye. |
d+q | 1. Chloramphenicol 1% ointment QID 2. Polyethylene glycol-400 0.4% + propylene glycol 0.3% eye drops BD |
| Day 14 | 6/18 ph 6/9 | 12 | Minimal-moderate PEE in right eye. No pain or FBS. Normal epithelium, stroma, endothelium, and tear film in the left eye. | d+q | 1. No eye treatment |
| Day 26 | 6/9 ph 6/6-3 | 12 | Normal epithelium, stroma, endothelium, and tear film in both eyes. | d+q | 1. No eye treatment |
The dominating feature of CED is debilitating unilateral ocular pain, with the tell-tale look of ‘abject misery’ and clutching of the inflicted eye [1, 3-5]. The pain often requires heavy doses of narcotics and only ceases upon regeneration of the corneal epithelium, which often takes 48-72 hours [1-3, 6]. The associated photophobia and blur can persist for 2-4 weeks [3, 6]. The history typically involves the patient being outdoors, dealing with vegetation (e.g., grass, hay, leaves) around sunset, and waking up with severe eye pain in the early hours of the next morning [1-3]. CED is also known as ‘Harvester’s Keratitis’ in certain rural parts due to its significant occupational association with harvesting activities in the summer months [1, 3]. Slit-lamp examination with fluorescein usually reveals shallow ulceration involving most of the corneal surface without signs of uveitis [1, 3, 4]. The condition is often self-limiting and complete resolution of symptoms may take up to 6 weeks [1, 3]. Long-term complications, such as corneal scarring and vision loss, though rare, have been reported [3]. There has been no clustering of cases to suggest person-to-person transmission [5].
Although the pathophysiology of CED remains obscure, the secretions of native beetles belonging to the genus Orthoperus have been implicated. Walker first described the isolation of a beetle of the Orthoperus species (Family Corylophidae) in a female patient with CED [1, 7]. Orthoperus beetles tend to swarm in the evenings and are found in the flora of the south-west region of NSW and the north-east region of Victoria. This coincides with the clinical history provided by the majority of patients who reported being outdoors, several hours before symptom onset [1-3, 7]. Walker proposed that the delayed pain, hours after presumed exposure to the beetle, is likely due to an auto-catalytic reaction culminating in epithelial cell loss and ulceration. He also suggested that the reaction could have been exacerbated by rapid eye movements or rubbing during sleep, resulting in patients waking with severe pain [1].
The delay in the onset of symptoms suggests a resemblance to the effects of paederin, a well-documented toxin released by a different species of beetle. Paederus beetles (Family Staphylinidae) are known to cause keratitis and iritis through the release of paederin, a potent vesicating amide generated by the endosymbiotic bacterium Pseudomonas. Paederin inhibits protein and DNA synthesis, resulting in inflammation and possible secondary infection [8-11]. Although no laboratory analysis of corneal scrapings or anterior chamber paracentesis was performed, our patient’s ocular swabs were negative for pathogens, including Pseudomonas species. Unlike the self-limiting nature of CED, Paederin-induced keratitis can cause long-term visual acuity deficits and sometimes require treatment with penetrating keratoplasty [8]. Paederus beetles are also known to cause a relatively milder seasonal acute keratoconjunctivitis and periocular dermatitis in Africa, aptly called “Nairobi Eye” [9-13]. Though animal experiments involving ocular exposure to Orthoperus beetle extracts were largely unsuccessful in replicating the corneal ulcers observed in CED, one notable experiment produced the characteristic ulcer in one of five rabbits [1, 11]. However, the postulated chemical irritant from Orthoperus beetles remains unknown, and the association between CED and these beetles remains circumstantial.
