All published articles of this journal are available on ScienceDirect.
The Role of Stress Reduction and Mindfulness Meditation in Glaucoma Management: A Review
Abstract
Glaucoma is a progressive optic neuropathy that is increasing in prevalence worldwide and can lead to devastating vision loss and even blindness if left untreated. Current medical and surgical approaches to glaucoma treatment all aim to lower intraocular pressure (IOP), which is a well-known risk factor for glaucoma development and progression. Although the exact pathogenesis of glaucoma is not yet fully elucidated, multiple studies suggest that mental stress and elevated cortisol levels may contribute to IOP elevation and glaucomatous progression. In recent decades, various randomized-controlled trials have also demonstrated a significant reduction of IOP in patients practicing stress-reduction techniques, including mindfulness meditation and yoga. In this review, we discuss the relationship between mental stress and glaucoma and review the supporting literature to highlight the potential role of mindfulness meditation as an adjunctive strategy to reduce stress and thereby lower IOP in glaucoma patients.
1. INTRODUCTION
Glaucoma is a type of progressive optic neuropathy that affects more than 70 million people, making it the leading cause of irreversible blindness worldwide [1]. Although the underlying pathogenesis of glaucoma remains poorly understood, intraocular pressure (IOP) is a well-established continuous risk factor for glaucomatous damage [2, 3]. Multiple studies, for instance, have demonstrated a direct correlation between increased IOP and the risk of glaucoma development and progression [4-8]. For this reason, medical and surgical glaucoma management, including topical eye drops, laser trabeculoplasty, and incisional glaucoma surgeries, all aim to lower IOP [9, 10].
The prevalence of glaucoma is expected to substantially increase in the coming decades due to an aging population [11]. Consequently, there is growing interest in identifying alternative IOP reduction strategies that could supplement our current medical and surgical glaucoma treatments [12, 13]. Previously proposed lifestyle-based approaches to IOP reduction include aerobic exercise, stress reduction, and supplementation with antioxidants and neuroprotective agents, such as Ginkgo biloba, coenzyme Q10, and nicotinamide [14-16]. In recent years, mindfulness meditation has garnered increased attention as a potential adjunctive treatment for reducing stress and lowering IOP, fueled by emerging evidence linking mental stress to glaucomatous progression [17-20]. However, there is still limited understanding of the effectiveness of mindfulness meditation for IOP reduction and the role it should play in glaucoma management. In this review, we aim to discuss current literature regarding the association between mental stress and glaucoma. We specifically highlight mindfulness meditation and relaxation techniques as a potential complementary approach to lowering IOP in conjunction with standard medical and surgical modalities of glaucoma treatment.
2. RELATIONSHIP BETWEEN MENTAL STRESS AND GLAUCOMA
The pathophysiology of glaucoma is complex and not yet fully elucidated. IOP is a known, modifiable contributor to the development and progression of glaucomatous damage [2, 3]. Vascular dysregulation and autonomic nervous system imbalance have also been suggested as key factors in the pathogenesis of certain glaucoma subtypes, including normal tension glaucoma [21-23]. In recent years, multiple studies have highlighted psychological stress as an upstream factor that can potentially modulate glaucoma risk by increasing IOP and impairing vascular autoregulation [24-29]. Nicou et al. (2021) and Turner et al. (2019) demonstrated that environmental disturbances causing acute stress led to substantial elevations of IOP in rats and non-human primates, respectively [25, 26]. Similar findings have been demonstrated in human populations. For example, Abe et al. (2020) measured significant increases in IOP after inducing psychological stress with the Trier Social Stress Test, a tool used to evaluate stress responses related to public speaking [27]. Jimenez and Vera (2018) similarly showed higher IOP values and cardiovascular indices (such as heart rate and blood pressure) in university students exposed to mental stress induced by test-taking compared to a control group [28]. In a prospective observational study on 151 glaucoma patients, the presence of mental stress was associated not only with increased IOP values but also with worsening of glaucoma based on visual field changes [29]. Such findings have led to an understanding that mental stress itself is a potentially modifiable risk factor for vision loss in glaucoma patients [24].
