All published articles of this journal are available on ScienceDirect.
Evaluating the Effectiveness of Laser Peripheral Iridotomy on Angle-closure Diseases: The Role of Spectral Domain Anterior Segment Optical Coherence Tomography (SD AS-OCT) in Indonesia Tertiary Eye Hospital
Abstract
Background
Laser Peripheral Iridotomy (LPI) is a management approach in primary angle-closure disease by eliminating the presence of a pupillary block. Spectral Domain Anterior Segment Optical Coherence Tomography (SD AS-OCT) can measure the anterior chamber parameters quantitatively.
Objective
To determine the difference in anterior biometric parameters before and after LPI using SD AS-OCT in primary angle closure disease.
Methods
This is an analytical observational study with a cross-sectional method. A total of 22 eyes were included and underwent LPI. The angle opening distance (AOD 500 and 750), trabecular iris space area (TISA 500 and 750), anterior chamber depth (ACD), anterior chamber width (ACW), anterior chamber area (ACA), and lens vault (LV) was measured using SD AS-OCT before and 1 week after LPI. Statistical tests were performed with paired t-test or Wilcoxon's alternative test.
Results
We conducted LPI in 22 eyes with primary angle closure disease (9 eyes Primary Angle Closure Suspect (PACS), 7 eyes Primary Angle Closure (PAC), and 6 eyes Primary Angle-Closure Glaucoma (PACG)). There was a significant decrease of intraocular pressure (p=0.001) and a significant increase of mean values for AOD500, AOD750, TISA500, and TISA750 (p=0.0001) before and 1-week after LPI. The anterior segment showed statistically significant change in ACD, ACW, and ACA before and after LPI (p=0.006, p=0.001, p=0.049; respectively). The changes of LV did not show any statistically significant difference (p=0.770).
Conclusion
There was a significant difference in anterior biometric parameters in angle closure disease. Laser Peripheral Iridotomy could widen the anterior chamber and the angle.
1. INTRODUCTION
Glaucoma is one of the main causes of blindness globally, other than cataract and refractive errors [1]. Angle-closure glaucoma is the most common type of glaucoma in Asia, with an estimated 16-20 million people affected by blindness. Angle closure is marked by apposition or synechiae between the trabecular meshwork and the iris, which are the major risk factor for primary angle-closure glaucoma [2-5]. Primary angle closure has two main mechanisms in the disease's progression: pupillary block and iris plateau. Increased resistance of aqueous humor outflow can lead to significant intraocular pressure increases, causing the progression of axonal damage and ganglion cell loss in the optic nerve head, causing vision impairment [2, 3, 5-7].
Laser peripheral iridotomy (LPI) is the primary management for angle-closure disease, aiming to widen the anterior chamber angle, thereby eliminating pupillary block, flattening the iris, and widening the anterior chamber angle. The LPI procedure is considered safe and effective, especially as a prophylactic therapy for primary angle closure and primary angle closure suspect [3, 6-8].
Examination of the anterior chamber angle through gonioscopy remains the gold standard. However, gonioscopy has limitations, including high inter-operator variability and the inability to quantitatively measure the anterior chamber angle. Spectral Domain Anterior Segment Optical Coherence Tomography (SD AS-OCT) is one modality for assessing the anatomical structure of the anterior chamber, providing high-resolution, detailed images in a single capture, independent of the operator. SD AS-OCT technology offers advantages in imaging, both qualitatively and quantitatively, with more accurate parameters such as trabecular iris space area (TISA) and angle opening distance (AOD) [4, 6, 7, 9-11]. This study aims to determine the differences in anterior chamber angle imaging results before and after LPI in angle-closure disease, as an effort to measure the procedure's effectiveness in handling angle-closure glaucoma.
