RESEARCH ARTICLE
Efficacy of Smartphone-based Fundus Photo in Vision Threatening Diabetic Retinopathy Screening: Developing Country Perspective
Mia Nursalamah1, Feti Karfiati1, 2, Nina Ratnaningsih1, 2, Sri Hudaya Widihastha1, *
Article Information
Identifiers and Pagination:
Year: 2024Volume: 18
E-location ID: e18743641281527
Publisher ID: e18743641281527
DOI: 10.2174/0118743641281527240116095349
Article History:
Received Date: 28/09/2023Revision Received Date: 01/12/2023
Acceptance Date: 06/12/2023
Electronic publication date: 19/01/2024
Collection year: 2024

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background
Vision-threatening diabetic retinopathy (VTDR) is a microvascular retinal complication caused by diabetes mellitus, which may lead to blindness if left untreated. One of the most effective methods to prevent diabetic-related ocular complications is through diabetic retinopathy (DR) screening. The community rarely carries out diabetic retinopathy-related eye examinations because using non-portable fundus photographs as its gold standard is costly and impracticable. This study aimed to determine the accuracy of smartphone-based fundus photographs as a practical and affordable tool for VTDR screening in developing countries.
Methods
This cross-sectional study used a consecutive technique at Cicendo National Eye Hospital, Indonesia. Patients with diabetes mellitus aged ≥20 years were evaluated for two-field mydriatic fundus photos using a non-portable fundus photo and a smartphone- based fundus photo utilizing the i-Spot fundus adapter. Results were analyzed to determine diagnostic test parameters.
Results
Two hundred and nineteen two-field mydriatic fundus photos were obtained from 139 patients. Smartphone-based fundus photography demonstrated a sensitivity of 98.4% (CI 96.6–100%), a specificity of 87.1% (CI 75.3–98.9%), a positive predictive value of 97.9% (CI 95.9–99.9%), a negative predictive value of 90.0% (CI 79.3–100%), and an accuracy of 96.8% (CI 94.5–99.8%).
Conclusion
The use of smartphone-captured fundus images proves to be a reliable screening method for VTDR. This tool has the potential to effectively screen the population, helping prevent future visual loss attributed to the disease.
1. INTRODUCTION
Vision-Threatening Diabetic Retinopathy (VTDR) is a microvascular condition of the retina that causes blindness in people with diabetes mellitus. The global prevalence of diabetic retinopathy (DR) is 34.6%, with VTDR at 10.2%. Bilateral blindness is found in 4% and 7.7% of people with DR and VTDR, respectively. After cataracts, glaucoma, and macular degeneration, DR is the fourth leading cause of blindness in Indonesia [1-3].
Early detection and appropriate management of VTDR patients can reduce the risk of blindness. The implementation of VTDR screening needs to be carried out massively and evenly in all primary health facilities by involving non-ophthalmologists. The DR screening program includes visual acuity testing and fundoscopy or digital retinal imaging. The fundus photograph with seven fields of view is the gold standard for DR inspection; however, it takes a long time, is inconvenient, and is costly. Since the early clinical indications of VTDR can be observed in the posterior pole (macular region and optic disc), detection of VTDR with a fundus picture of two fields of vision is deemed adequate [4-9].
The National Health Survey in the United Kingdom has set a minimum resolution of 6 megapixels, or 30 pixels per retinal degree, for retinal imaging instruments used in DR exams. With the advancement of smartphone camera technology, which now has a resolution of 5-64 megapixels, smartphone-based fundus photo exams may be performed more rapidly and affordably. Various investigations on smartphone-based fundus photographs in VTDR screening revealed varied sensitivity and specificity, ranging from 59–93% to 57–100%. Through telemedicine, this strategy attempts to improve the effectiveness and efficiency of the VTDR screening program in the community. This study will evaluate the accuracy of smartphone-based fundus picture assessment as a VTDR screening tool in developing countries settings.