There are multiple proposed mechanisms for how mental stress modulates IOP and impacts glaucoma pathogenesis based on the physiological adaptations of the body to stress. The typical stress response involves the activation of two neural networks: the sympathetic adrenomedullary (SAM) system and the neuroendocrine stress response system, also known as the hypothalamic-pituitary-adrenal (HPA) axis [24]. The SAM system is responsible for acutely constricting blood vessels and increasing heart rate in response to stress [30]. The HPA axis, on the other hand, produces a slower, more prolonged stress response through the release of glucocorticoids from the adrenal gland into the bloodstream [31]. The activation of these neural networks is thought to influence glaucoma risk by causing intraocular pressure elevation, autonomic nervous system imbalance, and vascular dysregulation [29, 32, 33].
In humans, cortisol is the steroid hormone that is synthesized and released by the adrenal glands in response to HPA axis activation. In addition to regulating the body’s stress response, this glucocorticoid hormone plays an important role in suppressing inflammation, regulating blood pressure, modulating the sleep-wake cycle, and regulating the metabolism of nutrients, such as lipids, carbohydrates, and proteins [34]. In the context of chronic psychological stress, elevated levels of cortisol are associated with a wide variety of systemic conditions, including obesity, cardiovascular disease, diabetes, autoimmune disease, asthma, and cognitive disorders [31, 35, 36]. The effects of cortisol impact the eye as well, with multiple studies dating back over 50 years that have identified a strong correlation between high plasma cortisol levels and the incidence of ocular hypertension and primary open-angle glaucoma [37-40]. Although the anti-inflammatory and metabolic effects of cortisol are crucial in maintaining eye health and have even been harnessed to treat inflammatory eye diseases through the use of topical, periocular, and intravitreal steroid medications [41], prolonged exposure to glucocorticoids can lead to structural and molecular changes in the eye that result in IOP elevation and glaucoma [34]. For example, multiple studies have shown that glucocorticoids contribute to microstructural alterations in the aqueous outflow pathway through the upregulation of myocilin, a protein of unknown function that resides primarily in trabecular meshwork tissue [42, 43]. The binding of cortisol and other steroid medications to glucocorticoid receptor beta has also been postulated to alter trabecular meshwork function through a reduction in phagocytic cell activity [44]. These structural changes associated with cortisol exposure promote aqueous outflow resistance, which leads to elevated IOP and subsequent glaucomatous damage if not controlled appropriately [45, 46].
Even in patients with relatively normal IOP, vascular dysregulation and autonomic imbalance associated with chronic mental stress may play a crucial role in glaucoma pathogenesis, particularly in the setting of normal tension glaucoma [24]. In addition to glucocorticoids, SAM system signaling molecules, such as pro-inflammatory cytokines and endothelin-1, can accelerate the progression of both primary open angle and normal tension glaucoma by contributing to vasoconstriction, endothelial cell dysfunction, and impaired ocular blood flow [24, 47]. Stress hormones may also disrupt nitric oxide signaling, which normally functions as a potent vasodilator and helps to regulate aqueous outflow through the trabecular meshwork [48, 49]. Over time, these vascular changes can result in impaired regulation of ocular perfusion pressure and increased risk of the optic nerve and retinal ganglion cell ischemia, making the eye more vulnerable to glaucomatous injury [32, 33].
The relationship between mental stress and glaucoma is not unidirectional. While chronic psychological stress is linked to an increased risk of glaucoma development and progression, glaucoma itself can exacerbate stress levels. In a study on 589 glaucoma patients, over 80% reported experiencing negative emotions when they received a glaucoma diagnosis [50]. Other studies have demonstrated increased levels of depression and anxiety in patients with progressing or severe glaucoma [51, 52]. Additionally, glaucoma management is complex and often requires regular monitoring, strict medication adherence, and, in some cases, invasive treatments, all of which can further heighten stress levels [53]. Therefore, addressing both the physiological and psychological aspects of glaucoma is crucial to breaking this negative feedback loop and improving the quality of life for glaucoma patients.
