All published articles of this journal are available on ScienceDirect.
Prevalence and Characteristics of Ocular and Systemic Manifestations in Iraqi Patients with Behçet’s Disease
Abstract
Objectives
This prospective study aimed to ascertain the prevalence of ocular and systemic manifestations among Iraqi patients diagnosed with Behçet’s disease. Patients underwent comprehensive evaluations, including HLA-B51 and Pathergy tests.
Methods
The study enrolled patients diagnosed with Behçet’s disease, who were examined at the Ophthalmology Department of Baghdad Medical City between November 2019 and September 2022. Examinations included slit lamp biomicroscopy and indirect ophthalmoscopy. Additionally, patients underwent HLA-B51 and pathergy testing.
Results
Out of the 76 patients enrolled, ocular involvement was observed in 50 patients (66%). Specifically, 48% presented with anterior uveitis, 40% with vitritis, 8% with retinitis, 34% with retinal vasculitis, and 8% with papillitis. Systemic involvement was prevalent, with 100% exhibiting oral ulceration, 74% genital ulceration, 50% arthritis, 16% skin lesions, 8% venous complications (such as DVT), and 4% gastrointestinal ulceration. HLA-B51 tested positive in 54% of patients, while the pathergy test yielded positive results in 36%.
Conclusion
Non-granulomatous anterior uveitis (48%) and vitritis (40%) emerge as the most prevalent ocular manifestations in Iraqi patients with Behçet’s disease. Oral (100%) and genital (74%) ulceration stand out as the predominant systemic features.
1. INTRODUCTION
Behçet’s disease is a systemic vasculitis most common in individuals of Mediterranean and Eastern origin, though it also affects Caucasians. The etiology remains unknown, but a widely held hypothesis is that a profound inflammatory response is triggered by an infectious agent in a genetically susceptible host. This is supported by the consistent association of disease susceptibility with HLA B51 [1-3].
Diagnostic criteria for Behçet’s disease (International Study Group for Behçet’s Disease) include recurrent oral ulceration (at least three times per year) plus two of the following: genital ulceration, ocular inflammation, skin lesions (e.g., erythema nodosum and acneiform lesions), and a positive pathergy skin test [4].
1.1. Clinical Features
1.1.1. Eye Disease
Ocular involvement is reported in 30-70% of patients with Behçet’s disease. It often involves chronic, relapsing bilateral uveitis affecting both the anterior and posterior uveal tracts. Anterior uveitis with hypopyon is characteristic, along with posterior uveitis and retinal vasculitis. Other lesions include iridocyclitis, scleritis, keratitis, vitreous hemorrhage, optic neuritis, retinal vein occlusion, and retinal neovascularization. Eye disease tends to be less severe in the United States than in Japan or the Middle East [5-8].
1.1.2. Recurrent Aphthous Ulceration
This is the sine qua non of Behçet’s disease. Genital ulcers occur in 72-94% of cases and are similar in morphology to oral ulcers [9].
1.1.3. Skin Disease
It is present in about 80% of patients, including erythema nodosum, papulopustular lesions, and acneiform nodules. Pathergy is positive in 60% of Middle Eastern populations, 15% in Koreans, and only 5% in Caucasians [9-11].
1.1.4. Articular Disease
Joint manifestations are prevalent, affecting nearly two-thirds (approximately 65%) of patients, with a predilection for the knees, ankles, and wrists [5, 12, 13].
1.1.5. Vascular Disease
It is considered as a systemic vasculitis that involves both arteries and veins, manifesting as a vascular disease in a considerable proportion of patients, with a reported prevalence ranging from 7% to 49% [12].
1.1.6. Gastrointestinal Disease
Gastrointestinal involvement exhibits substantial variability, with a notably higher prevalence observed in Japan compared to Turkey [14].
1.1.7. CNS Involvement
Neurological involvement in Behçet’s disease, also known as Neuro-Behçet’s syndrome (NBS), affects about 5-10% of patients. This form of involvement is more frequently observed in Europe and the United States compared to the Middle East [15].
2. METHODS
Patients diagnosed with Behçet’s disease were evaluated at the outpatient clinic of the Ophthalmology Department at Baghdad Medical City between November 2019 and September 2022. Referrals to this department were made from the dedicated Behçet’s disease clinic at Baghdad Teaching Hospital within the Medical City complex.