2. MATERIALS AND METHODS
This analytical observational cross-sectional study consecutively enrolled patients diagnosed with primary angle closure (PAC), primary angle closure suspect (PACS), and primary angle-closure glaucoma (PACG). Comparative analysis was performed to evaluate the changes of anterior chamber angle structures, utilizing parameters such as Angle Opening Distance (AOD), Trabecular Iris Space Area (TISA), Anterior Chamber Depth (ACD), Anterior Chamber Width (ACW), Anterior Chamber Area (ACA), and Lens Vault (LV) before and after Laser Peripheral Iridotomy (LPI) in angle closure disease, using Spectral Domain Anterior Segment Optical Coherence Tomography (SD AS-OCT). The study included patients aged 40 to 70 years with PAC, PACS, and PACG. Patients with a history of intraocular surgery, history of laser treatment on the anterior segment previously, history of corneal abnormalities that can interfere with the visualization of SD AS-OCT and gonioscopy examinations, SD AS-OCT imaging results with non-visible scleral spur visualization that interfere measurement, or not completing the examination, were excluded.
The study was conducted at National Eye Center Cicendo Eye Hospital in Bandung, Indonesia, from January to February 2023. Ethical approval was granted by the Health Research Ethics Committee of National Eye Center Cicendo Eye Hospital Bandung with reference number LB.02.01/2.3/17866/2022, and written informed consent was obtained from all participants. This study was financially supported by research grant from National Eye Center Cicendo Eye Hospital with reference number HF.02.03/II/2.3/1197/2023.
All patients underwent comprehensive examination at the outpatient clinic, including medical history taking, assessment of eyeball position and movement, slit lamp biomicroscopy, Goldmann applanation tonometry, gonioscopy examination with Sussman gonioscope lens, and posterior pole examination with either a wide-field or 78D lens, followed by SD AS-OCT imaging. The clinical diagnosis was made by glaucoma consultant and all the imaging result was evaluated by glaucoma consultant for its eligibility of reading.
Laser peripheral iridotomy (LPI) was performed by one of two glaucoma consultants (MA/SU). Patients are administered 2% pilocarpine drops three times with 5-minute intervals, 1 hour before the laser procedure. The procedure was performed using an Abraham lens with the laser point between 10 and 2 o'clock on the thinnest part of the iris crypt, and power between 1 to 6 mJ with single burst pulse. The procedure was considered successful if signs of retro illumination are present, the anterior lens capsule is directly visible, or there is a burst of aqueous along with iris pigment. Intraocular pressure was monitored 1 hour after LPI using a Goldman applanation tonometer, and non-steroidal anti-inflammatory eye drops (sodium diclofenac) were prescribed four times daily for one week after LPI.
In the follow-up visit one week after the procedure, all patients underwent the same thorough ophthalmological examination as before, including iridotomy examination and SD AS-OCT imaging, to evaluate changes after LPI procedure.
Data are presented as percentages (%) and mean values ± standard deviation (SD). Statistical analyses were assessed with paired t-tests or Wilcoxon's alternative test, and p-value of <0.05 was considered significant. All collected data were recorded in a special form and processed with SPSS 24.0 version for Windows.
3. RESULTS
A total of 22 eyes from 22 patients with primary angle-closure disease met the inclusion and exclusion criteria for this study. Table 1 describes the characteristics of the subjects included in this study. The overall mean age of the study subjects was approximately 57.86 ± 7.624 years, with an age range of 42 to 70 years, and females dominated the study, comprising 90.9% of the subjects. There were 9 eyes (40.9%) with primary angle-closure suspect (PACS), 7 eyes (31.8%) with primary angle-closure (PAC), and 6 eyes (27.3%) with primary angle-closure glaucoma (PACG). For the uncorrected visual acuity (UCVA), 15 eyes (68.2%) with ≥ 6/12, 3 eyes (13.6%) with <6/12-6/18, 4 eyes (18.2%) with <6/18-6/60, and no patient with visual acuity less than 6/60. The Vertical Cup-Disc Ratio had an average of 0.40 ± 0.129. The mean number of anti-glaucoma medications used had an average of 0.50 ± 0.740.
The total energy used in patients undergoing LPI had an average of 38,33 ± 25,52 mJ. The average number of laser shots administered was 18,59 ± 12,09. This study found that 40.9% of the procedures were complicated by bleeding during the LPI, which was no longer active 1 hour after procedure.
The comparison of IOP values before, 1-hour after, and 1-week after LPI procedure were reported. There was a statistically significant decrease of IOP between before and 1-day after LPI, and also between before and 1-week after LPI, from 16,68 ± 3,657 mmHg to 14,68 ± 3,198 mmHg (p=0.025) and from 16,68 ± 3,657 mmHg to 13.59 ± 3.050 mmHg (p=0.001), respectively.