3. MINDFULNESS MEDITATION FOR THE REDUCTION OF IOP
Although mindfulness meditation effectively reduces stress [54], it is not commonly used as an adjunctive glaucoma therapy. According to a 2002 Wills Eye Hospital survey of 1027 patients, only 1.8% of patients had ever utilized mindfulness meditation as a complementary approach to glaucoma treatment [13]. This is perhaps due to relatively scarce scientific evidence to support its usage and a limited understanding of how mindfulness meditation could be effectively applied in real-life clinical practice. Herein, we discuss the randomized-controlled trials that have investigated meditation for glaucoma in recent decades and the impact of mindfulness-based yogic exercises on IOP (Table 1). One of the earliest randomized-controlled trials to investigate the relationship between mindfulness practice and IOP was based in Germany in 1995 [55]. Kaluza and Strempel (1995) randomized primary open-angle glaucoma patients on standard medical therapy to either 1) a training group that underwent eight 90-minute weekly sessions of autogenic relaxation training in addition to their glaucoma drops (n = 11) or 2) a waiting-list control group that remained on their glaucoma drops alone (n = 12). After 8 weeks, both the training group and the control group were exposed to a mental stressor test (MST) designed to increase psychological stress [56]. Although there was no difference in the immediate rise of IOP in response to the MST for patients in the training and control groups (p > 0.05), patients in the training group demonstrated an average reduction of IOP by 3 mm Hg compared to the control group (p<0.001) [55, 56]. Unfortunately, the sample size in this study was very small, making it difficult to draw definitive conclusions about the role that mindfulness techniques should play in glaucoma management.
Decades later, Dada et al. conducted a series of three larger randomized-controlled trials to investigate the effectiveness of mindfulness meditation in treating glaucoma [18-20]. These studies evaluated the impact of meditation on IOP reduction and also investigated how meditation-induced IOP changes might be explained by changes in serum biomarkers, serum gene expression, trabecular meshwork gene expression, and optic nerve vasculature. In 2018, Dada et al. investigated the effect of meditation on primary open-angle glaucoma patients with medication-controlled IOPs [18]. They performed a prospective, single-blinded, and randomized-controlled trial with mindfulness meditation as the intervention arm. The primary endpoint was IOP, while the secondary endpoints were quality of life (QOL) scores (World Health Organization (WHO) questionnaires), stress-related serum biomarkers (i.e., cortisol, β-endorphins, IL6, TNF-α, brain-derived neurotrophic factor (BDNF), reactive oxygen species (ROS), and total antioxidant capacity (TAC)), and whole genome expression. The study included patients older than 45 years old with IOPs between 12 and 21 mm Hg and a best corrected visual acuity of 20/40 or better. Patients with newly diagnosed or uncontrolled glaucoma, a comorbid condition of vision loss (i.e., macular degeneration), a history of eye surgery in the past 6 months, or prior meditation experience were excluded. Ninety patients were randomized to two groups: 1) meditation + medication (n = 45) and 2) medication only (n = 45). Group 1 did 60 minutes of guided meditation with a trained Mindfulness Stress Based Reduction (MSBR) instructor at 8 AM daily. The meditation sessions consisted of breathing exercises, followed by mindfulness meditation. The study endpoints were measured on the first day of the meditation course and then again on day 21. Of note, the IOP was measured 5 hours after the meditation sessions to avoid possible transient IOP changes directly related to the sessions.
