All published articles of this journal are available on ScienceDirect.
Efficacy of Argon Laser Photoablation for Conjunctival Cysts
Abstract
Purpose
This paper aims to study the efficacy and safety of argon laser photoablation for conjunctival cysts.
Methods
A retrospective chart was reviewed in 23 eyes of 23 patients receiving argon laser photoablation to treat conjunctival cysts at Quzhou People’s Hospital from December 2020 to February 2023. Results of success rate, subconjunctival hemorrhage, conjunctival scarring and ocular irritation were recorded for analysis.
Results
All patients were followed up for 12 months. Complete resolution occurred after a single laser session in 19 eyes (82.6%). Two cases succeeded after the second laser treatment (the final success rate was 91.3%). One case recurred again after the second laser session, but it was smaller than before, and he refused treatment again. One case stopped laser photoablation for massive subconjunctival hemorrhage during treatment, and she chose surgical excision later on. No conjunctival granuloma was observed after argon laser photoablation. Ocular irritation usually disappears within one week.
Conclusion
Argon laser photoablation is a safe and effective treatment for conjunctival cysts in an outpatient clinic, especially for small fixed cysts.
1. INTRODUCTION
Conjunctival cysts are sac-like lesions with a thin wall ocular surface [1, 2], most of which occur spontaneously, some after ocular surface trauma or ophthalmic surgery [3]. Most patients with conjunctival cysts are asymptomatic. However, others may have symptoms such as foreign-body sensation, blurred vision, and dry eye due to unstable tear film as their size increases [4, 5].
Needling and simple aspiration is performed frequently in an outpatient clinic [6], but is associated with a high rate of recurrence because the inner epithelial lining of the cyst remains. The traditional treatment is conjunctival cyst surgical excision, which is performed to minimize recurrence [7], but because the wall of the conjunctival cyst is very thin, the cyst is easy to rupture during the operation. The boundary of the cyst is unclear, so it is difficult to remove it completely. Partial residual cyst wall will lead to recurrence, and some operators use viscoelastic, trypan blue, or indocyanine green to assist cyst excision [7, 8]. Surgery requires higher costs and resources, often necessitating routine laboratory tests and a hospital stay.
The argon laser is one of the most widely used laser types in the ophthalmic field, which was used in retinal photocoagulation, peripheral iridoplasty, and trichiasis because of its convenience, effectiveness, and safety [9, 10]. Han et al. reported a conjunctival cyst was successfully removed by argon laser using the mechanism of thermal photoablation of the cyst wall [11]. Subsequently, another study reported a modified argon laser photoablation for conjunctival cysts by staining the conjunctival cyst surface to increase the absorption of thermal laser energy [12]. Our prospective study using this method was conducted at Quzhou People’s Hospital between December 2020 and February 2023, aiming to evaluate the efficacy of argon laser photoablation as a modality of treatment for conjunctival cysts.
2. SUBJECTS AND METHODS
2.1. Participants
This simple descriptive study included 23 patients diagnosed with conjunctival cysts and underwent argon laser photoablation of conjunctival cysts at Quzhou People’s Hospital. The study followed the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of Quzhou People’s Hospital. Informed consent was obtained from each patient before treatment. Routine anterior segment photography, best-corrected visual acuity (BCVA), intraocular pressure (IOP) and other general examinations were acquired before treatment.
2.2. Treatment
In the outpatient treatment room, topical anesthesia was given with 0.5% proparacaine hydrochloride. Periocular skin and conjunctival sac disinfection with povidone-iodine solution were applied. The patient was instructed to move their eyes until the conjunctival cyst was centered in the slit lamp microscope’s field of view. The surface of the conjunctival cyst was marked with a skin marker pen under a slit lamp microscope, and the conjunctival cyst was punctured with a 26-gauge needle to drain the fluid. The 532 argon laser therapy instrument (Visulas 532 s; Carl Zeiss Meditec, Jena, Germany) was used to perform argon laser photoablation of the cyst epithelium on the marked area (500 µm spot size, 0.3 seconds duration and 200~300 Watt power). After the laser spot covered the entire surface of the conjunctival cyst, a wet cotton swab was used to wipe off the conjunctiva damaged by laser photoablation. The overall treatment process is shown in Fig. (1). After treatment, topical 1% tobramycin-dexamethasone eye drops were administered 4 times daily for one week.