Data collection included comprehensive medical history, demographic details (age, gender), anterior segment examination using slit lamp biomicroscopy, posterior segment evaluation via indirect ophthalmoscopy, Snellen visual acuity assessment, intraocular pressure (IOP) measurement using air-puff and Goldmann tonometry, and systemic examination for associated features. All patients underwent HLA-B51 testing and pathergy testing.
The Behçet’s disease clinic at Baghdad Medical City serves as the primary referral center in Iraq for the diagnosis and management of Behçet’s disease. Patients are routinely directed to the Ophthalmology Department within the medical complex for the diagnosis and treatment of ocular involvement, both at the time of initial diagnosis and during subsequent follow-up appointments. This study adhered to the principles outlined in the Declaration of Helsinki. It was conducted after gaining approval from the Ethics Committee on Human Research in Baghdad Medical City (Approval No. 221 on the 10th of March 2019). Additionally, both verbal and signed informed consent forms were obtained from the patients before they participated in the study. All data were kept anonymous, and no divulging of information occurred; it was only for research purposes.
3. RESULTS
A total of 76 patients with Behçet’s disease were included in the study. Oral ulceration was observed in all patients (100%, n=76), making it the most common manifestation. Genital ulceration was present in 56 patients (74%). Ocular involvement was noted in 50 patients (66%). Arthritis affected 37 patients (48%), and skin lesions were seen in 12 patients (16%). Venous involvement was identified in 6 patients (8%), gastrointestinal ulceration in 3 patients (4%), and neurological involvement also in 3 patients (4%). The prevalence of HLA-B51 positivity was found in 41 patients (54%), and the pathergy test was positive in 27 patients (36%) (Table 1).
Among the 50 patients with ocular involvement, bilateral manifestations were observed in 37 patients (74%), while 13 patients (26%) had unilateral involvement. Of the bilateral cases, 19 (38%) were symmetric, and 18 (36%) were asymmetric. Non-granulomatous anterior uveitis was detected in 24 patients (48%). Vitritis was found in 20 patients (40%); vitritis was defined using the Standardization of Uveitis Nomenclature (SUN) guidelines, which grades vitreous haze from 0 (no haze) to +4 (severe haze). Retinal vasculitis was observed in 17 patients (34%) (Fig. 1), retinitis was observed in 4 patients (8%), and hypopyon was observed in 3 patients (6%) (Table 2, Fig. (2)). These findings highlighted the diverse ocular manifestations that can occur in Behçet’s disease.
| Type of Manifestation | Number of Patients (out of 76) | Percentage |
|---|---|---|
| HLA- B 51 | 41 | 54% |
| Pathergy test | 27 | 36% |
| Ocular involvement | 50 | 66% |
| Oral ulceration | 76 | 100% |
| Genital ulceration | 56 | 74% |
| Venous involvement | 6 | 8% |
| Skin lesions | 12 | 16% |
| Neurological involvement | 3 | 4% |
| Arthritis | 37 | 48% |
| GIT ulceration | 3 | 4% |
| - | Number of Patients (out of 50) | Percentage |
|---|---|---|
| Anterior uveitis | 24 | 48% |
| Hypopyon | 3 | 6% |
| Vitritis | 20 | 40% |
| Retinitis | 4 | 8% |
| Retinal vasculitis | 17 | 34% |
| Papillitis | 4 | 8% |
| Bilateral involvement | 37 | 74% |
| - Symmetric | 19 | 38% |
| - Asymmetric | 18 | 36% |
| Unilateral involvement | 13 | 26% |
Regarding gender distribution, 62% of the patients were male (n=47), and 38% were female (n=29), resulting in a male-to-female ratio of approximately 3:2 (Table 3). This distribution indicates a higher prevalence of Behçet’s disease among males in the studied population.
4. DISCUSSION
The male to female ratio in our study was approximately 3:2, aligning well with the gender distribution observed in Eastern Mediterranean populations. This contrasts with Far Eastern Asian populations, where females are more frequently affected [16, 17].
