All published articles of this journal are available on ScienceDirect.
Efficacy of Anterior Chamber Air Injection with Scleral Tunnel Peripheral Iridectomy for Descemet’s Membrane Detachment
Abstract
Aims and Objectives
This study aims to explore the effectiveness of iridotomy combined with anterior chamber insufflation for the treatment of Descemet's membrane detachment (DMD) through a scleral tunnel incision.
Methods
This is a retrospective study, analyzing 48 DMD patients treated at Hainan Eye Hospital, Zhongshan Ophthalmic Center, Sun Yat-sen University, from December 2012 to October 2024. Patients were divided into a conservative treatment group, a simple anterior chamber air injection group, and an anterior chamber air injection combined with peripheral iridectomy group through through scleral tunnel incision according to different treatment methods. Herein, the patient's preoperative visual acuity, corneal edema, and DMD recovery were observed and recorded on postoperative day 1, 7, and 1 month. Literature was retrieved related to DMD for the past 10 years, which was compared and analyzed for risk factors, treatment methods, and treatment outcomes.
Results
The conservative treatment group consisted of 12 cases, with an average age of 73.0±10.7 (SD) years and an average recovery time of 13.7 days. There were 6 cases in the simple anterior chamber air injection group, with an average age of 68.6±8.5 (SD) years. On the first day after surgery, all cases of DMD had complete recovery. Among them, 3 cases had elevated intraocular pressure on the first day after surgery, and were treated with anterior chamber deflation and medication to reduce intraocular pressure. Two cases recovered to normal intraocular pressure 3 days after surgery, and 1 case developed ciliary ring block glaucoma. Posterior vitrectomy combined with peripheral iridectomy was performed to control intraocular pressure. Thirty cases of iris peripheral surgery combined with anterior chamber air injection group were considered, with an average age of 70.6±7.4(SD) years. On the first day after surgery, 2 cases had elevated intraocular pressure, which was restored through drug treatment. One week after surgery, one case of DMD did not recover, but was restored through corneal suturing and anterior chamber insufflation. The remaining 27 patients had normal intraocular pressure, DMD recovery, and resolution of corneal edema on the first day after surgery. In both the simple anterior chamber air injection group and the combination therapy group, there was one case of slight anterior chamber bleeding on the first day after surgery. Postoperative complication rates were significantly lower in the combined group (13.33%) compared to the simple injection group (83.33%, p=0.003).
Discussion
Anterior chamber air injection effectively reattaches DMD, while adjunctive scleral tunnel iridectomy reduces the risks of postoperative angle closure and IOP elevation. The surgical approach avoids re-injury of DMD and minimizes complications.
Conclusion
Combined anterior chamber air injection and scleral tunnel peripheral iridectomy is a safe and effective treatment for DMD, with a low incidence of postoperative complications.
1. INTRODUCTION
Descemet's membrane is the basement membrane of corneal endothelial cells. Descemet's membrane detachment (DMD) is one of the common complications after cataract surgery. In 1928, Samuels [1] first reported DMD after anti-glaucoma surgery. The occurrence of DMD can cause serious visual impairment, and if not handled properly, it can lead to corneal decompensation. Timely reposition of the Descemet membrane can immediately restore corneal clarity and prevent further corneal complications [2].
Multiple authors have classified DMD into various categories. In one of the studies, Kumar et al. [14] proposed an HELP algorithm based on AS OCT (representing height (measured by distance between detached Descemet's membrane (DM) and corneal stroma), degree of DM in the cornea (central, sub central, and peripheral cornea), length of detachment, and pupil (DMD to pupil position)) to help manage different types of DMD, and proposed different conservative or surgical treatment measures based on the height and range of DMD detachment. Jain et al., classified DMD based on the location and extent of detachment using anterior segment optical coherence tomography (AS-OCT) [3]. They defined DMD as involving more than half of the cornea, and severe DMD as extending to the central cornea. Early surgical treatment is advocated for severe DMD, with the expectation of achieving good visual outcomes [4-6]. However, in clinical practice, it is challenging to establish a clear boundary, which can lead to confusion in selecting specific clinical treatment methods.
We selected different treatment measures based on the duration of DMD. AS-OCT examination was performed on cases with corneal edema that did not subside one week after cataract surgery. Patients diagnosed with DMD were treated conservatively for 3 weeks, and those who did not recover were treated with anterior chamber air injection. For cases where there is no recovery through anterior chamber gas injection, corneal suturing is used to reposition DMD. Our use of a scleral tunnel incision combined with peripheral iridectomy can reduce the risk of DMD recurrence, postoperative high intraocular pressure, and angle closure glaucoma compared to simple anterior chamber insufflation. The following report is presented.
2. METHODS
This retrospective study was approved by the ethics committee of Hainan Eye Hospital, with informed consent waived, and was conducted in accordance with the tenets of the Declaration of Helsinki. The approval number of the Ethics Committee is: 2024-028-01. Patients with DMD after cataract surgery from Nov 01, 2012, to Aug 30, 2024, at Hainan Eye Hospital, Zhongshan Ophthalmic Center, Sun Yat-sen University, Hainan, China, were reviewed.