Fig. (1A, B) is an example of SD AS-OCT image in wide-field mode to assess AOD and TISA before and after LPI in one of the subjects. The image includes a legend to determine the position of nasal or temporal quadrants.
Tables 2 and 3 shows the comparison of temporal AOD and TISA values, nasal AOD and TISA values, and mean AOD and TISA values before and 1-week after LPI. The mentioned mean values are the averages of the nasal and temporal parameter measurements. There was a statistically significant increase in the mean values of the temporal AOD500, temporal AOD750, nasal AOD500, nasal AOD750, temporal TISA500, temporal TISA750, nasal TISA500, nasal TISA750, mean AOD500, mean AOD750, mean TISA500, and mean TISA750 before and 1-week post-LPI (p=0,0001 for all variables). The temporal AOD500, nasal AOD750, and mean AOD750 showed the largest T-value, indicating the most significant increase between before and after LPI.
| Variable | N = 22 |
|---|---|
| Age | - |
| Mean ± SD | 57,86 ± 7,624 |
| Median | 59,00 |
| Range (min-max) | 42,00 – 70,00 |
| Gender | - |
| Male | 2(9,1%) |
| Female | 20(90,9%) |
| Laterality | - |
| Right eye | 7(31,8%) |
| Left eye | 15(68,2%) |
| Uncorrected Visual Acuity | - |
| ≥6/12 | 15(68,2%) |
| <6/12-6/18 | 3(13,6%) |
| <6/18-6/60 | 4(18,2%) |
| <6/60-3/60 | 0(0.0%) |
| <3/60 | 0(0.0%) |
| Intraocular Pressure Pre-LPI | - |
| Mean ± SD | 16,68 ± 3,657 |
| Median | 16,00 |
| Range (min-max) | 10,00 – 26,00 |
| Vertical Cup-Disc Ratio | - |
| Mean ± SD | 0,40 ± 0,129 |
| Median | 0,40 |
| Range (min-max) | 0,30 – 0,80 |
| Diagnosis | - |
| PACS | 9(40.9%) |
| PAC | 7(31.8%) |
| PACG | 6(27.3%) |
| Number of anti-glaucoma medications used | - |
| Mean ± SD | 0,50 ± 0,740 |
| Median | 0,00 |
| Range (min-max) | 0,00 - 2,00 |
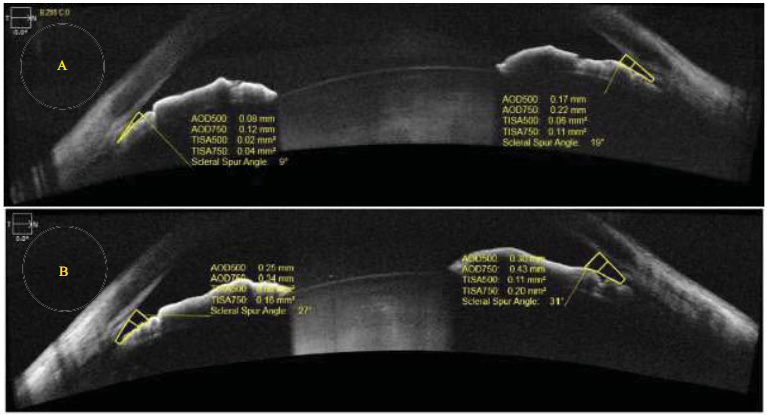
Wide-Field Mode SD AS-OCT Imaging Results Before (A) and 1-week After (B) LPI procedure.
AOD500/750, angle-opening distance (AOD), perpendicular distance measured from the trabecular meshwork at 500 and 750 μm anterior to the scleral spur along the anterior iris surface; TISA 500/750, trabecular-iris space area (TISA), trapezoidal area with 4 boundaries: the line segment of AOD, a line drawn from the scleral spur perpendicular to the plane of the inner scleral wall to the opposing iris, the corneoscleral wall, and anterior iris surface at 500/750 μm. [9].
