All published articles of this journal are available on ScienceDirect.
Reversal of Cupping in a Patient with Juvenile Open-angle Glaucoma who Underwent Deep Sclerectomy: A Case Report
Abstract
Background
Reversal of cupping refers to a reduction in optic disc cup size. It is a rare phenomenon primarily observed after antiglaucoma surgeries, particularly in patients with juvenile glaucoma.
Case Presentation
We report a case of reversal of cupping in an adult male patient who underwent deep sclerectomy. He had no history of eye surgery, trauma, or use of medications, such as steroids, nor any family history of glaucoma. He presented with uncontrolled intraocular pressure despite medical treatment and selective laser trabeculoplasty.
Conclusion
Following the reversal of cupping, deep sclerectomy with mitomycin C proved to be a safe and effective method to lower intraocular pressure. Additionally, no significant complications were observed. Further research is required to elucidate the mechanism of cupping and evaluate its relationship with the development of juvenile glaucoma.
1. INTRODUCTION
Reversal of cupping is a term used to describe the reduction in optic disc cup size that occurs when the intraocular pressure (IOP) reduces by ≥ 25% [1]. This condition is most typically observed after glaucoma surgeries, particularly in patients with juvenile and primary congenital glaucoma and less commonly in adult patients [2]. The causes of true reversal of cupping include a decrease in the diameter of the scleral canal, which is elastic in nature at a younger age, and the forward movement of the lamina cribrosa. Consequently, reversal of cupping can become challenging if elasticity declines with age, which causes stiffening of the mechanical support of the head of the optic nerve [3]. In patients with congenital glaucoma, the cupping rates can be reversed by 40%–70% with good IOP management after surgical therapy [4]. Herein, we report a case of reversal of cupping in a patient with juvenile open-angle glaucoma who successfully underwent deep sclerectomy (DST).
2. CASE REPORT
2.1. Patient Details
This case report describes the reversal of glaucomatous cupping of the optic nerve in an 18-year-old male patient with a history of juvenile open-angle glaucoma (JOAG). The patient was from Najran, which is a province located in the south of Saudi Arabia. He presented to a glaucoma clinic at King Khaled Eye Specialist Hospital in Riyadh, Saudi Arabia. He was first diagnosed with JOAG at the age of 16 years.
The patient first exhibited blurring of vision and intermittent pain in the left eye (LE). Based on the assessment using the Goldmann applanation tonometry, the IOPs of the right eye (RE) and LE were 19 and 16 mmHg, respectively. The patient was then diagnosed with JOAG with uncontrolled IOP. However, he did not present with a previous history of eye surgery or trauma, the use of medications, such as steroids, or any family history of glaucoma. Routine ophthalmic examination revealed that the patient’s visual acuities were 20/40 in the RE and 20/25 in the LE, respectively.
The biomicroscopic slit lamp examination provided normal results for both eyes, and the fundus examination showed an unremarkable fundus with a flat retina without evidence of retinal tears or breaks. The patient received brimonidine tartrate/timolol maleate ophthalmic solution (Combigan®) and latanoprost (Xalatan®) for the medical treatment of both eyes. A gonioscopy examination revealed evidence of an open and normal angle without pigmentation. Meanwhile, fundoscopy showed concentric optical disc cupping with C/D ratios of 0.8 and 0.6, respectively (Fig. 1A and B). Moreover, the central corneal thickness values were 581 and 593 mm for RE and LE, respectively. The Humphrey visual field test revealed a superior arcus with nasal step in both eyes (Fig. 2). Moreover, generalized thinning was observed in both eyes on optical coherence tomography.
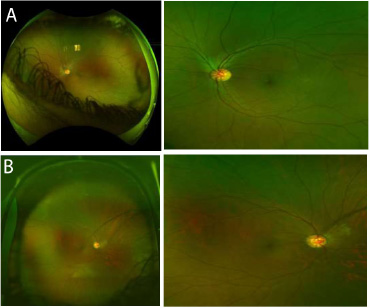
Fundus images of both eyes showing significant optic disc cupping preoperatively.
