All published articles of this journal are available on ScienceDirect.
An Asymptomatic Metallic Foreign Body Retained in the Subconjunctival Space for over 50 Years: A Rare Case Report
Abstract
Introduction
Failure to promptly remove an ocular foreign body, particularly a metallic fragment, is often associated with the development of inflammation, infection, or granuloma formation. However, this report presents a rare case of a metallic foreign body that remained within the subconjunctival space for over 50 years without significant ocular complications.
Case Presentation
An 80-year-old woman presented with a complaint of blurred vision in both eyes. In slit-lamp examination, the cataract bilaterally and incidentally revealed the presence of a tiny black foreign body within the subconjunctival space in the left eye. No further abnormal findings were observed in the fundus and extraocular components in both eyes. After inquiring about the patient's history of trauma, it was revealed that over 50 years ago, the patient experienced an ocular injury from a shard of iron while working at a factory. Given the impending cataract surgery and associated risks, the subconjunctival foreign body was removed under topical anesthesia in the operating room and identified as a magnetic metal fragment. At the 1-month follow-up, the patient had fully recovered from the incision site, with no observed adverse effects.
Conclusion
In this case, there appear to be no severe consequences associated with the long-term retention of a subconjunctival metallic foreign body. Nonetheless, it is imperative to conduct meticulous patient evaluations and interventions to mitigate the potential risk of injury.
1. INTRODUCTION
Ocular foreign body injuries are highly common in industrial workplace settings [1]. Foreign bodies located on the superficial conjunctiva and cornea are usually easily identifiable and removable. However, depending on the impact force, foreign bodies (FB) can also penetrate varying depths of ocular tissues, potentially lodging either extraocularly or intraocularly. Most cases are promptly identified and managed due to characteristic symptoms, such as pain, redness, tearing, blurred vision, and the risk of infection [2-9]. Nonetheless, small penetrating foreign bodies may be overlooked if a comprehensive assessment is not conducted, particularly when concealed by significant subconjunctival hemorrhage or conjunctival congestion. In rare instances, the foreign body may remain asymptomatic and undetected for prolonged periods [10-14]. Here, we document a rare case of an incidentally discovered subconjunctival metallic foreign body retained for more than 50 years without pronounced clinical consequences.
2. CASE PRESENTATION
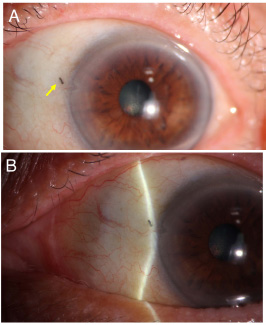
An 80 year-old woman attended the clinic with a chief complaint of decreased vision in both eyes for a couple of days. On presentation, she had a BCVA of 20/25 in the right eye and 20/20 in the left eye with normal intraocular pressure. The slit-lamp examination revealed a minute metal-like foreign body located in the subconjunctival space adjacent to the nasal limbus of the left eye, with the conjunctiva appearing white and undisturbed. Additionally, a minor wedge-shaped defect was observed in the limbus near the site of the foreign body (Fig. 1). Upon eyelid eversion, no foreign bodies were identified in the upper and lower tarsal conjunctiva or the fornix. The anterior chamber of both eyes exhibited transparency without the presence of cells or flare. Pupils displayed round morphology with normal light reflexes, and no evident transillumination defects were observed in both eyes. No synechia was found, and symmetrical cataracts were noted bilaterally. Subsequent examination of the fundus after pupil dilation revealed no anomalies in the posterior and peripheral retina and choroid. The patient's ocular motility was within normal limits. Upon further inquiry into the patient's traumatic history, she recalled a work-related injury that occurred over 50 years ago while engaged in unprotected iron casting work in a factory, leading to ocular trauma from a metallic fragment in her left eye. Fortunately, her visual acuity remained unaffected at that time, and she only received prompt eye irrigation at a local clinic, with no remarkable subsequent manifestations of discomfort. Additionally, she also denied any history of other ocular diseases or trauma over the past 50 years.