Table 4 illustrates the comparison of ACD, LV, ACW, and ACA values before and 1-week after LPI. There is a statistically significant difference in the mean values of ACD, ACW, and ACA before and 1-week after LPI (p=0.006; p=0.001; p=0.049, respectively), but no statistical difference in the mean values of LV (p=0.770).
Fig. (2A, B) is an example of SD AS-OCT imaging in anterior chamber mode to assess ACD, LV, ACW, and ACA before and after LPI in one of the study subjects.
| Variable | Group | T-value / Z-score Wilcoxon | p-value | |
|---|---|---|---|---|
|
Pre-LPI (Mean±SD) |
1-week Post-LPI (Mean±SD) | |||
| N=22 | N=22 | |||
| Temporal AOD500a | 0,12 ± 0,074 | 0,22 ± 0,111 | 5,724 | 0,0001** |
| Temporal AOD750a | 0,20 ± 0,118 | 0,31 ± 0,143 | 4,328 | 0,0001** |
| Nasal AOD500b | 0,12 ± 0,070 | 0,22 ± 0,097 | 4,112 | 0,0001** |
| Nasal AOD750a | 0,20 ± 0,100 | 0,32 ± 0,144 | 5,235 | 0,0001** |
| Mean AOD500b | 0,12 ± 0,066 | 0,22 ± 0,091 | 4,015 | 0,0001** |
| Mean AOD750a | 0,20 ± 0,096 | 0,31 ± 0,144 | 6,349 | 0,0001** |
| Variable | Group | T-value / Z-score Wilcoxon | p-value | |
|---|---|---|---|---|
|
Pre-LPI (Mean±SD) |
1-week Post-LPI (Mean±SD) |
|||
| N=22 | N=22 | |||
| Temporal TISA500b | 0,05 ± 0,024 | 0,08 ± 0,042 | 3,596 | 0,0001** |
| Temporal TISA750a | 0,08 ± 0,044 | 0,14 ± 0,067 | 4,535 | 0,0001** |
| Nasal TISA500b | 0,04 ± 0,025 | 0,08 ± 0,039 | 4,030 | 0,0001** |
| Nasal TISA750b | 0,08 ± 0,045 | 0,14 ± 0,062 | 4,022 | 0,0001** |
| Mean TISA500b | 0,05 ± 0,022 | 0,08 ± 0,035 | 3,926 | 0,0001** |
| Mean TISA750b | 0,08 ± 0,038 | 0,14 ± 0,059 | 4,077 | 0,0001** |
| Variable | Group | p-value | |
|---|---|---|---|
|
Pre-LPI (Mean±SD) |
1-week Post-LPI (Mean±SD) |
||
| N=22 | N=22 | ||
| ACDa | 2,04 ± 0,292 | 2,07 ± 0,300 | 0,006* |
| LVb | 842,55 ± 195,596 | 843,77 ± 207,207 | 0,770 |
| ACWa | 10,84 ± 0,429 | 10,98 ± 0,395 | 0,001* |
| ACAb | 13,76 ± 3,026 | 13,69 ± 3,386 | 0,049* |
5. DISCUSSION
Angle-closure disease are characterized by iridotrabecular contact >180°, leading to obstruction of aqueous humor flow through the trabecular meshwork. Our study evaluated the effectiveness of LPI in 22 eyes who underwent LPI using SD AS-OCT. We found that there was a statistically significant difference in AOD, TISA, ACD, ACW, and ACA before and 1-week after LPI, with a predominance of female patients at 90.9% compared to 9.1% male, and the average age was 57.86 ± 7.624 years. This aligns with other previous studies that state the majority of angle-closure disease cases found in females. Females are more likely to have a shallow anterior chamber, a narrow angle of the chamber, and experience a more significant decrease in ACD as they age compared to males. Age is one of the contributing factors for the development of angle closure as the anterior chamber angle narrows with age due to lens thickening [3, 7, 12, 13].