After 1 year, the IOP of the RE remained uncontrolled, exceeding the target level of 20 mmHg. Brinzolamide (AZOPT eye drops) was administered two times daily. After 3 years, the subsequent assessment revealed that the patient presented with persistent uncontrolled IOP in the RE, which reached 24 mmHg. He was not feeling well. Thus, we placed him on full medication. The patient received a minimal number of brinzolamide/brimonidine drops (Simbrinza) two times daily, and bimatoprost/timolol (Ganfort) was taken once daily. Subsequently, selective laser trabeculoplasty was performed to control the IOP in the RE, which remained high. Meanwhile, DST with mitomycin C (MMC) for the RE was planned.
2.2. Surgical Technique
The patient was prepared and draped using the usual aseptic procedures for ophthalmic intervention. A wire speculum was applied to open the lids. A clear traction 7-0 Vicryl suture was placed from the 11 to 1 o’clock position, and the eye was rotated inferiorly. A fornix-based conjunctival flap was made between the 10 and 2 o’clock position. Hemostasis was achieved with light cautery. A trapezoidal marker for the partial-thickness superficial scleral flap was used (5 mm (anterior border) × 5 mm (long) × 4 mm (posterior border)) and was dissected with the Mani blade. Filter papers soaked in 0.002% MMC solution for 2 min were applied under the far posterior part of the conjunctiva (Kwan technique) and the scleral flap. Thereafter, the filter papers were removed, and the field was irrigated with 100 mL of balanced salt solution.
A trapezoidal marker for the second scleral flap was also used (4 mm (anterior border) × 4 mm (long) × 3 mm (posterior border)). Next, it was dissected with the Mani blade to almost full thickness under the first flap and into the clear cornea, thereby making a wide trabeculo-Descemet window. Paracentesis was performed, and the eye was cautiously decompressed. Then, Miocol was injected intraocularly. The remnant scleral tissue from the second flap was excised using special DST scissors. The inner wall of the Schlemm’s canal was scraped and peeled.
Next, the Sclemm’s ostium was checked with the Mermoud spatula. After assessing for adequate filtration, right outflow, and anterior chamber stability, the first scleral flap was closed loosely with a 10/0 nylon suture. The conjunctiva was closed using the 9-0 Vicryl suture. Cefazolin at a dose of 50 mg and dexamethasone at a dose of 2 mg were administered subconjunctivally. The lid speculum and traction suture were removed. Then, Maxitrol ointment and Pilocarpine 2% drops were applied, followed by a patch and shield.
On postoperative day 1, significant improvements were observed. The best-corrected visions were 20/40 for the RE and 20/25 for the LE, respectively. Further, the IOP was significantly reduced, with the RE and LE having an IOP of 5 and 17 mmHg, respectively. The antiglaucoma medications for RE were discontinued, and the IOP in the RE was controlled within the next 3–6 months after surgery. A slit lamp examination of the RE revealed a clear cornea without signs of leakage. In addition, there was evidence of a conjunctival diffuse elevated bleb (+2). The anterior chamber was deep and quiet, indicating the patient to have a stable postoperative condition.
After 3 months, follow-up examinations revealed that the patient’s condition significantly improved. The IOP in the RE remained stable at 5 mmHg. Meanwhile, the IOP in the LE was 20 mmHg. Further, an optic disc examination indicated significant improvements, with a reduction in cupping by 0.7 mm in the RE (Fig. 1B). In addition, the visual field was stable. Due to the positive outcome, the antiglaucoma medication for the RE was discontinued. However, at 6 months post-surgery, the patient expressed discomfort with the continued use of the medications for the LE. Therefore, to prevent the need for ongoing medication management, the patient was scheduled for DST with MMC specifically for the LE.
On postoperative day 1, encouraging outcomes were observed. The IOP in the LE was 5 mmHg. Upon examination, the conjunctiva exhibited a diffuse bleb that was rated as elevated +3. This finding indicated a successful surgical intervention with the development of a well-formed bleb, thereby contributing to the stability of the postoperative condition. Subsequently, at 4 months post-surgery, the antiglaucoma medication for the LE was discontinued. This reflected the positive response to the surgical intervention and the sustained management of IOP within an acceptable range.
During the last visit, the optic disc cupping significantly improved. In particular, based on the measurements, it returned to the normal level (0.5 for the RE and 0.3 for the LE) (Fig. 2A and B). This positive change indicated a favorable response to the surgical procedure, with the optic nerve showing signs of restoration to a healthier state. In addition, the visual field was stable, further confirming the efficacy of the interventions. These promising outcomes suggested DST to be effective in addressing the underlying pathology and optimizing the visual function of the patient.