2. METHODS
A cross-sectional diagnostic test study was conducted on patients who visited the PMN polyclinic at Cicendo Eye Hospital, Bandung, from December 2021 to April 2022. A sequential approach was used in selecting the research sample. Inclusion criteria comprised (1) diabetes patients aged more than 20 years old, (2) fundus images with mydriatic fields, and (3) photo quality grades 2 and 3 according to NHS UK guidelines. Technical and clinical problems were categorized as exclusion criteria, including lack of cooperation during examination, contraindications to mydriatics, pupil size less than 5 mm after mydriatic, and significant opacity of the refractive media. The drop-out criteria were fundus photos with low-quality photos or unreadable images. The Ethics Committee of Cicendo Eye Hospital granted ethical permission for this study, with registration number LB.02.01/2.3/042/2021.
Patients with diabetes who met the inclusion criteria were recorded in general data through analysis. Visual acuity, intraocular pressure, and anterior segment were examined, followed by the administration of mydriatic drops. A trained operator performed a non-portable fundus picture (NIDEK AFC-330, Japan) with two fields of view on the patient. The patient was next subjected to retinal imaging using a smartphone-based fundus photo (Samsung Galaxy M51, South Korea) with an i-Spot fundus adapter arm (Indonesia) and a 20 D lens (Volk Optical, USA), as seen in Fig. (1). On the same day, a resident ophthalmologist performed a smartphone-based fundus picture examination. Fundus pictures with VTDR and non-VTDR findings were displayed on a randomized computer for interpretation by a vitreoretinal ophthalmologist. The data are displayed in a 2x2 table, and statistical analysis was performed to derive diagnostic test parameters, such as sensitivity, specificity, positive predictive value, negative predictive value, and accuracy, using the SPSS version 24.0 application for Windows.
 |
Fig. (1).
Smartphone-based fundus photo with i-spot fundus extension arm and 20 D lens. Private Documentation by Aldiana Halim, 2021. |
| Characteristics | Amount (Percentage) |
|---|---|
| Age | N=139 |
| Mean±SD | 53,41±8,29 years |
| Range (min-max) | 25 – 73 years |
| - | - |
| Sex | - |
| Male | 47 (33,8%) |
| Female | 92 (66,2%) |
| - | - |
| Duration of DM | - |
| ≤5 years | 54 (38,8%) |
| 6-10 years | 44 (31,7%) |
| >10 years | 41 (29,5%) |
| - | - |
| Comorbid | - |
| Hypertension | 47 (33,8%) |
| Dyslipidemia | 14 (10,1%) |
| Hypertension and Dyslipidemia | 51 (36,7%) |
| None | 27 (19,4%) |
| Visual Acuity | N = 219 |
| ≥6/12 | 33 (15,1%) |
| <6/12-6/18 | 23 (10,5%) |
| <6/18-6/60 | 94 (42,9%) |
| <6/60-3/60 | 18 (8,2%) |
| <3/60 | 51 (23,3%) |
3. RESULTS
The overall sample size was 224 eyes from 142 patients; however, five eyes (2.2%) were included in the drop-out criteria, allowing 219 eyes (139 patients) to be studied in this study. The characteristics of the subjects are shown in Table 1.
The subjects in this research were 53 years old on average, with the female gender dominating by as much as 66.2%. Most individuals reported having DM for at least five years, with as many as 38.8% having concomitant hypertension and dyslipidemia. The biggest group in this research, 42.9%, was the visual acuity group 6/18–6/60, followed by the visual acuity group 3/60.
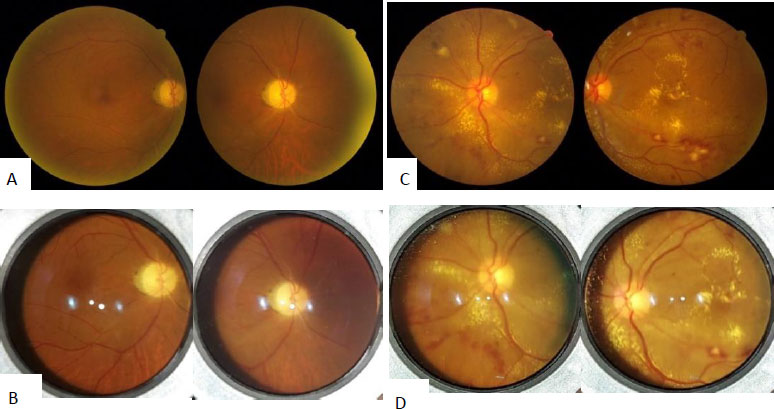
The interpretation result of retinal imaging using a smartphone-based fundus picture and a non-portable fundus photo group that was graded as VTDR was 185 eyes or 98.4%. Meanwhile, in the non-portable fundus photo group, 27 eyes (87.1%) were classified as non-VTDR on smartphone-based fundus images. The table that shows the proportion of smartphone-based and non-portable fundus photos is presented in Table 2. The example of a fundus photo is shown in Fig. (2).
