All published articles of this journal are available on ScienceDirect.
Agreement between Two Biometers for Central Corneal Thickness Measurement in High Myopia Patients
Abstract
Background
In refractive surgery, the measurement of Central Corneal Thickness (CCT) is a critical factor in the preparation and screening of surgery to correct myopia. CCT measurements can be measured by optical biometers, including the Scheimpflug camera and Swept-source Optical Coherence Tomography (SS-OCT).
Aim
This study aimed to compare the Central Corneal Thickness (CCT) measurements made with Swept-source Optical Coherence Tomography (SS-OCT)-based biometers and the Scheimpflug camera in patients with high myopia.
Methods
An analytical cross-sectional study was performed to evaluate the agreement between Central Corneal Thickness (CCT) values obtained using Swept-source Optical Coherence Tomography (SS-OCT) and the Scheimpflug camera. We included a total of 28 individuals with high myopia, including 44 eyes, for our study. These patients underwent Central Corneal Thickness (CCT) tests using both Swept-source Optical Coherence Tomography (SS-OCT) and the Scheimpflug camera. The Bland-Altman test was used to assess the agreement between the two devices.
Results
Forty-four eyes with axial lengths ranging from 26.05 to 34.02 mm based on SS-OCT examinations were included in this study. The mean CCT was 527.59 ± 35.710 (p <0.05) μm and 525.64 ± 35.421 μm (p <0.05), based on SS-OCT and the Scheimpflug camera, respectively. The Bland-Altman plot revealed good agreement between both devices, with a mean difference of 2.3409 μm; however, a 95% limit of agreement demonstrated a wide range, ranging from -8.48509 to 12.39400 μm at a 95% confidence interval.
Conclusion
CCT measurements using SS-OCT and the Scheimpflug camera differed significantly among patients with high myopia. Our findings have suggested that CCT measurements made with either device should be interpreted with caution and not be used interchangeably.
1. INTRODUCTION
Central Corneal Thickness (CCT) is an important measure in the clinical practice of ophthalmology. CCT measurement can be used in the diagnosis of corneal diseases, such as keratoconus, Fuchs’ endothelial dystrophy, endotheliitis, preoperative and postoperative evaluation for keratorefractive surgery, and the evaluation of intraocular pressure in patients with glaucoma. There are a number of variables that can affect the accuracy of intraocular pressure measurements using Goldmann applanation tonometry as the gold standard, including CCT, corneal curvature, and previous corneal surgery [1, 2]. CCT measurements can also be used to evaluate endothelial function before and after cataract surgery [3, 4]. Accurate CCT measurement values are an important step in the clinical evaluation in ophthalmological practice [5].
Myopia is a preventable cause of visual impairment in both children and young adults. Myopia is defined as having an axial length greater than or equal to 24.00 to 26.00 mm or a spherical equivalent of ≤ -0.50 D, whereas high myopia is defined as having an axial length greater than or equal to 26.00 mm or the spherical equivalent of ≤ -6.00 [6-8]. The prevalence of myopia is increasing in various countries, particularly in East and Southeast Asia. It is estimated that the prevalence of myopia will reach five billion people per year by 2050 [9]. In teenagers and young adults, the prevalence of myopia has been increasing by 80–90% in East and South East Asia, followed by a prevalence of high myopia of 10–20% [8]. Refractive surgery, especially laser in situ keratomileusis, has become increasingly popular in Asia, particularly in patients with high myopia. CCT measurement is an important consideration in refractive surgery when screening and planning surgery to correct myopia [10].
Previously, ultrasound pachymetry was considered the most reliable method for measuring CCT. However, it has several disadvantages, such as a direct contact probe to the cornea that may cause corneal epithelial defects, irritation, or infection [10]. Other disadvantages include the need for topical anesthesia and incorrect localization that may cause misdiagnoses [11]. CCT measurement can also be done using other techniques, like biometers, Optical Coherence Tomography (OCT), and specular microscopy [10]. The rotating Scheimpflug camera (Pentacam AXL, Oculus) is one of the technologies frequently used in CCT measurement in refractive surgery, especially in patients with high myopia [12]. Swept-source OCT (SS-OCT) (IOLMaster 700, Zeiss Meditec) is commonly used for the calculation of intraocular lens power. This instrument can also measure anterior segment parameters, such as CCT, anterior chamber depth, lens thickness, and axial length [13]. In recent years, various types of non-contact instruments have been developed for CCT measurements and have been used in clinical settings because of their advantages. It is important to determine the discrepancies of the devices [14].