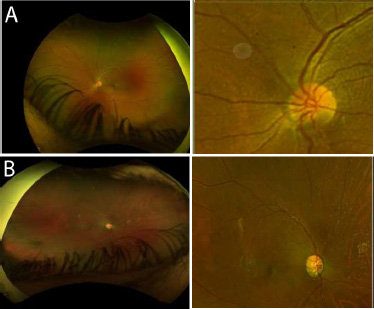
Fundus image of both eyes showing a significant reversal in optic disc cupping at 8 months postoperatively.
3. DISCUSSION
Several studies have documented the reversal of optic disc cupping after antiglaucomatous surgeries. Reversal of optic disc cupping has been reported to be associated with a decrease in IOP progression, but without subsequent improvement in visual function [5]. Cup reversal is associated with glaucoma progression (odds ratio = 0.226, 95% confidence interval: 0.055–0.99) and is considered an independent protective factor [6]. In the study performed by Kotecha et al. [7], a reduction in the IOP was observed in 70 patients who exhibited reversal of disc cupping at 2 years after trabeculectomy and a significant increase in rim volume. Meanwhile, in another report, 3 of 67 patients did not exhibit improvement in their visual acuity. However, they presented with a reduction in IOP at 3–6 months after trabeculectomy [8]. The growth of the astroglial tissue filling the cup, the restoration of intra- and extracellular fluid in the optic disc, and the narrowing of the scleral canal due to scleral elasticity are some theories that can explain the occurrence of optic disc cupping. This theory explains why children have a higher prevalence of restricted scleral canals because a rigid scleral canal structure prevents scleral canal size from changing immediately in adult individuals [5]. In the current case, there was no previous history of eye surgery or trauma, the use of medications, such as steroids, or any family history of glaucoma. Silva et al. [9] reported a case of juvenile glaucoma that presented with a reversal of disc cupping in a patient without a previous history of eye surgery or trauma. After 1 year of treatment with prostaglandin analog, the patient presented with a reduction in IOP and a decrease in optic disc cupping. In our case, after 2 years of using combined topical beta blockers, alpha agonists, and prostaglandin, the target level of IOP management [optical disc cupping (C/D ratio) of 0.8 and 0.6 on the RE and LE, respectively] was not achieved. Selective laser trabeculectomy based on level I evidence was first performed. Therefore, it can be a primary management for POAG, and it has long-term effects and few complications [10]. However, the patient’s IOP did not significantly improve even though it decreased after DST with MMC. In a previous study, the success rate was 85.7% in 98 eyes, which was defined as a 30% postoperative reduction of IOP after trabeculectomy combined with DST with MMC. However, there was no significant correlation between postoperative IOP control and the best corrected visual acuity [11]. Other studies have reported a 30% postoperative reduction in the IOP (complete success A1) within 2 years in patients who have not received medications after sutureless DST [12]. A retrospective case series assessed 26 eyes with glaucoma in patients who underwent DST with 0.2–0.4 mg/mL MMC, which appeared to be safe with a low rate of complications and an effective procedure for lowering IOP [13]. This was confirmed by other studies as DST with MMC provided effective results with fewer complications compared to trabeculectomy [14, 15]. In the current case, after DST with MMC, the cup-to-disc ratio reversed from 0.8 and 0.6 to 0.5 and 0.3 in the RE and LE, respectively. Concomitantly, an improvement in the visual field was detected. However, three adult patients with reversal of glaucomatous cupping showed improvement in the visual field after a 79.1% reduction in IOP. Therefore, reversal of cupping may occur even in adults and children with advanced conditions [16]. Meirelles et al. [17] analyzed the variables associated with the reduction in the C/D ratio. Results showed younger age at the time of surgery to be associated with a high reversal cupping rate. Other reports have revealed a significant reduction in the C/D ratio in patients with a 36% reduction in IOP after medical management with topical prostaglandin [18]. Lesk et al. [19] reported a reduction in cup volume and area in patients with a decreased IOP. Meanwhile, Nicolela et al. [20] and Felembam et al. [21] did not identify optic disc changes as the change in IOP was modest (Figs. 3 and 4).