2.3. Outcome Measures
Patients received regular follow-up examinations at 1 week, 1, 6, and 12 months after the treatment. After 12 months, the patients were asked to visit when needed. The rate of recurrence of conjunctival cyst, subconjunctival hemorrhage, conjunctival scar, and foreign body sensation were recorded.
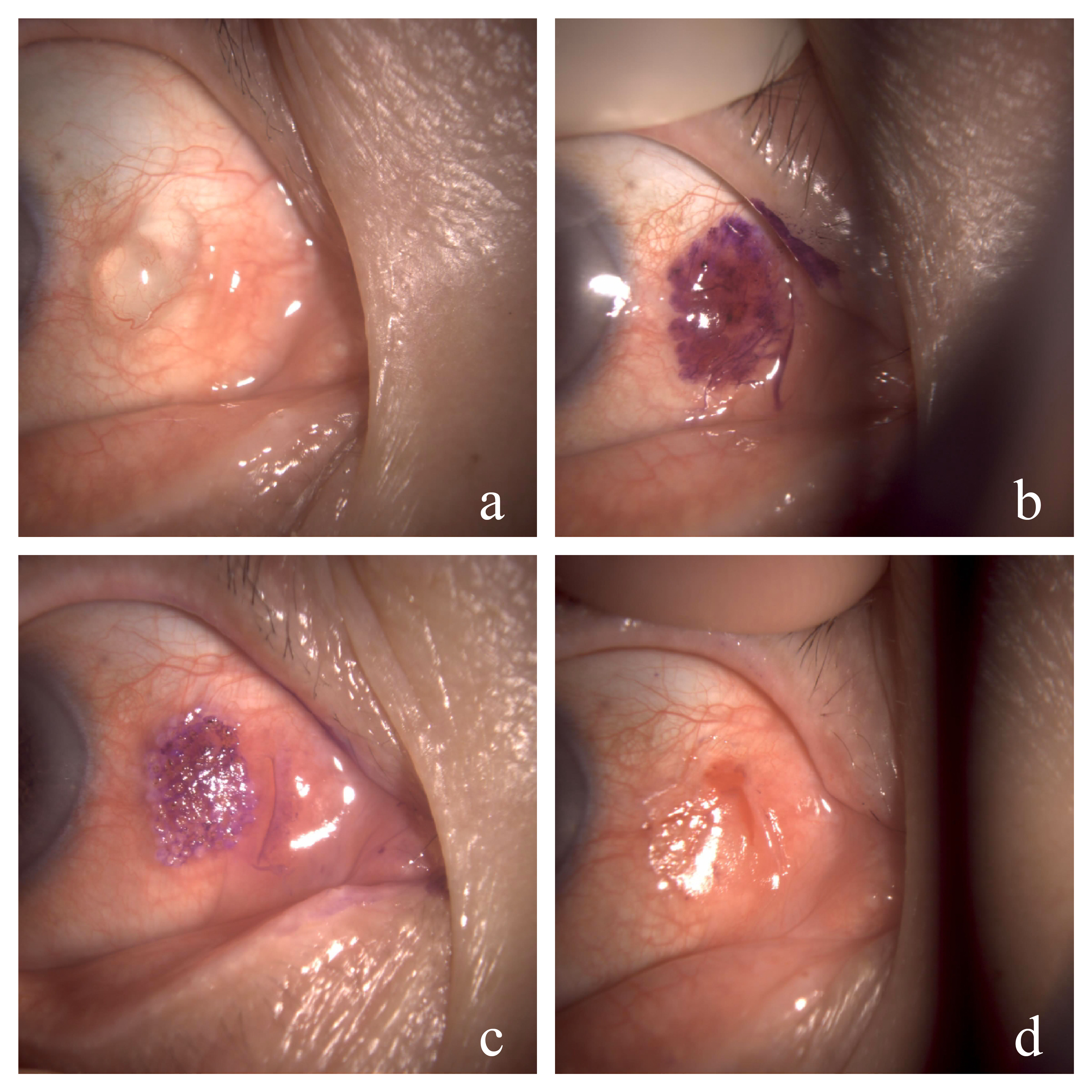
The procedure of argon laser photoablation of conjunctival cysts. (a) The conjunctival cyst before treatment, (b) The surface of the conjunctival cyst staining by skin marker pen after draining the fluid from the cyst by needle puncture, (c) Argon laser photoablation of conjunctival cyst on the marked area, (d) The appearance of the conjunctiva damaged by laser photoablation after wiping off by wet cotton swab.