A previous study showed that CCT measurements in healthy individuals using ultrasonic pachymetry and optical instruments are not directly interchangeable [11]. Another study by Omoto et al. revealed moderate agreement in CCT measurement between two optical biometers using SS-OCT [15]. This study aimed to investigate the agreement between SS-OCT and the Scheimpflug camera in CCT measurement in patients with high myopia. To our knowledge, this is the first study that has compared CCT measurements using SS-OCT and the Scheimpflug camera in patients with high myopia.
2. METHODS
This prospective, cross-sectional, analytical study was conducted from July to October 2022 at Cicendo National Eye Hospital, and was approved by the local ethics committee. The study was carried out in accordance with the Declaration of Helsinki. The study was conducted prospectively using consecutive sampling. All the participants provided written informed consent. The study included 44 eyes from 28 patients with high myopia over 18 years of age and an axial length of 26.00 mm. The patients had both uncorrected and best-corrected visual acuity assessments, as well as anterior and posterior segment measurements. Axial length and biometric data were measured using SS-OCT.
SS-OCT is an optical biometer based on the SS-OCT principle that uses an infrared laser diode with a wavelength of 1034–1095 nm. Longer wavelengths may reduce light scattering and increase the ability of light penetration [16]. The IOLMaster 700 uses 18 reference points with hexagonal patterns at 1.5, 2.4, and 3.2 mm from the optical zone in the central cornea to detect the corneal curvature. CCT measurements were performed at the corneal vertex [17].
The Scheimpflug camera is a non-contact instrument that combines the Scheimpflug camera rotation and partial coherence interferometry using a blue light-emitting diode with a wavelength of 475 nm as the light source. The Scheimpflug camera on the Pentacam AXL obtains measurements from 138.000 points from the entire cone and calculates keratometry from the central cornea [17]. Pentacam AXL detects 25 slit captures from the anterior segment in two seconds and automatically estimates the corneal pachymetry from the central cornea. It can obtain multiple measurements of anterior segment parameters, such as CCT, anterior chamber depth, lens thickness, and axial length [18].
Each patient underwent CCT measurements performed by a single examiner using SS-OCT and a Scheipmflug camera. The patient was positioned on a chin rest, pressing the forehead against the forehead strap, and then asked to look at the fixation point. The cornea and pupil were positioned at the center, and images were captured automatically by the instrument. The measurements were performed in a dimly lit room.
Unreliable measurements of both devices, according to the requirements of each device, were excluded from the study. Patients with a cataract density greater than grade II, a history of corneal abnormalities or a history of wearing contact lenses in the last two weeks before the measurements, a history of intraocular trauma or surgery, a history of any corneal surgery, a history of using any eyedrops in the previous month, and patients who were unwilling or could not be examined by either device were also excluded from the study.
The sample size required for the current study was estimated to be 40 eyes with a 95% confidence interval and an 80% statistical power. The following formula was used in this study:
 |
Where, n is the sample size, z is the selected alpha and beta for significance and power test value, P is the proportion, and π is the discordance. After considering a 10% non-response rate, the total sample size was forty-four eyes.
The normality of the data was confirmed using the Shapiro–Wilk test (p ≥0.05). The statistical analysis was performed using a paired t-test to compare both instruments and assess the Limit of Agreement (LoA) of 95% based on the Bland-Altman plot. A one-sample t-test was used to compare the difference in agreement between the IOLMaster 700 and Pentacam AXL. A p-value of <0.05 was considered to indicate a statistically significant difference between both devices. The data were analysed using IBM SPSS Statistics for Windows, version 24.0 (IBM Corp., Armonk, NY, USA).
3. RESULTS
A total of 44 eyes (28 patients) were included. The mean age was 36.82 ± 15.62 years, with a range of 18–73 years, and 15 (53.6%) patients were female. The axial length ranged from 26.05 to 34.02 mm based on SS-OCT measurements, with a mean of 28.11 ± 2.003 mm, as shown in Table 1.