Considering the potential risks associated with the metallic foreign body for subsequent cataract surgery, the foreign body was removed. Following topical anesthesia, an incision was made in the conjunctiva near the foreign body for exploration, unveiling the foreign body's position between the conjunctiva and Tenon's capsule. The piece of foreign body fragmented upon attempted extraction with forceps (Fig. 2). However, complete removal was successfully achieved, with no residual fragments identified. Moreover, no scleral defects and siderosis were noted underneath. Using a magnet bar, the magnetic attraction test for extracted foreign body fragments was positive, which confirmed that the foreign body was composed of magnetic metal. The patient was routinely administered postoperative topical antibiotics and corticosteroids. At the 1-month follow-up, the patient had fully recovered from the incision site, with no observed adverse effects.
3. DISCUSSION
Work related injuries are the most common type of ocular trauma, with ocular foreign body injuries being one of the most common workplace injuries [1]. The location of the foreign body in the eye can greatly impact the severity of visual and functional impairments. Timely removal of foreign bodies, reducing the risk of prolonged exposure and subsequent damage to the ocular tissues, offers a better visual prognosis. The identification of foreign bodies, particularly those of small size and lacking symptoms of pain or visual impairment, as in this case, can be challenging without prompt medical attention and comprehensive assessment. A few previous reports of asymptomatic intraocular foreign bodies suggest a potential role of the eye's innate defense mechanisms, such as encapsulating and isolating foreign objects, leading to tolerance of such entities over time [11, 13]. We postulate that the long-term ocular tolerance observed in this patient may be attributed to the sealing and isolation of the foreign object by the conjunctival tissue. The management of asymptomatic extraocular foreign bodies should be determined on a case-by-case basis. Some clinicians have challenged the conventional approach of immediate foreign object removal, advocating instead for a conservative strategy of observation and monitoring in cases where the extraocular foreign body does not induce significant symptoms or complications, especially when the risks associated with surgical removal are higher [14, 15]. However, in our case, the extended presence of the metallic foreign body in the subconjunctival space has led to a significant increase in its fragility, suggesting a progressive alteration of its properties. Moreover, the long standing metallic foreign bodies in the ocular region carry potential risks and unforeseeable hazards. Several reports have detailed cases in which patients undergoing MRI examinations for unrelated medical conditions experienced image distortion or discomfort in the eye, revealing that these issues were caused by previously unnoticed ocular metallic foreign bodies that had become magnetized and undergone displacement during the MRI scan, consequently leading to ocular injury [16-18]. To this end, the removal of the subconjunctival metallic foreign body through thorough exploration is the optimal strategy to minimize the potential risk of secondary ocular injuries. In this instance, the extraction of the foreign body was relatively straightforward. Postoperatively, the patient maintained a BCVA of 20/25 in the left eye, with no observed adverse effects. Future management considerations for the patient include cataract surgery to address the painless visual blur in both eyes.
CONCLUSION
This case highlights that a tiny subconjunctival metallic foreign body can be asymptomatic and well-tolerated over an extended period in the absence of infection and inflammation. A comprehensive examination of the ocular surface is crucial for detecting any retained foreign bodies in patients with a history of trauma. Depending on the individual clinical scenario, surgical interventions may be necessary to mitigate potential risks.
AUTHORS’ CONTRIBUTION
X.L.: Data collection; F.J.: Analysis and interpretation of results; W.S. and T.H.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| FB | = Foreign Body |
| BCVA | = Best Corrected Visual Acuity |
| MRI | = Magnetic Resonance Imaging |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study received ethical approval from the Medical Ethics Committee of Tianjin Medical University General Hospital, China (Reference Number: IRB2025-YX-075-01).
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article will be available from the corresponding author [T.H.] upon reasonable request.
ACKNOWLEDGEMENTS
The authors would like to thank the patient for the invaluable support and coordination.