The reading quality of smartphone-based fundus images was 97.1%. As many as seven fundus pictures with photo quality grade 1 that cannot be read were eliminated.
Table 3 shows numerous characteristics that influence the accuracy of smartphone-based fundal evaluation findings on non-portable fundal images. The sensitivity value of 98.4% shows a very high statistical sensitivity value with a CI of 96.6–100%, but the specificity value of 87.1% indicates a statistically substantial specificity value with a CI of 75.3–98.9%. As mentioned earlier, the positive predictive value (NDP) is 97.9%, suggesting a powerful NDP with a CI of 95.9–99.9%, whereas the negative predictive value (NDN) on this diagnostic test is 90.0% (CI 79.3–100%). With a CI of 94.5–99.1%, the accuracy rating of 96.8% shows a strong level of accuracy.
| - | Nonportable FP | Total | ||
|---|---|---|---|---|
| VTDR | Non-VTDR | |||
| Smartphone-based FP | VTDR | 185 (98,4%) | 4 (12,9%) | 189 (86,3%) |
| Non-VTDR | 3 (1,6%) | 27 (87,1%) | 30 (13,7%) | |
| Total | 188 (85,8%) | 31 (14,2%) | 219 | |
| Diagnostic Test Parameter | Value | 95% Confidence Interval (CI) |
|---|---|---|
| Sensitivity | 98,4% | 96,6 - 100 |
| Specificity | 87,1% | 75,3 - 98,9 |
| Positive Predictive Value | 97,9% | 95,9 - 99,9 |
| Negative Predictive Value | 90,0% | 79,3 - 100 |
| Accuracy | 96,8% | 94,5 - 99,1 |
4. DISCUSSION
Diabetic retinopathy screening in the community necessitates employing low-cost and simple-to-use methods. A screening instrument's sensitivity and specificity test findings are compared to the acknowledged gold standard to determine its efficacy. The British Diabetic Association (BDA) advises that a successful diabetic retinopathy screening method has sensitivity and specificity values of at least 80% and 95%, respectively. Smartphone-based fundus photos in this study have a high sensitivity value, but the specificity has yet to reach 95%. However, this study classified the sensitivity and specificity values as extremely strong and statistically significant [10-15].
Several studies on DR screening techniques have been conducted using various methods with differing degrees of accuracy. The smartphone-based fundus picture tool that is now being developed is either directly or indirectly in the form of a smartphone camera-based fundus photo. Indirect smartphone fundus images with a 20-D lens outperform direct smartphone fundus photos regarding photo quality and accuracy [16-19].
A meta-analysis study conducted by Tan et al. on the use of smartphones in detecting DR showed that smartphone ophthalmoscopes play a significant role in recognizing DR in places with restricted access. The sensitivity and specificity combined were 86.5% and 96.4%, respectively. The diversity was related to using various smartphone-based fundus photography equipment; most research employs direct smartphone ophthalmoscopes with an integrated camera and a smartphone adapter arm. In this study, the smartphone-based fundus picture tool is similar to indirect ophthalmoscopy, which employs a 20-D condensation lens and an i-Spot fundus adaptor. Compared to the more expensive direct smartphone ophthalmoscope, this indirect smartphone ophthalmoscope is regarded as more accessible, affordable, and practical for DR screening. As a result, the smartphone-based fundus picture in this investigation is more sensitive than Tan et al. [10, 11].