The mean CCT measurements in this study were 527.59 ± 35.710 μm and 525.64 ± 35.421 μm, based on the SS-OCT and Scheimpflug camera measurements, respectively. The range of CCT measurements in this study was 438–597 μm and 444–595 μm based on the SS-OCT and Scheimpflug camera measurements, respectively (p <0.001; Table 2). The 95% LoA exhibited a range of -8.48509 to 12.39400 μm (p = 0.006) with a mean difference of 1.95455 μm. Both devices were strongly correlated, with an “r” value of 0.989 based on Pearson’s analysis and a p-value of <0.001. The Bland–Altman plots of the mean CCT differences between SS-OCT and the Scheimpflug camera are shown in Fig. (1).
| Variable | N=28 |
|---|---|
| Age | |
| Mean±SD | 36.82±15.63 |
| Median | 30.50 |
| Range (min-max) | 18.00-73.00 |
| Sex | |
| Male | 13(46.4%) |
| Female | 15(53.6%) |
| Variable | Axial length (mm) |
| Based on SS-OCT | |
| Mean±SD | 28.11±2.003 |
| Median | 27.72 |
| Range (min-max) | 26.05-34.02 |
| Variable | Group | P-value | 95% LoA | - | - | |
|---|---|---|---|---|---|---|
| SS-OCT | Scheimpflug Camera | Pearson Correlation Coefficient | P-value | |||
| (N=44) | (N=44) | - | ||||
| CCT | - | - | - | - | - | - |
| Mean±SD | 527.59±35.710 | 525.64±35.421 | 0.0001** | -8.48509 to 12.39400 | 0.989 | 0.0001** |
| Median | 527.50 | 525.50 | - | - | - | - |
| range (min-max) | 438.00-597.00 | 444.00-595.00 | - | - | - | - |
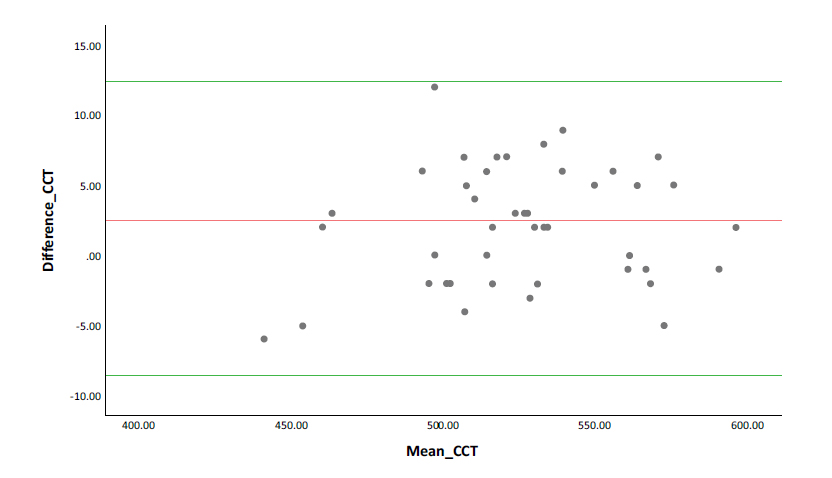
A Bland-Altman plot showing poor agreement between CCT measurements using SS-OCT and Scheimpflug camera. The red line shows the mean difference and the green line shows the upper and lower 95% LoA (CCT = central corneal thickness, SS-OCT = swept-source optical coherence tomography).
4. DISCUSSION
CCT measurements in patients with high myopia are important, especially in those who undergo refractive surgery. Various optical instruments are used for CCT measurements in daily practice. Various studies have compared CCT measurement values between optical instruments and ultrasound pachymetry as the gold standard. However, the results of these studies have been inconsistent. Several studies have shown Pentacam and ultrasound pachymetry to provide comparable results in CCT measurements with high repeatability in healthy individuals [5]. However, Modis et al. demonstrated that Pencatam HR and ultrasound pachymetry should not be used interchangeably for CCT measurements [19]. Pateras et al. compared ultrasound pachymetry and two different optical biometers, IOLMaster 700 and RTVue XR Angiovue, for CCT measurements. They found IOLMaster 700 to be comparable with ultrasound pachymetry for corneal thickness measurements [20]. Previous studies have also shown high repeatability in segment anterior parameter and CCT measurement using the IOLMaster 700 and Pentacam [21-23]. To our knowledge, there is currently no published data evaluating the agreement in CCT measurement between SS-OCT and the Scheimpflug camera in patients with high myopia.
Our study has demonstrated significant differences in CCT measurements between SS-OCT and the Scheimpflug camera in patients with high myopia, with a mean difference of 1.95455 μm and a maximum difference of 12.00 μm (p <0.001). In this study, SS-OCT measurements obtained were significantly thicker than those obtained using the Scheimpflug camera. Liao et al. showed the CCT measurements in healthy individuals based on the IOLMaster 700 to have a significantly higher value than the Tomey OA-200; both instruments have obtained SS-OCT measurements [24]. Another study by Kumar et al. demonstrated the mean CCT measurements of Pentacam to have a significantly lower value than that of IOLMaster 700 by a mean difference of 1.56 μm (p <0.001) [3]. These findings have not been found to be in accordance with the study by Kiraly et al. that has shown Pentacam HR to exhibit a higher CCT measurement value than the IOLMaster 700 in healthy patients with a mean of 10.99 μm (p ≤0.001) [25]. Each device uses different reference points for central measurements, which may cause a different value in CCT measurements [3].