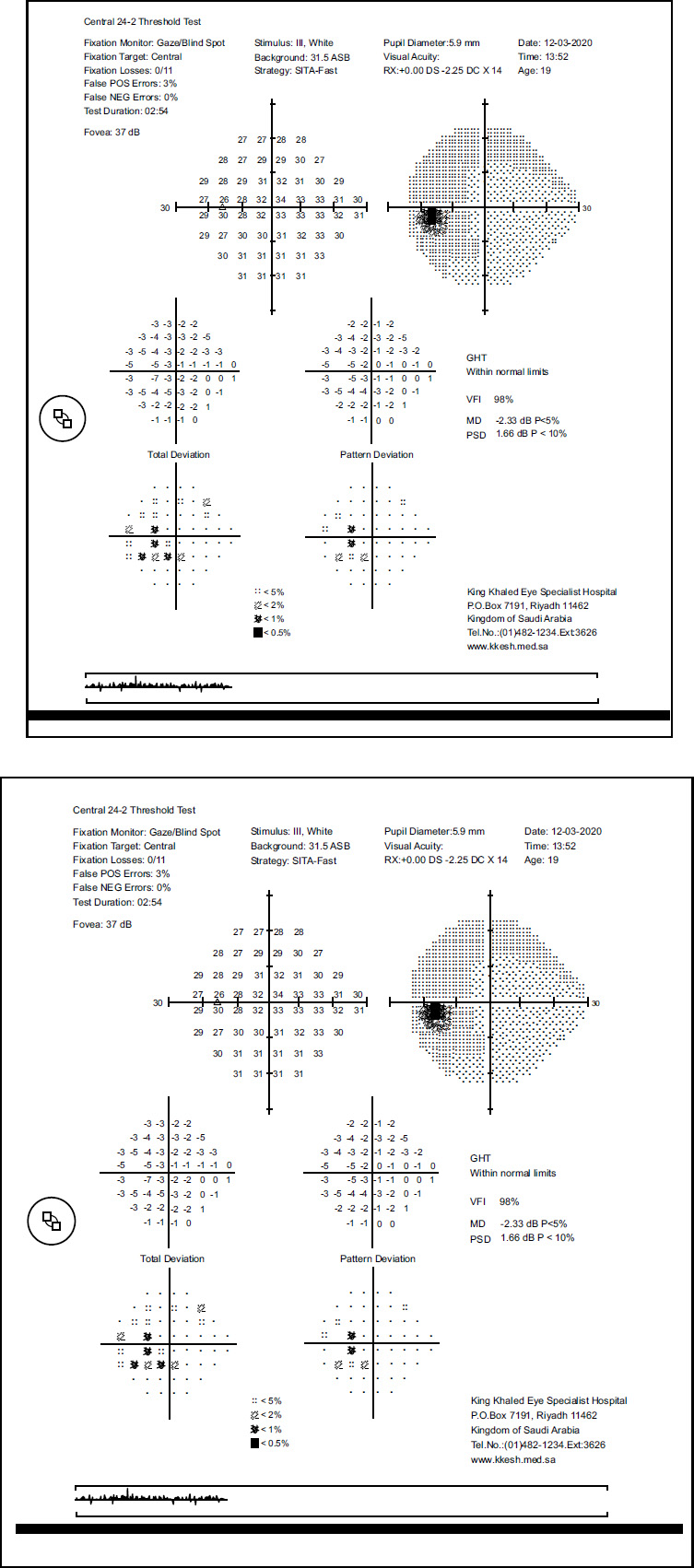
Humphry 30-2 visual field of both eyes showing the patient’s visual field to be stable postoperatively.