3. RESULT
There were 23 eyes of 23 patients (6 men and 17 women, mean age 55.6±10.2 years) included. The mean size of the long diameter of the cysts was 4.9±1.7mm. After 12 months of follow-up, there were no significant changes in BCVA and IOP. Nineteen patients (82.6%) were successfully treated with a single laser session, and mild conjunctival scarring was observed after argon laser photoablation (Fig. 2), but no conjunctival granuloma was observed. The foreign body sensation generally disappeared within one week. Recurrent patients were generally smaller and more fixed than before, and the fixed small cysts were more convenient for retreatment because the position of fixed small cysts remained unchanged during the treatment process (Fig. 3). Among them, 2 cases were cured by argon laser retreatment (the final success rate was 91.3%). One case still relapsed after the second laser session, but it was smaller than before and with no discomfort, so she refused to be treated again. One case had a massive subconjunctival hemorrhage during acupuncture, which made subsequent laser treatment difficult to complete, and she chose surgical excision later on.
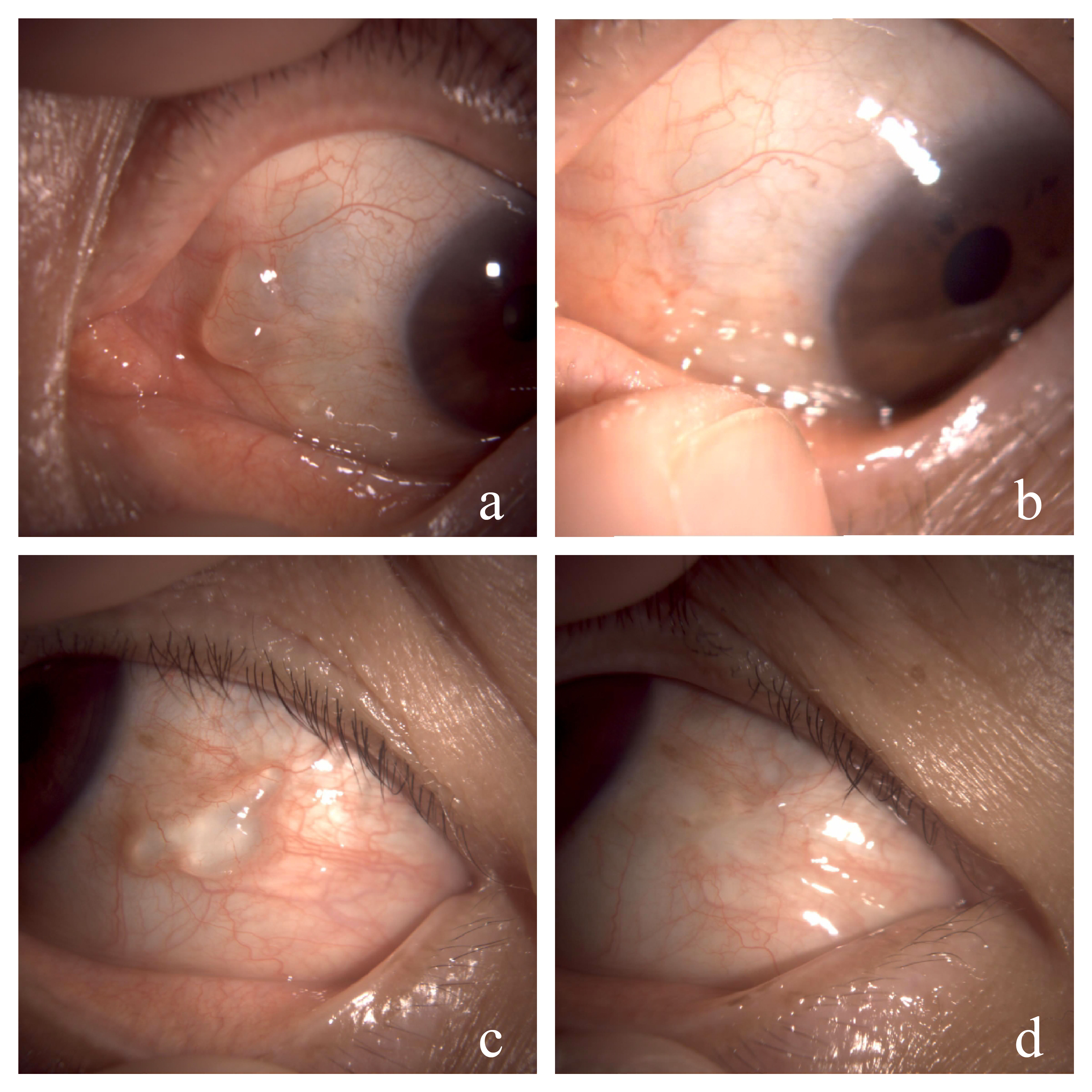
Examples of argon laser photoablation of conjunctival cysts. (a and c) Pre-operative appearance, (b and d) Twelve-month postoperative appearance.