Based on the analysis in the present study, we found a strong positive correlation between SS-OCT and the Scheimpflug camera with a correlation coefficient of 0.989. However, the Bland-Altman plot demonstrated that the two measurements should not be used inter- changeably. The present study has demonstrated a large LoA of approximately 20 μm. The values were scattered throughout the plot, and the CCT measurements based on these instruments could not be correlated. A study by Jiang et al. demonstrated that CCT values in IOLMaster 700 and Tomey EM-3000 should not be used interchangeably due to bias and wide variation in the measurement [21]. Mayali et al. also demonstrated that Pentacam should not be used interchangeably with handheld contact ultrasound pachymetry and a specular microscope because the 95% LoA was 34 μm and 42 μm, respectively [26]. Another study by Ruixue et al. compared the measurements of the Scheimpflug camera combined with partial coherence interferometry, Pentacam AXL and large coherence length SS-OCT, and the Argos biometer in healthy individuals and found differences of 1.15 ± 5.79 μm in CCT measurements and narrow ranges in Bland-Altman plots [27]. A study by Kiraly et al. reported an agreement of CCT measurements between Pentacam HR and IOLMaster 700 to be lacking in healthy individuals.
CCT values are fundamental for the preoperative assessment of keratorefractive surgery, especially in patients with high myopia [25]. Pentacam is a non-contact instrument that evaluates corneal thickness with a 475 nm monochromatic blue beam reflected from corneal surfaces with different active indices. Pentacam calculates the distances between the anterior and posterior surfaces and provides the CCT values of the cornea. Different variable measurement points could result in statistically significant differences for each measurement instrument. IOLMaster 700 is an SS-OCT instrument that measures CCT in the optical axis and the anterior corneal position, recognized as the surface tear layer [15]. Pentacam HR and IOLMaster 700 have different algorithms for calculating corneal thickness, which may be the cause of the findings in this study. Patient fixation is also an important factor in measuring corneal thickness using optical instruments. The tear film should also be considered when determining the accuracy of CCT measurements [25]. The differences in this study have suggested the need for standardized protocols in clinical practice. By establishing clear guidelines on which measurement device to use for CCT evaluations, ophthalmologists can enhance the accuracy and reliability of their assessments to improve surgical outcomes.
A limitation of our study is that the measurements were obtained only from patients with high myopia. Therefore, patients with axial lengths other than 26.05–34.02 mm may have different agreement results. Only healthy corneas from healthy individuals were analysed in this study. Consequently, this study could not be applied to previous corneal surgery or pathological cornea. This study has also evaluated both eyes of the patients, which may have resulted in bias. This study also did not conduct a repeatability test, although previous repeatability results in CCT measurements for both the IOLMaster 700 and the Pentacam AXL were excellent [21-23]. To our knowledge, this is the first study that has compared SS-OCT and the Scheimpflug camera for CCT measurement, especially in patients with high myopia.
CONCLUSION
CCT measurements using SS-OCT and the Scheimpflug camera have been found to differ significantly in patients with high myopia. Our findings have suggested that ophthalmologists should use these devices with caution when interpreting CCT values obtained using these devices, especially in high myopia patients in whom accurate corneal thickness assessments are critical for surgical planning and management. Both devices can be used for CCT measurements in clinical settings and research applications. However, in clinical settings, where CCT values are crucial, CCT measurements based on SS-OCT and the Scheimpflug camera should not be used interchangeably. Future studies should aim to establish standardized protocols for CCT measurement in high myopia patients to enhance the accuracy and reliability of preoperative assessments, ultimately improving patient outcomes in refractive surgery.
AUTHORS’ CONTRIBUTION
B.B.: Study conception and design; L.M.T.: Writing of the paper; A.M.H.K.: Data analysis or interpretation; E.D.S.: Data collection.
LIST OF ABBREVIATIONS
| CCT | = Central Corneal Thickness |
| SS-OCT | = Swept-source Optical Coherence Tomography |
| LoA | = Limits of Agreement |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by Cicendo National Eye Hospital’s ethical committee, Indonesia with approval number LB.02.01/2.3/8264/2022.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee, and with the 1975 Declaration of Helsinki, as revised in 2013.