The mainstay of CED treatment is pain management, which is often refractory. Topical anaesthetics provide significant but transient pain relief and should be used with caution [1, 3]. Overuse of topical anaesthetics, even at low concentrations, has been shown to delay corneal healing and precipitate persistent epithelial defects, endothelial damage, and peripheral anterior synechiae formation [14]. Topical anaesthetics could also mask worsening symptoms and delay the diagnosis of other potentially sight-threatening conditions, such as bacterial keratitis [14]. Non-steroidal anti-inflammatory eye drops can also be used to treat ocular pain in CED patients. Howsam demonstrated considerable pain relief using hourly topical application of 1% indomethacin, but the evidence is limited by the small sample size [3]. There is no evidence for the role of antibiotics or steroids in improving clinical or pain outcomes. CED patients with intractable pain are often hospitalised and treated with parenteral analgesia [3, 4]. Given the lack of significant pain, our patient did not require any pain relief. His treatment included only 1% tropicamide ocular drops, 1% chloramphenicol ointment, and lubricant ocular drops. Traditionally, topical cycloplegics and mydriatics, such as tropicamide, have been used in large corneal ulcers to relieve pain from ciliary spasm; however, evidence for its use in uncomplicated corneal abrasions is inconsistent [2, 15-17]. Given the ambiguous nature of his presentation, chloramphenicol, a broad-spectrum antibiotic, was commenced prophylactically to treat bacterial infections.
Although the characteristic initial “green splash” corneal ulceration and the overall duration of ulcer and symptom resolution correspond with typical CED progression, our case has three atypical features. This is the first documented case of CED in the upper Blue Mountains region, where the climate is considerably cooler, a stark contrast to the hot and dry climate traditionally associated with the distribution of CED in the southwest region of NSW and northeast region of Victoria. The occurrence of CED in the town of Blackheath also questions the conventional understanding of the disease distribution, where areas part of and east of the Great Dividing Range were thought to be free of the condition [5]. The absence of severe pain in CED is also atypical, with only a handful of documented CED cases known to manifest with mild pain [1]. Most CED patients are noted to be outdoors in the late evenings and are woken by severe pain in the early hours of the morning. Atypically, our patient was in the Blackheath bushwalking trails in the morning and only woke up occasionally during the night due to mild discomfort. This timing variance may indicate possible exposure to different entomological or environmental precipitants.
Being outdoors among the vegetation is a lifestyle feature strongly associated with CED and possible exposure to Orthoperus beetles [1-3]. However, according to data from the Atlas of Living Australia (ALA), there have been no documented or confirmed sightings of Orthoperus beetles in the Blue Mountains region [18]. Interestingly, Paederus beetles are native to the Blue Mountains region and are known to be active during the day [11, 19]. Although not typically linked with CED manifestation, exposure to paederin toxin remains an aetiologic possibility given that contact with these small (2-8 mm) beetles may have gone unnoticed by the patient [7]. Paederin-induced ocular complications are often a result of transferring the toxin of crushed beetles by finger to the eyes [9, 12]. Our patient could have also been exposed to other vesicant-toxin-producing beetle varieties known to cause transient ocular irritation, such as Meloidae (true blister beetles) and Oedemeridae (false blister beetles), both of which are native to the Blue Mountains region [20, 21]. Both Meloidae and Oedemeridae beetles contain cantharidin, a terpenoid toxin that causes chemical burns to the skin and ocular tissues [9-11]. The onset of action is similar to Paederin, with symptoms occurring within 12-14 hours of exposure and are often self-limiting with conservative management [9]. Apart from the proposed entomological causes, an unidentified non-entomological environmental trigger remains a possibility, underlying the need for further research to validate the pathogenesis of CED.
CONCLUSION
CED is a clinical diagnosis, and medical practitioners should be aware of atypical features, such as the absence of debilitating pain. Additionally, our case demonstrates that the geographic distribution of CED appears to be more extensive than previously thought. The self-limiting and benign natural history of the condition may mean that cases are under-reported, and the existing literature may not reflect the true geographical extent of the disease distribution. Therefore, one should be aware of the possibility of CED in regions not commonly associated with it. Entomological precipitants of this condition remain circumstantial and warrant further validation.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained.
STANDARDS OF REPORTING
CARE guidelines have been followed in this study.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
FUNDING
None.
ACKNOWLEDGEMENTS
The authors thank Professor Richard C. Russell, Director of the Department of Medical Entomology at Westmead Hospital, for providing guidance and information on the beetle species implicated in CED, and Mr. Ciaran Mathewson, from the Australian Museum, for facilitating access to the Atlas of Living Australia (ALA). We would also like to extend our special thanks to optometrists, Mr. Glen Barker (George & Matilda Eyecare) and Ms. Corrine Borg (Mudgee Eyecare), for providing information on their local CED cases in Gulgong, Mudgee, and Bathurst.