After 3 weeks, the intervention arm had several dramatic results compared to the control group. Analysis revealed a statistically significant reduction in IOP of 6 mm Hg (32%) in the meditation group compared to a reduction of <1 mm Hg for the non-meditation group (p < 0.001). Notably, 30 of the 40 participants (75%) who completed the full meditation course demonstrated a >25% reduction in IOP. There was also a significant improvement in the WHO QOL scores in all domains for the intervention arm (p < 0.001). Next, blood samples on days 1 and 21 were compared for differences in biochemical markers and gene expression profiling. The meditation group had significant decreases in serum cortisol, IL6, TNF-α, and ROS and significant increases in serum BDNF and TAC. They also had significantly different expressions of 109 genes, of which 54 were upregulated and 55 downregulated. For example, NGFR, TAZ, BNP, IL2, IL4, FGFR1, and metallothionein-I were upregulated, whereas RAR, CYP26A1, I-kB, EGFR, ERK7, PTGER3, and IL21A genes were downregulated in the meditation group. The meditation group also had decreased whole genome expression of BCL2L11, CARD8, and MAPK10, all of which are associated with apoptosis and inflammation [18].
This study by Dada et al. (2018) not only showed that meditation significantly reduced IOP but also simultaneously improved patient QOL [18]. The IOP reduction in their meditation study arm was comparable to using an additional eye drop (~30% reduction) without the drop-related side effects or QOL reduction [57]. The improved QOL parameters in the meditation group suggest that meditation may effectively target the mental stress that is thought to be an upstream factor for glaucoma risk. Dada et al. (2018) then used serum biomarkers and whole genome expression to build a possible mechanistic framework for how meditation ultimately impacts IOP [18]. For instance, the meditation group had decreased serum cortisol, IL6, TNF-α, and ROS levels. Cortisol, like other glucocorticoids, is notorious for increasing IOP by altering trabecular meshwork microstructure, as previously discussed. IL6 and TNF-α are both inflammatory markers, the latter of which causes metalloproteinase-associated tissue remodeling in glaucomatous optic nerve heads and IOP-induced retinal ganglion cell death [58, 59]. Additionally, oxidative stress from ROS damages the trabecular meshwork, especially the endothelial cells, which can further raise IOP [60, 61]. Therefore, a reduction in these biomarkers after mindfulness meditation may have contributed to the lower IOP seen in the intervention arm. In summary, meditation appeared to reduce stress-related serum biomarkers and modulate the expression of genes that may have harmful effects on the trabecular meshwork through inflammation, tissue remodeling, and apoptosis. The conclusion that these systemic changes affected ocular tissues in this study was an assumption until the second study in 2021 addressed it [20].
In 2021, Dada et al. subsequently conducted a randomized-controlled trial that assessed primary open-angle glaucoma patients in imminent need of a trabeculectomy due to uncontrolled high IOP [20]. This study expanded on the conclusions of the 2018 study by also exploring if meditation actually affected ocular tissues. The 2021 study included patients with IOPs ≥21 mm Hg and optic nerve head cup-to-disc ratio >0.7 on maximum medical therapy. The endpoints were similar to the 2018 study but also included diurnal IOP measurements (Goldmann tonometry every 3 hours on days 1 and 21) [18, 20]. The 2021 study was conducted in two stages (Fig. 1). In stage 1, 60 patients were randomized to an intervention group (daily guided meditation + current medications) and a control group (current medications only) for 21 days. On day 21, “success” was defined as IOP ≤15 mm Hg and “failure” as IOp >15 mm Hg. In stage 2, those with IOP ≤15 mm Hg continued their current management, while those who failed received a trabeculectomy and had their trabecular meshwork punches submitted for genome expression profiling. The patients who initially were in the meditation arm, regardless of whether trabeculectomy was ultimately performed, were instructed to continue meditating at home without guidance. Repeat measurements were done after 6 weeks (9 weeks total after enrollment).