Ocular involvement was observed in 66% of the patients, which falls within the global range of 30-70% and is fairly close to the rate in Turkey (80%) (Tugal-Tutkun et al.) [6]. In comparison, the rate is 65% in the Saudi population and 55% in Iran (El-Asrar et al., Davatchi et al.) [5, 18]. Anterior uveitis, vitritis, and retinal vasculitis appeared at relatively similar rates in this study compared to Turkish figures (45%, 40%, and 27%, respectively) and Iranian statistics (41%, 44%, and 30%, respectively) (Gul, Davatchi et al.) [5, 17]. Hypopyon was observed in 6% of the patients, which is lower than the rates typically reported in other populations. Both retinitis and papillitis were found at much lower rates. The smaller number of patients in this study might have played a role, or this may reflect different rates of ocular manifestations in the populations studied [5, 6, 17, 18].

Fundus fluorescein angiography show vasculitis.
HLA-B51 was found positive in 54% of patients in this study, compared to 47% in the Turkish population and 33.9% in Iran (Davatchi et al.) [5]. The pathergy test was positive in 36% of patients, falling within the global range of 15-60%, with a rate of 57% in Iran [19, 4].
Arthritis, vascular disease, and genital ulceration were found at rates similar to those reported globally in Turkey, Saudi Arabia, and Iran (Davatchi et al., Kural-Seyahi et al.) [5]. Neurological symptoms were reported in 4% of the cases in this study, while the global rate is 5-10%, 3.2% in Iran, 0.2% in Turkey, and an unusually high 44% in Saudi Arabia (Al-Araji & Kidd, Siva et al.) [20, 21].
Skin lesions were reported in only 16% of patients compared to 80% globally, 69% in Iran, 57% in Saudi Arabia, and 27% in Turkey (Davatchi et al., Gul, Seyahi et al.) [5, 17, 22, 23]. The smaller number of patients in this study likely influenced these discrepancies. Additionally, the fact that this is a hospital-based study might have contributed to the differences observed, or it may reflect different tendencies in the Iraqi population.
A trend was observed where patients with severe systemic symptoms, such as recurrent and extensive genital ulceration, exhibited more severe ocular involvement (e.g., retinal vasculitis and vitritis). However, statistical significance could not be established due to the limited sample size. This observation warrants further investigation in larger cohort studies.
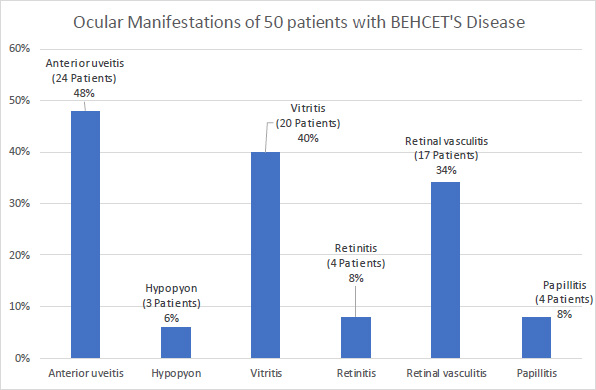
Ocular manifestations of 50 Iraqi patients with behçet’s disease.
| Gender | Number (out of 76) | Percentage |
|---|---|---|
| Male | 47 | 62% |
| Female | 29 | 38% |
CONCLUSION
Our study sheds light on the diverse spectrum of ocular and systemic manifestations observed in Iraqi patients with Behçet's disease. Notably, we found that non-granulomatous anterior uveitis (48%) and vitritis (40%) emerged as the most prevalent ocular features, underlining the significant burden of ocular involvement in this population.
Moreover, our findings highlighted the predominant systemic manifestations of Behçet's disease among Iraqi patients. Oral ulceration was universally present, observed in 100% of cases, underscoring its diagnostic significance and the immense impact it has on patients' quality of life. Additionally, genital ulceration was prevalent in 74% of patients, further emphasizing the multisystemic nature of the disease.
These insights contribute to a deeper understanding of Behçet's disease in the Iraqi population, providing valuable clinical data that can inform more targeted and effective management strategies. Further research and collaborative efforts are warranted to elucidate the underlying mechanisms driving these manifestations and to optimize therapeutic interventions tailored to the specific needs of Iraqi patients with Behçet's disease.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| NBS | = Neuro-Behçet’s syndrome |
| IOP | = Intraocular pressure |
| SUN | = Standardization of Uveitis Nomenclature |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
It was conducted after gaining approval from the Ethics Committee on Human Research in Baghdad Medical City, Iraq (Approval No. 221 on the 10th of March 2019).
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Both verbal and signed informed consent forms were obtained from the patients before they participated in the study.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
Declared none.