Wintergerst et al. also employed an indirect smartphone-based fundus picture method to detect VTDR. The validation value had a sensitivity of 76% (CI 66–85%) and a specificity of 76% (CI 97–100%). The standard reference of this study was the outcome of a clinical evaluation by two grading ophthalmologists utilizing direct and indirect ophthalmoscopy. The smartphone fundus picture was taken with video and performed by an optometrist who had just been trained for three days. According to the findings, smartphone-based fundus picture assessment can be assigned to non-expert operators [20-22].
Sengupta et al. obtained sensitivity and specificity values of 95% and 97% from two graders, respectively. The findings of this study are similar to those of Sengupta et al.; however, the tool employed is a Remidio FOP fundus picture with an integrated camera, a smartphone-based fundus photo, and a smart-scope, as opposed to a non-portable fundus photo of TOPCON with three fields of view. This study was undertaken in the same context as this study, which was carried out at a specialized tertiary eye hospital. However, the percentage of VTDR and non-VTDR cases collected was balanced since Sengupta et al. included patients without a history of DM in their study, as opposed to this analysis, which had only patients with a history of DM who visited Cicendo Eye Hospital. As a result, the proportion of VTDR and non-VTDR patients found in this study differed significantly [21].
The screening program is not a diagnostic test but a public health initiative. Diagnostic screening tests should have high sensitivity while having a somewhat lower specificity [17, 23].
The percentage of accurately recognized conditions in the screening test is referred to as sensitivity. If a screening test has a sensitivity of 90%, one out of every ten will be overlooked. A high-sensitivity test has the potential for screening since it seldom misses a diseased person. If the condition under investigation is fatal if left untreated and survival rates increase with immediate treatment, sensitivity is more crucial than specificity. As with VTDR diseases that, if not addressed promptly, might result in irreversible blindness, a more excellent sensitivity rating becomes more valuable [24-26].
Test kits with high specificity provide extremely few false-positive findings. As a result of its minimal false-positive error, a test with high specificity is helpful for diagnostic reasons. A poor specificity test has the drawback of screening many healthy patients as positive and subjecting them to unnecessary diagnostic or treatment procedures. The specificity value in this investigation was lower than the sensitivity, indicating that non-VTDR people might be recognized as VTDR and referred for additional ophthalmological evaluation. Given the condition of diabetic retinopathy, which requires routine tests to maintain adequate visual acuity, this is deemed manageable [23, 26].
The positive predictive value (NDP) of this study is 97.9%, indicating the possibility of someone suffering from VTDR if the diagnostic test result is positive, and the negative predictive value (NDN) is 90.0%, indicating the probability of someone not suffering from VTDR if the diagnostic test result is negative. Because the prevalence of a disease in the population examined has a considerable impact on the NDP and NDN values, these two parameters are more relevant for doctors in evaluating the morbidity of a group. In this study, the accuracy of 96.8% from the use of smartphone-based fundus images reveals that the percentage of this test tool identifies positive in VTDR patients and detects negative in non-VTDR patients exceptionally well [23].
The resolution of the camera in smartphone-based fundus images will determine their quality. Several prior studies utilized devices from Apple or Samsung. The difference in using these sorts of cell phones does not impede because they have met the minimum resolution criteria set by the NHS in the United Kingdom. The smartphone used in this study represents the average specifications of the new generation of smartphones and is more affordable from an economic standpoint. In principle, the higher the quality of the fundus images generated, the better the camera specification utilized. However, some studies found no statistically significant difference in picture quality between Apple and Samsung cellphones when employing fiberoptic flexible cystoscopy. The i-Spot may also be used with other smartphones as well with the main camera that is side by side with the flashlight as its specification [20].
The approach used to take fundus photographs can also impact the quality of the images acquired. The camera in non-portable fundus photos is fixed on the table at eye level with the eyes of patients and has a chin rest and headrest to stabilize the head of patients. Non-portable fundus photos also have a visual fixation target that can help the patient stabilize the eye position with a better camera for making precise, sharper, and more distinct pictures. Whereas there are no components of visual fixation or head position in smartphone-based fundus photographs, the location of the condensing lens and smartphone camera only rests on the arm of the examiner. It has the possibility of image focus instability, resulting in unsatisfactory images. An extra i-Spot fundus arm is used to aid in the alignment of the camera location, light source, and condensing lens, allowing non-ophthalmologists to use smartphone-based fundus photographs [10].