| Authors/Year | Participants and Intervention | Main Results |
|---|---|---|
| Kaluza and Strempel 1995-6 [55, 56] | 23 POAG patients on standard drops: • 11 patients in the study group underwent 90-minute weekly sessions of autogenic relaxation training for 8 weeks in addition to drops • 12 patients in the control group used drops alone |
Average reduction of IOP by 3 mm Hg in the study group compared to the control group (p < 0.001) |
| Gagrani et al. 2018 [71] | 60 POAG patients on standard drops: • 30 patients in the study group underwent 45-minute daily breathing exercises for 6 weeks in addition to drops • 30 patients in the control group used drops alone |
Average reduction of IOP by 1.5 mm Hg in the study group compared to <0.1 mm Hg in the control group (p = 0001) |
| Dada et al. 2018 [18] | 90 POAG patients on standard drops: • 45 patients in the study group underwent 1 hour of daily mindfulness meditation for 3 weeks in addition to drops • 45 patients in the control group used drops alone |
Average reduction of IOP by 6 mm Hg in the study group compared to <1 mm Hg in the control group (p < 0.001) |
| Dada et al. 2021 [20] | 60 POAG patients with uncontrolled high IOP on maximum drops: Stage 1: • 30 patients in the study group underwent daily guided meditation for 3 weeks in addition to drops • 30 patients in the control group used drops alone Stage 2: • Patients with IOP ≤15 mm Hg continued current management • Patients with IOp >15 mm Hg underwent trabeculectomy in addition to home meditation or drops |
Stage 1: Average reduction of IOP by 5 mm Hg in the study group compared to 0.2 mm Hg in the control group (p = 0.001) Stage 2: 50% of participants in the study (meditation) group had IOp >15 mm Hg and required trabeculectomy, and 100% of participants in the control (non-meditation) group had IOp >15 mm Hg and required trabeculectomy |
| Dada et al. 2021 [19] | 60 POAG patients on standard drops: • 30 patients in the study group underwent a 6-week mindfulness meditation course in addition to drops • 30 patients in the control group used drops alone • Circumpapillary vessel density was evaluated with optical coherence tomography angiography (OCT-A) in both groups |
Average reduction of IOP by 2 mm Hg in the study group compared to 0.8 mm Hg in the control group (p = 0.001) and increased circumpapillary vessel density on OCT-A in the study group compared to the control group |
| Udenia et al. 2021 [69] | 90 POAG patients on standard drops: • 45 patients in the study group underwent 30-minute daily breathing exercises in addition to drops • 45 patients in the control group used drops alone |
Average reduction of IOP by 6 mm Hg in the study group compared to the control group (p < 0.001) |
| Ismail et al. 2022 [70] | 62 POAG patients on standard drops: • 31 patients in the study group underwent daily guided Jyoti-Trataka mindfulness sessions in addition to drops • 31 patients in the control group used drops alone |
Average reduction of IOP by 3 mm Hg in the study group and 0 mm Hg in the control group (p < 0.001) |
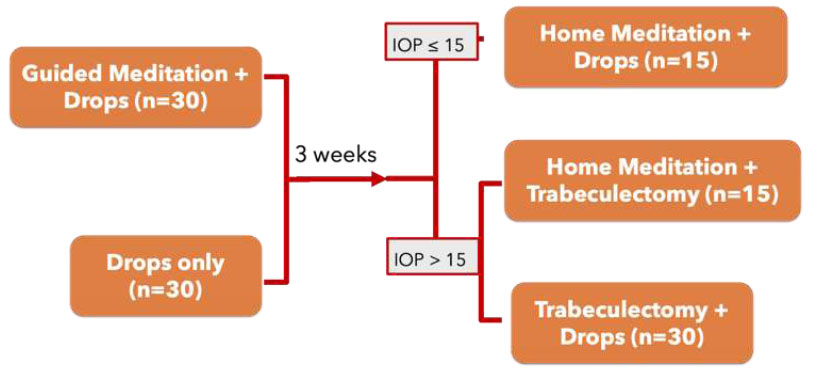
Flow chart of the study by Dada et al. (2021).