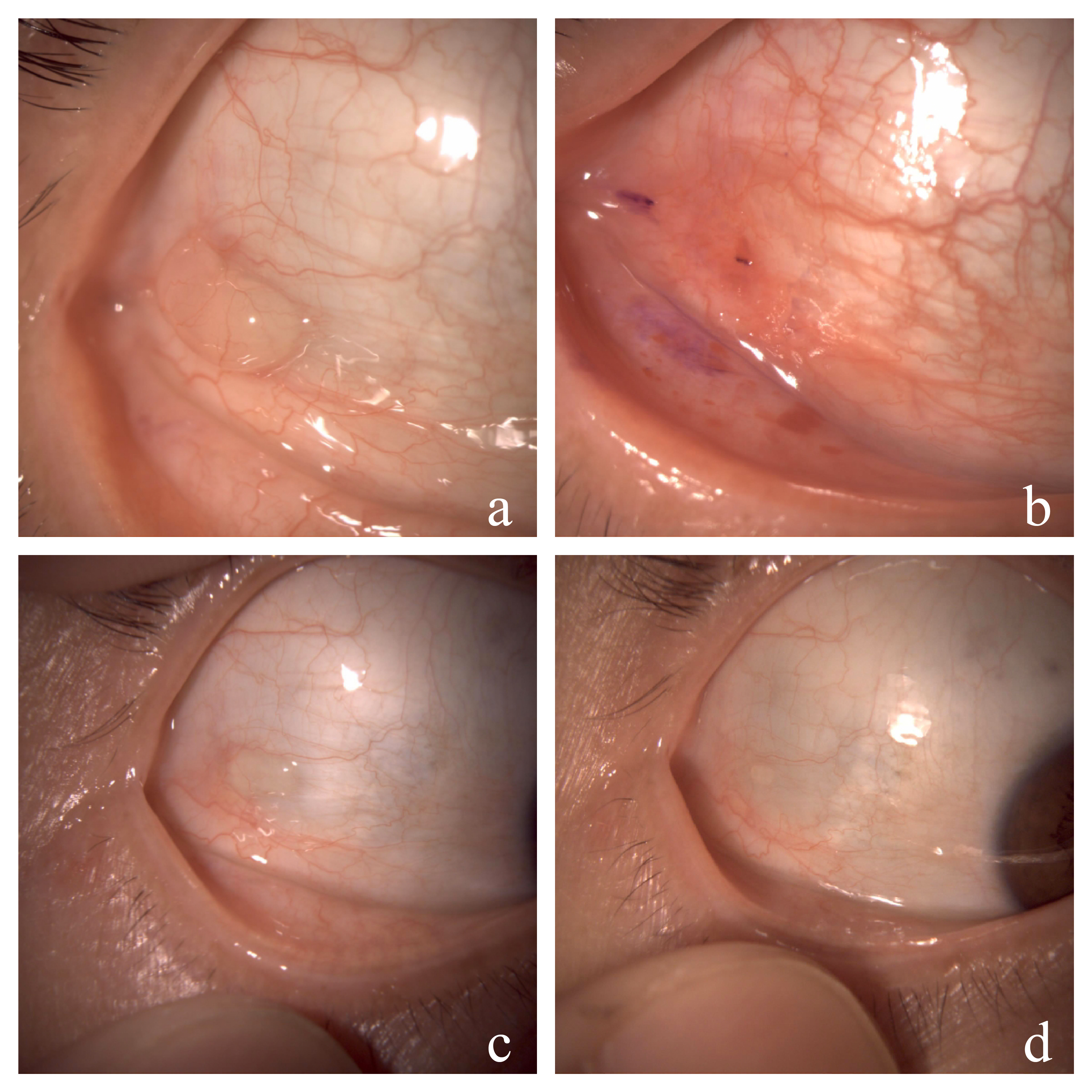
A case of recurrent conjunctival cyst. (a) Pre-operative appearance, (b) The appearance of the first argon laser photoablation, (c) Recurrent conjunctival cyst two weeks later, (d) Twelve-month postoperative appearance of retreatment.