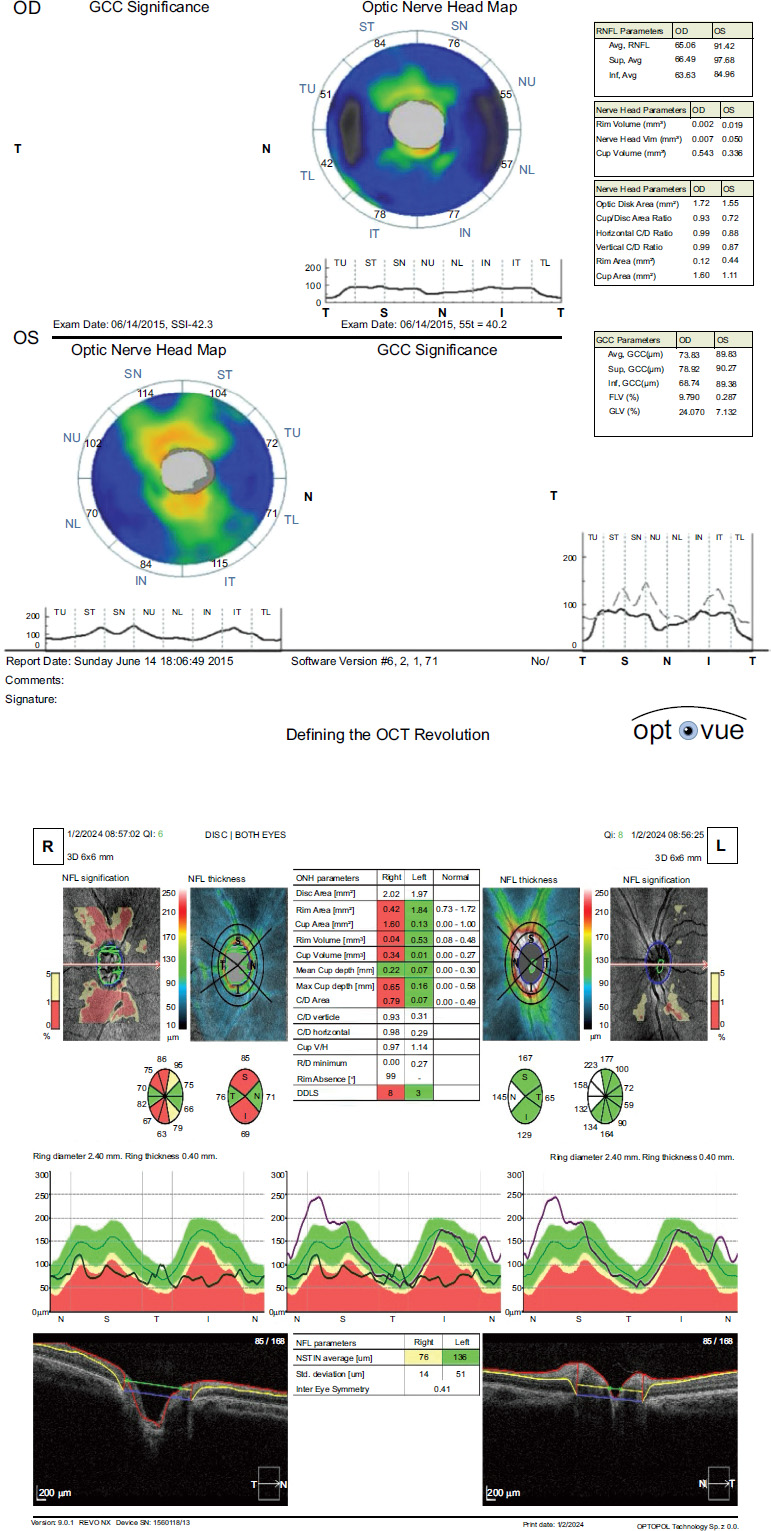
Optical coherence tomography of the optic disc showing a significant postoperative improvement in retinal nerve fiber thickness compared to the preoperative measurement.
CONCLUSION
In this case, DST with MMC was effective and safe for reducing IOP after the reversal of cupping. Moreover, it was not associated with major complications. Nevertheless, more studies should be conducted to validate the pathophysiology of the reversal of cupping and assess its relation to juvenile glaucoma progression.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| IOP | = Intraocular pressure |
| DST | = Deep sclerectomy |
| JOAG | = Juvenile open-angle glaucoma |
| LE | = Left eye |
| RE | = Right eye |
| MMC | = Mitomycin C |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was obtained from the research ethics committee at King Khalid Eye Specialist Hospital, Riyadh, Saudi Arabia with approval number RD/26001/IRB/0583-23.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
The authors thank the patient for graciously consenting to participate in this research study.