After 21 days and at the end of stage 1, the meditation group had a significant decrease in mean IOP (5 mm Hg, 23.34% reduction) and diurnal IOP range (4.07 to 1.75 mm Hg) compared to that of the control group (mean IOP decrease of 0.2 mmHg and change in diurnal IOP range from 4.5 to 4.28 mm Hg; p = 0.001). Half of the participants in the meditation group (n = 15) and all of the participants in the control group (n = 30) did not show any significant change (IOp >15 mm Hg). Of note, 7 patients in the meditation group who met the success criteria (IOP ≤15 mm Hg) actually had IOP ≤12 mm Hg at day 21. At the end of stage 2, there were patients in 3 groups: meditation + drops, meditation + trabeculectomy, and trabeculectomy only (Fig. 1). All groups had significant reductions in IOP by the end of the study period (mean IOP of 12.8 mmHg, 11.8 mmHg, and 13.3 mmHg, respectively; p = 0.0001). The patients with the largest ultimate IOP decrease were those in the meditation group who also received a trabeculectomy. Trabecular meshwork gene expression was compared between the intervention and control groups; the meditators had significant upregulation of NGB, NGFR, NRG1, NOS1, NOS3, MNTR1A, NR3C1, and MT1E, and downregulation of IL4, BCL2L11, CARD8, FGFR1, MAPK10, MAPK15, TGFB, TNFA, NFkB, and EGFR.
This study showed that meditation was associated with both significantly decreased mean IOP and diurnal IOP range [20]. About 86% of the meditation group had ≥15% IOP reduction, and half of the meditation group had enough IOP reduction to avoid trabeculectomy. This effect was sustained 6 weeks later, even though the guided group meditation session was changed to home meditation, implying that patients were perhaps able to maintain an effective meditation practice by themselves. Even the meditators who needed a trabeculectomy had the largest IOP decrease compared to the patients with trabeculectomy alone. These results suggest that meditation may also be effective as an adjunctive therapy for patients with uncontrolled IOP; not only can it potentially delay incisional surgery, but it can also be a supplementary treatment pre- and post-operatively if surgery is indicated. Lastly, the comparison of the trabecular meshwork genome expression revealed that gene expression in ocular tissues between the intervention and control groups had significant differences. The meditation group had decreased expression of NFkB (pro-inflammation), TGFB (trabecular meshwork fibrosis), and EGFR (trabecular meshwork remodeling) and increased expression of NOS (increased trabecular meshwork flow and vasodilation) [48] and melatonin receptors (IOP homeostasis) [20]. This 2021 study strengthens the hypothesis that meditation first reduces the whole body stress response (serum biomarker and whole genome expression) [18], which then changes ocular tissues (trabecular meshwork genome expression) to eventually reduce IOP [20].
In 2021, Dada et al. also performed a follow-up randomized controlled trial investigating the effects of meditation on the optic nerve head using ocular coherence tomography angiography (OCT-A) [19]. As vascular changes have been linked to glaucoma [22, 62], this study evaluated the effect of meditation on the optic nerve head microvasculature. The study design was similar to that of a study conducted in 2018; 60 primary open-angle glaucoma patients with IOPs <21 mm Hg on medications were randomized to meditation and control groups [18, 19]. OCT-A and IOP measurements were performed at the beginning and end of a 6-week meditation course. The study again confirmed that daily meditation significantly reduced IOP compared to the control group (p = 0.001), with 23 (38%) eyes demonstrating a <10% reduction in IOP, 33 (55%) eyes showing a 10-15% reduction in IOP, and 4 (7%) eyes having a >15% reduction in IOP. OCT-A imaging showed that the meditation group had significantly increased circumpapillary vessel density superiorly (p = 0.02) and nasally (p = 0.01), circumpapillary vessel perfusion (p < 0.001), and flux index (p < 0.001) compared to the control group. As decreased circumpapillary vessel perfusion and density have been linked to worsening visual fields, increasing these parameters via meditation may be protective against glaucoma progression [63, 64]. Although the mechanism for how meditation specifically affects optic nerve head vasculature has not yet been elucidated, it is reasonable to postulate that meditation-induced reduction of SAM system signaling, as previously discussed, could counteract sympathetic-driven vasoconstriction and lead to increased vascular perfusion of the nerve [24, 47].