Several studies have demonstrated several methods of obtaining smartphone-based fundus pictures, including directly recording photos and videography, both of which are interpreted in the form of movies or screenshots of the video. The examiner utilized video in this investigation to take pictures, which were then screened from the film. The photograph is then evaluated and compared to the results of a non-portable fundus photograph. When compared to direct photo capture, steps like these might degrade the resolution of the resultant image [16-21].
Lighting artifacts in this smartphone-based fundus shot may contribute to the interpretation differences in the study. In this study, only 7 (2.9%) of smartphone-based fundus photos were released due to the first degree of image quality. Moreover, in this study, 97.1% of fundus images taken with a smartphone could be graded or had sufficient photo quality, in contrast to the study conducted by Tan et al., which found that 79.5% of eyes could be graded using smartphone ophthalmoscopy [10].
The limitation of this study is that the main emphasis is on the smartphone-based fundus picture tool; however, it falls short of providing a thorough comparison with conventional methods of diabetic retinopathy (DR) screening. However, this study has shown sensitivity and specificity as a reference to consider this tool as a screening tool. Secondly, the number of unbalanced proportions of VTDR and non-VTDR patients is a drawback of this study since it was done in a tertiary eye hospital that serves as a national referral center; thus, the number of non-VTDR cases acquired was limited. This condition may not accurately reflect the state of DR screening in the community, as non-VTDR disorders are expected to be more prevalent. As a result, when tested on the general public in primary health care, the specificity value of this smartphone-based fundus picture may be higher.
CONCLUSION
Smartphone-based fundus photos of two mydriatic fields have good accuracy in screening for vision-threatening diabetic retinopathy in developing country settings. Smartphone-based fundus picture tools can be utilized in the community for VTDR screening. Moreover, further studies might be undertaken with a bigger sample size, community-based, and involving non-ophthalmologists.
LIST OF ABBREVIATIONS
| DM | = Diabetes Mellitus |
| DR | = Diabetic Retinopathy |
| VTDR | = Vision-threatening Diabetic Retinopathy |
| D | = Diopter |
| NHS | = National Health Service |
| CI | = Confidence Interval |
| PPV | = Positive Predictive Value |
| NPV | = Negative Predictive Value |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study involving human subjects was conducted with the approval of the Ethical Commitee at Cicendo Eye Hospital. The approval number for this study is LB.02.01/2.3/042/2021.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all adult participants involved in this study. These consents include permission for the publication of study findings while maintaining the anonymity and confidentiality of the participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
In memoriam, we express our deepest appreciation to the late Aldiana Halim, whose unwavering commitment and contributions during the creation of this journal and in the realm of community ophthalmology will forever be remembered. Though no longer with us, his invaluable contributions to the creation of this journal and his significant impact on community ophthalmology have left a lasting imprint on both the journal and the community.