4. DISCUSSION
Simple aspiration and surgical excision are two common procedures for removing conjunctival cysts, but each method may have limitations [6, 7]. Simple aspiration is an office-based procedure, but associated with a high recurrence rate. Surgical excision is a standard invasive method with a lower recurrence rate, in which incision, hemostasis, and suture are required in the operating room. Argon lasers are effective coagulating instruments that are easy to apply in outpatient clinics. Argon laser photocoagulation has been used to treat various conjunctival diseases, such as conjunctival nevus [13, 14], pinguecula [15, 16], and conjunctivochalasis [17, 18]. In 2012, Han et al. first reported a case of conjunctival cyst that was successfully treated by argon laser in an outpatient clinic [11]. Later, in 2020, a study reported a modified method in which argon laser treatment was performed after staining the surface of conjunctival cysts to enhance the absorption of thermal laser energy [12]. The success rate of a single laser session was 82.35% (14/17). Among them, 3 relapsed patients were cured by laser retreatment (100%) [13]. We used the same method to treat 27 cases of conjunctival cysts, and the success rate of a single laser session was 82.6% (19/23), which was similar to the previous research results.
Histologically, the conjunctival cyst includes the wall and the surface composed of non-keratinized squamous epithelium, and goblet cells appear as epithelial cells in its wall [1]. The conjunctival cyst wall is thin; after draining the fluid from the cyst by needle puncture and staining the surface with a dark purple marker pen, the thermal energy of the argon laser can be effectively transferred to the conjunctiva and the underlying cyst to ablate the epithelial cells of the cyst [12]. At the same time, during the healing process, the inner surface of the cyst wall adheres firmly to the surrounding tissue, making it difficult for the secreted fluid to reaccumulate. The recurrence cysts were usually fixed, localized small cysts, which were easier to retreat because the position of fixed small cysts remains unchanged during the treatment process, and the treatment range is exact. While the position of mobile cysts may change during acupuncture, leading to the marked range may not cover the exact range of conjunctival cysts, which may affect the laser treatment and cause the recurrence of cysts. In our study, the 2 cases of recurrent conjunctival cysts were small fixed cysts, which were successfully resolved after the second laser session. Therefore, argon laser photoablation is especially suitable for small fixed conjunctival cysts.
The main complication of this treatment was subconjunctival hemorrhage caused by accidentally injuring blood vessels during acupuncture. Still, most of them were small pieces of bleeding, which could be stopped by compression and generally did not affect subsequent laser treatment. In one patient, a massive subconjunctival hemorrhage formed a blood pack during acupuncture, which made subsequent laser treatment difficult to complete. Patients need to be informed that conjunctival hemorrhage is a common complication, which can affect the appearance of the eye but can be absorbed by itself to avoid unnecessary stress. No conjunctival granuloma was observed after argon laser photoablation. Most patients had foreign body sensations after treatment, which may be caused by the mild conjunctiva scars. The heat of the laser is transferred from the surface of the conjunctiva to the subconjunctiva, resulting in damage and loss of the conjunctiva epithelium and degeneration of the subconjunctiva tissue, which may lead to conjunctiva scar. However, the foreign body sensations usually disappear within one week, and artificial tears may be needed for sensitive patients.
CONCLUSION
In summary, argon laser photoablation of conjunctival cysts is safe and effective, and it can be done in the office setting, especially suitable for small fixed conjunctival cysts.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| BCVA | = Best-corrected Visual Acuity |
| IOP | = Intraocular Pressure |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This retrospective study was approved by the Ethics Committee of Quzhou People’s Hospital, China (application number 2021-05-051).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
This study was supported by the Research Foundation of Quzhou People’s Hospital (No.YNB20 to GH Chen) and Quzhou Science and Technology Project (No.2023ZD034 to GH Chen).
ACKNOWLEDGEMENTS
Declared none.