Another practice that has been studied in relation to glaucoma and IOP reduction is yoga, which incorporates physical postures, breathing techniques, focusing exercises, and mindfulness meditation to reduce stress and foster physical and mental well-being [65-68]. Yogic breathing and focusing exercises, such as Jyoti-Trataka (gazing at a single point or candle flame) or meditation-focused breathing, have been shown to reduce IOP in glaucoma patients [69-71]. In a clinical trial by Ismail et al. (2022), 62 open-angle glaucoma patients were included. Thirty-one patients were randomized to a study group that participated in guided Jyoti-Trataka mindfulness sessions with a certified yoga instructor in addition to their baseline glaucoma medication, and 31 patients were randomized to a control group with glaucoma medication only [70]. Compared to the control group, which demonstrated a mean IOP of 26.40 mm Hg after 1 month, the study arm demonstrated a significant reduction in not only mean IOP (23.23 mm Hg) but also systolic and diastolic blood pressure measurements (p < 0.05). This study supported the hypothesis that yogic focusing exercises, such as Jyoti-Trataka, may be useful in reducing IOP in glaucoma patients in conjunction with standard medical therapy for glaucoma. Yogic breathing exercises have also been associated with a potentially beneficial effect on IOP in glaucoma patients. In a randomized-controlled trial by Udenia et al. (2021), 90 patients with moderate and severe primary open-angle glaucoma were randomized to either a yoga group combined with glaucoma medication (n = 45) or a control group with glaucoma medication only (n = 45) [69]. Patients in the yoga group participated in diaphragmatic breathing and alternate nostril breathing exercises for 30 minutes per day over a period of 6 months. Compared to the control group, the yoga group demonstrated IOP reductions of nearly 6 mm Hg in each eye after 6 months (p < 0.001). Gagrani et al. (2018) also investigated the effect of breathing exercises on IOP in moderate and severe primary open-angle glaucoma patients [71]. In their study on 60 glaucoma patients, 30 patients were randomized to a yoga group in addition to standard medical treatment, and 30 patients were randomized to a control group with standard medical treatment only. The yoga group participated in meditation focused on breathing exercises for 45 minutes per day over 6 weeks. After 6 weeks, the yoga group demonstrated a significant reduction in mean IOP (15.9 to 14.4 mm Hg; p = 0.0001) compared to the control group (15.7 to 15.65 mm Hg; p = 0.41) [71]. These studies demonstrated that mindfulness-based breathing exercises may be useful for reducing IOP in both the short-term (6 weeks) [71] and the long-term (6 months) [69].
Unfortunately, not all relaxation practices are helpful for achieving IOP reduction, and some forms of yoga may even lead to elevated IOP and increased risk of glaucoma progression [65]. For example, two case studies and a prospective single-center observational study showed that breath-holding exercises and Asanas (yoga postures) that involve head-down positioning are associated with significantly increased IOP during practice and, in some cases, may even lead to worsening visual field defects [72-74]. For this reason, providers should be prudent in the types of yoga and mindfulness practices that they recommend to patients with glaucoma.
4. LIMITATIONS AND FUTURE DIRECTIONS
The studies discussed in this review highlight the possible effectiveness of mindfulness meditation and relaxation techniques as adjunctive strategies for IOP reduction. However, there is still a scarcity of data regarding the usage of meditation in actual clinical practice, as well as a limited understanding of how these techniques impact IOP and glaucoma prognosis in the long term. Many of the studies that have investigated the relationship between mindfulness meditation, yogic practices, and IOP reduction have been limited to relatively small sample sizes. For example, Kaluza and Strempel (1995) included only 23 patients in total, which limits the generalizability and reliability of their findings [55]. To address this sample size limitation and provide a more precise estimate of the relationship between mindfulness practices and IOP, two meta-analyses were performed. Zaher et al. (2023) evaluated studies related to the impact of meditation, autogenic or ocular relaxation exercises, or yoga on IOP, and Chetry et al. (2023) evaluated studies related to the impact of yogic practices on IOP [65, 75]. In the meta-analysis by Zaher et al. (2023), regular practice of yoga for 6 weeks was associated with a 22% reduction in IOP, and meditation was associated with an average reduction of IOP by 2.02 mm Hg [75]. Similarly, in the meta-analysis by Chetry et al. (2023), pooled data from multiple randomized-controlled trials showed a decrease in mean IOP by 1-2 mm Hg after 4-6 weeks of participation in relaxation yoga techniques (p < 0.05) [65]. Although meta-analyses can be useful for increasing overall sample size and, consequently, increasing power to study an effect of interest [76], additional primary studies with larger sample sizes would be useful to better understand the impact of mindfulness practices on IOP in glaucoma patients.