REFERENCE
| [1] | Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract 2019; 157: 107843. |
| [2] | Flaxel CJ, Adelman RA, Bailey ST, Fawzi A, Lim JI, Vemulakonda GA. Diabetic retinopathy preferred practice pattern. Ophthalmology 2020; 127(1): 66-145. |
| [3] | Sasongko MB, Widyaputri F, Agni AN, et al. Prevalence of diabetic retinopathy and blindness in indonesian adults with type 2 diabetes. Am J Ophthalmol 2017; 181: 79-87. |
| [4] | Peraturan Kementrian Kesehatan Republik Indonesia Nomor 82 Tahun 2020 Tentang Penanggulangan Gangguan Penglihatan dan Gangguan Pendengaran. 2020. Available from:https://clinicaltrials.gov/ct2/results?cond=Melanoma&term=SiRNA&cntry=&state=&city=&dist= |
| [5] | Rajalakshmi R, Arulmalar S, Usha M, et al. Validation of smartphone based retinal photography for diabetic retinopathy screening. PLoS One 2015; 10(9): e0138285. |
| [6] | Goh JKH, Cheung CY, Sim SS, Tan PC, Tan GSW, Wong TY. Retinal imaging techniques for diabetic retinopathy screening. J Diabetes Sci Technol 2016; 10(2): 282-94. |
| [7] | Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care. Ophthalmology 2018; 125(10): 1608-22. |
| [8] | WHO. Diabetic retinopathy screening- a short guide. 2020. Available from:https://www.who.int/europe/publications/i/item/9789289055321#:~:text=The%20purpose%20of%20screening%20is,of%20vision%20impairment%20or%20blindness. |
| [9] | Hutchinson A, McIntosh A, Peters J, et al. Effectiveness of screening and monitoring tests for diabetic retinopathy – A systematic review. Diabet Med 2000; 17(7): 495-506. |
| [10] | Tan CH, Kyaw BM, Smith H, Tan CS, Tudor Car L. Use of smartphones to detect diabetic retinopathy: Scoping review and meta-analysis of diagnostic test accuracy studies. J Med Internet Res 2020; 22(5): e16658. |
| [11] | Ryan ME, Rajalakshmi R, Prathiba V, et al. Comparison Among Methods of Retinopathy Assessment (CAMRA) study. Ophthalmology 2015; 122(10): 2038-43. |
| [12] | Kesehatan, LPdP. Laporan Nasional Riskesdas 2018; 2019: 123-43. |
| [13] | Sovani I. Validitas Foto Fundus Portabel Satu Lapang Pandang Midriatika dalam Mendeteksi Retinopati Diabetika Mengancam Penglihatan 2019. |
| [14] | Halim A, Syumarti S, Rini M, et al. Prevalence and associated factors of diabetic retinopathy in people with type 2 diabetes attending community based diabetic retinopathy screening in greater bandung, indonesia. Int J Retina 2022; 5(1): 1. |
| [15] | Manao IL, Hutami HT, Rahmi FL, Saubig AN. The association of diabetes duration with the severity of diabetic retinopathy. Diponeg Med J 2021; 10(1): 64-8. |
| [16] | Sasongko MB, Indrayanti SR, Wardhana FS, et al. Low utility of diabetic eye care services and perceived barriers to optimal diabetic retinopathy management in Indonesian adults with vision-threatening diabetic retinopathy. Diabetes Res Clin Pract 2021; 171: 108540. |
| [17] | Scanlon PH. The English national screening programme for diabetic retinopathy 2003–2016. Acta Diabetol 2017; 54(6): 515-25. |
| [18] | Trevethan R. Sensitivity, specificity, and predictive values: Foundations, pliabilities, and pitfalls in research and practice. Front Public Health 2017; 5: 307. |
| [19] | Field A. Discovering Statistics Using SPSS 2011. |
| [20] | Wintergerst MWM, Mishra DK, Hartmann L, et al. Diabetic retinopathy screening using smartphone-based fundus imaging in India. Ophthalmology 2020; 127(11): 1529-38. |
| [21] | Sengupta S, Sindal MD, Baskaran P, Pan U, Venkatesh R. Sensitivity and specificity of smartphone-based retinal imaging for diabetic retinopathy. Ophthalmol Retina 2019; 3(2): 146-53. |
| [22] | Wintergerst MWM, Jansen LG, Holz FG, Finger RP. Smartphone-based fundus imaging-where are we now? Asia Pac J Ophthalmol 2020; 9(4): 308-14. |
| [23] | Ismael S. Dasar-dasar metodologi Penelitian Klinis 4th ed.. 2011. |
| [24] | Herman C. What makes a screening exam “good”? Virtual Mentor 2006; 8(1): 34-7. |
| [25] | Alexander LK, Lopes B, Ricchetti-Masterson K, Yeatts KB. Assessment of Diagnostic and Screening Tests. 2015. Available from:https://sph.unc.edu/wp-content/uploads/sites/112/2015/07/nciph_ERIC16.pdf |
| [26] | Maxim LD, Niebo R, Utell MJ. Screening tests: A review with examples. Inhal Toxicol 2014; 26(13): 811-28. |