Pupillary block is the main mechanism of angle closure due to resistance from aqueous humor at the pupil, increasing posterior chamber pressure, causing anterior iris bulging, and narrowing the anterior chamber angle. Laser peripheral iridotomy (LPI) is the primary management for angle closure, creating a full-thickness hole to eliminate pupillary block. Aqueous humor moves from the posterior to the anterior chamber across the LPI hole, equalizing pressures and pulling the iris down, thereby opening the anterior chamber angle. This study suggests the main mechanism in angle closure disease might be pupillary block, as there was a significant increase in AOD and TISA values before and after LPI on SD AS-OCT. Study by Jiang et al. in the ZAP trial study stated that the opening of the anterior chamber angle parameters after LPI was a result of the elimination of the pupillary block. Zebardast et al. reported an increase in AOD due to the flattening of iris curvature, widening the iridotrabecular contact, and increasing the anterior chamber angle. Radhakrishnan et al. in a literature review reported no increase in IOP > 21 mmHg from 326 eyes with PACS evaluated from 11 to 56 months after LPI procedure, with only about 44 eyes assessed up to 56 months requiring further therapy [6, 8, 14, 15].
This study found a statistically significant increase in AOD and TISA values across all quadrants after LPI, aligns with other study by Chen et al., Tun et al., Zebardast et al., and Meduri et al. The mean AOD750 showed the most significant increase between pre-LPI and post-LPI procedure. A study by Tun et al. reported a comparison of mean AOD750 pre-LPI at 0.2 ± 0.01 mm to 0.3 ± 0.01 mm after 1 week with a p-value < 0.001 and mean TISA750 pre-LPI at 0.1 ± 0.01 mm2 to 0.15 ± 0.01 mm2 after 1 week with a p-value < 0.001, assessed up to 3 months. For
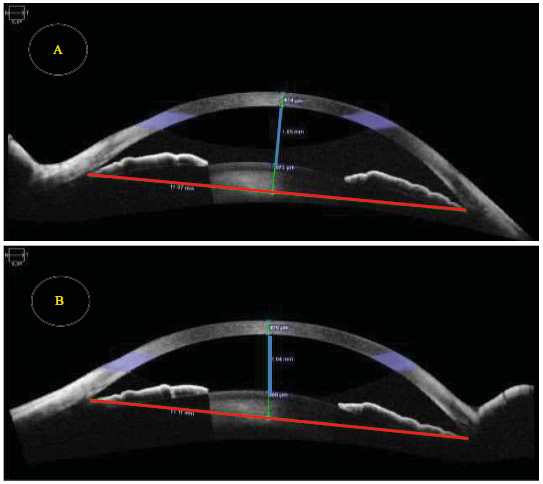
SD AS-OCT Imaging in Anterior Chamber Before (A) and 1-week After (B) LPI Procedure.
Anterior Chamber Area (ACA) represents the area of the anterior chamber; Anterior Chamber Width (ACW) is the distance between the scleral spurs marked by the red line; Anterior Chamber Depth (ACD) is the distance from the endothelium to the anterior lens capsule marked by the blue line; Lens Vault (LV) is the distance between the anterior lens capsule and the perpendicular line to ACW.
anterior chamber angle assessment up to 1 month, Koh et al. reported a significant increase in mean AOD750 from 0.48 ± 0.49 mm pre-LPI to 0.58 ± 0.35 mm after 1 month with a p-value of 0.024 and mean TISA750 from 0.21 ± 0.19 mm2 pre-LPI to 0.29 ± 0.18 mm2 after 1 month with a p-value of 0.001. Study by Meduri et al. reported a comparison of AOD and TISA parameters in the temporal, nasal, and mean quadrants similar to this study. The greatest increase was in temporal TISA500 from 0.06 ± 0.01 mm2 to 0.11 ± 0.06 mm2 (+45.5%) with a p-value < 0.001 and temporal TISA750 from 0.12 ± 0.04 mm2 to 0.16 ± 0.09 mm2 (+25.0%) with a p-value < 0.001, but no statistically significant increase was found in nasal AOD500, nasal TISA750, and mean TISA750. Other parameters from the study by Meduri et al. showed significant increases in temporal AOD500, temporal AOD750, nasal AOD750, mean AOD500, mean AOD750, nasal TISA500, and mean TISA500 [6, 8, 11, 12, 16, 17].