Randomization of patients into exposure and control groups is useful for reducing the potential for bias in a study. However, in the context of mindfulness meditation and IOP-related studies, it is difficult to account for all potential confounding variables since IOP can be influenced by numerous factors. In multiple studies, for example, patients were continued on their baseline topical glaucoma medications, which could potentially confound the IOP findings (although Dada et al. attempted to account for this by demonstrating no significant differences between the intervention and control groups with regard to the types (p = 0.21 to 0.34) and numbers (p = 0.19 to 0.70) of glaucoma medications used) [19, 20, 55, 56, 69, 70]. Additionally, these studies had relatively short follow-up intervals (ranging from 3 to 9 weeks), so it is uncertain if the beneficial effects of meditation could be sustained for months to years [65, 75]. The current lack of long-term follow-up precludes the ability to determine if meditation actually reduces visual field loss, which is the end-point of greatest clinical utility. Therefore, we cannot yet know how the use of mindfulness meditation in clinical practice would impact the long-term visual prognosis of glaucoma patients. Further clinical trials with longer follow-up periods are needed to assess if meditation actually decreases glaucoma progression long-term.
Although there were no harmful effects from mindfulness meditation alone, it was still time-consuming to commit to one hour of meditation daily. For this reason, many studies used an instructor to provide daily guided meditations and ensure consistent compliance with treatment sessions [18-20, 56]. It is unclear if patients have the time or motivation in real-life settings to attend guided hour-long meditation sessions or if this duration of meditation is even necessary to achieve useful IOP reduction. The 2021 study by Dada et al. showed encouraging data that after 3 weeks of guided meditation sessions, those who continued their practice at home without guidance maintained a lower IOP even 6 weeks later [20]. A survey of 100 patients in Australia also showed that 63% were amenable to doing 45-60 minutes of meditation daily for glaucoma if prescribed by a doctor [17]. Still, agreeability and actual performance are two different aspects. Further studies that mimic real-world settings, such as fewer guided sessions, shorter meditation times, or even the usage of a meditation-guided phone application, are needed to evaluate the practicality of meditation as a therapy.
Although mindfulness meditation has gained increasing acceptance in the medical community, especially via MSBR therapy, it is still not yet considered a mainstream adjunctive medical treatment. There may be a scarcity of trained MSBR instructors or a lack of awareness on how patients can be referred to them. We hope that these logistical hurdles become less as the evidence for meditation as a complementary glaucoma therapy increases.
CONCLUSION
In numerous randomized-controlled trials, mindfulness meditation and relaxation techniques have been associated with a significant reduction of IOP relative to standard medical treatment of glaucoma alone. These findings suggest that meditation may be a useful adjunctive, non-invasive strategy to optimize IOP management in glaucoma patients. However, it is still unclear whether the beneficial effects of meditation persist long-term. Additionally, mindfulness-based practices should not be used as a replacement for standard medical and surgical treatment of glaucoma. Furthermore, multi-year studies are needed to ascertain the real-life clinical feasibility and long-term effectiveness of mindfulness meditation in glaucoma management.
AUTHORS’ CONTRIBUTION
A.P. and A.P.M.: Study conception and design; A.P. and A.P.M.: Data collection; A.P. and A.P.M.: Analysis and interpretation of results; A.P., A.P.M., B.C.S., and B.M.W.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.