Consistent with the study by Moghimi, et al., our findings revealed no significant difference in the mean values of LV. This is in line with the results of the study by Yan, et al. which also revealed no significant alterations in LV after LPI, but did find a significant decrease in LV following lens extraction surgery. The lens vault measures the perpendicular distance between the anterior pole of the lens to a line drawn between the two scleral spurs. While pupillary block and plateau iris are the primary mechanisms in the mechanism of angle closure diseases, the position and relationship of the iris and lens also play critical roles. The lens can push the iris upward, reducing the gap between iris and lens. LPI restores the pupillary block condition, allowing aqueous humor to move from the posterior chamber to anterior chamber area, across peripheral iris hole, thereby widening the angle. However, LPI may not always be the effective management for all types of angle closure diseases, particularly in cases where pupillary block is not the main cause [18, 19].
This study observed a significant increase in AOD and TISA in the temporal quadrant, nasal quadrant, as well as their average, before and after LPI. Focusing solely on the nasal (0°) and temporal (180°) quadrants provides crucial insights into assessing the anterior chamber angle, leveraging advanced imaging technology in SD AS-OCT. This method is practical, dependable, and generates highly reproducible measurements, highlighting its utility in clinical evaluations. Tun et al. suggested AOD750 is a better diagnostic tool due to its alignment with gonioscopy results compared to TISA750, but measurements of AOD and TISA have limitations as these parameters only measure in one or two dimensions, not fully representing the condition of the entire anterior chamber angle. In the same study, Tun et al. conducted examinations taking slices every 11.25°, resulting in 16 image slices and performed 3-dimensional measurements through angle opening distance area (AODA) and trabecular-iris space volume (TISV), including volumes of TISA750, anterior chamber area (ACA), and iris volume (IV) in their formula calculations. Other studies have attempted to depict the anterior chamber angle condition in 360°, like Meduri et al., who took slices every 30°, resulting in 12 image slices and Kansara et al., who took vertical and horizontal slices, finding 7% were unassessable due to eyelid coverage, and measured 3-dimensional parameters such as trabecular-iris circumference volume (TICV) calculated with additional software [7, 12, 17, 20, 21]. This study has several limitations. First, the short follow-up time could not assess the progression in angle-closure disease after LPI. Second, this study does not compare the results of LPI between gonioscopy and SD AS-OCT. Third, this study does not evaluate the correlation among parameters.
In this study, we measured these parameters only before and after LPI procedure; we did not assess these parameters after cataract surgery. Future research is needed to evaluate these parameters after cataract surgery.
CONCLUSION
There were significant differences in the values of AOD, TISA, ACD, ACW, and ACA, and no significant difference in the value of LV one week after LPI in primary angle closure disease. SD AS-OCT can be used as a tool to assess the condition of the anterior chamber angle after LPI. Future studies should be conducted with extended follow-up time to assess the effects of LPI in preventing progression and acute incidents. Collecting a larger sample size could facilitate comparisons between PACS, PAC, and PACG. Correlations among parameters from SD AS-OCT could be assessed and compared in the evaluation of angle closure disease.
AUTHORS CONTRIBUTION
M.R., I.I., A.M.H.K., R.V.: Study conception and design; R.F.R.: Data collection; S.U., A.P.: Analysis and interpretation of results; I.N.: Draft manuscript.
LIST OF ABBREVIATIONS
| LPI | = Laser Peripheral Iridotomy |
| SD AS-OCT | = Spectral Domain Anterior Segment Optical Coherence Tomography |
| AOD | = Angle Opening Distance |
| TISA | = Trabecular Iris Space Area |
| ACD | = Anterior Chamber Depth |
| ACW | = Anterior Chamber Width |
| ACA | = Anterior Chamber Area |
| LV | = Lens Vault |
| PAC | = Primary Angle Closure |
| PACS | = Primary Angle Closure Suspect |
| PACG | = Primary Angle-Closure Glaucoma |
| IOP | = Intraocular Pressure |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was granted by the Health Research Ethics Committee of National Eye Center Cicendo Eye Hospital Bandung, Indonesia with reference number LB.02.01/2.3/17866/2022.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIAL
The data supporting the findings of the article is available in Zenodo Repository at https://doi.org/10.5281/zenodo.13951823.
FUNDING
This study was funded by Cicendo Eye Hospital, Indonesia Awards/Grant number: (HF.02.03/II/2.3/1197/2023).
ACKNOWLEDGEMENTS
Declared none.