2.1. Inclusion Criteria
The inclusion criteria were as follows:
(1) Patients aged ≥18 years diagnosed with DMD following cataract surgery;
(2) DMD confirmed by AS-OCT, with corneal edema persisting for more than 1 week;
(3) Complete clinical records, including preoperative and postoperative follow-up data (visual acuity, intraocular pressure, corneal edema status, and AS-OCT results at 1 day, 7 days, and 1 month postoperatively).
2.2. Exclusion Criteria
The exclusion criteria were as follows:
(1) Non-surgical DMD (e.g., caused by trauma, corneal transplantation, glaucoma surgery, or other non-cataract procedures);
(2) Concurrent severe ocular diseases (e.g., active ocular infection, corneal endothelial decompensation, advanced glaucoma, or retinal pathologies that may interfere with treatment evaluation);
(3) Incomplete data or loss to follow-up (patients with missing postoperative records or failure to complete the 1-month follow-up).
For cases where corneal edema does not subside one week after surgery, routine AS-OCT examination is performed. For patients diagnosed with DMD, a conservative treatment regimen of three weeks is recommended. If there is still no recovery, simple anterior chamber air injection or combined scleral tunnel incision iridectomy and anterior chamber air injection surgery should be performed. Follow-up should be conducted on the first and the, seventh day, and one month after surgery. If the DMD does not recover from anterior chamber insufflation, the DMD and corneal suture should be combined, and the anterior chamber should be insufflated again. Patients were divided into a conservative treatment group, a simple anterior chamber gas injection group, an anterior chamber air injection group with iridectomy group through a ciliary tunnel incision.
2.3. Simple Anterior Chamber Air Injection
Under routine corneal surface anesthesia, anterior chamber puncture was performed on the limbus in areas without DMD based on the preoperative AS-OCT examination. Air bubbles were injected into the anterior chamber to increase intraocular pressure to TN+3. After 5 minutes, some air was released to reduce intraocular pressure to TN+1. After returning to the ward, a supine position was maintained for 2 hours.
2.4. Peripheral Iridectomy with Scleral Tunnel Incision Combined with Anterior Chamber Air Injection
At approximately 11 O’clock, subconjunctival local infiltration anesthesia with 2% lidocaine was given to the patient. The conjunctiva was cut to open along the limbus to perform cauterization to stop bleeding. A scleral tunnel incision with a width of approximately 1mm and a length of approximately 2mm was made 1mm behind the edge of the cornea. The peripheral iris was pulled out along the tunnel to perform partial excision, and then retracted into the anterior chamber. The filtered air was then injected into the anterior chamber through a scleral tunnel incision to achieve TN+3 intraocular pressure, which was maintained for 5 minutes, and then some air was released to bring the intraocular pressure back to TN+1. The conjunctiva was burned and aligned, with 0.3% Tobramycin and dexamethasone eye ointment (Alcon, USA) applied to the conjunctival sac. The patient was advised to maintain a supine position for 2 hours after returning to the ward (Fig. 1).
2.5. DMD Corneal Suturing Surgery
Under corneal surface anesthesia, a 2.4mm transparent limbus incision was made far away from DMD. The viscoelastic agent was injected into the anterior chamber to reattach the detached DM to the cornea. A 10/0 nylon suture was used to insert the needle from the corneal surface, pass through the cornea, cross over the DM, and exit the cornea for knotting. The viscoelastic agent was aspirated from the anterior chamber, and filtered air was injected to restore DMD. Corneal bandage contact lenses were used to reduce postoperative stimulation. One week after surgery, the corneal sutures were carefully removed, followed by the removal of bandage lenses.
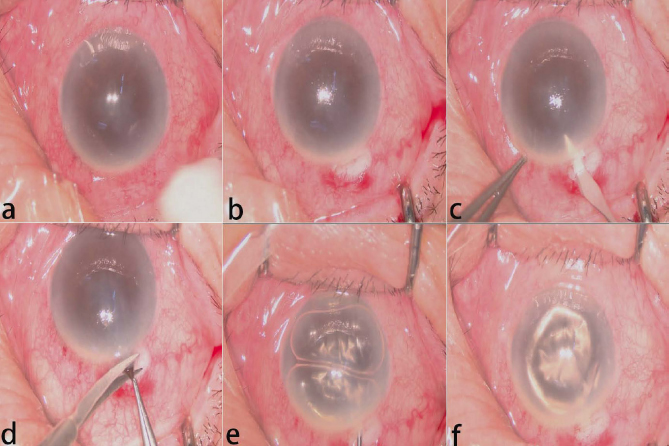
Surgical procedure of scleral tunnel peripheral iridectomy combined with anterior chamber air injection. (a) Perform subconjunctival local infiltration anesthesia (b) Conjunctival incision at the limbus; (c) Creation of a 1-mm scleral tunnel 1 mm behind the limbus; (d) Peripheral iridectomy performed through the tunnel; (e) Air injection to achieve intraocular pressure of TN+3; (f) Release some air to bring the intraocular pressure back to TN+1
| Demographics | CT Group | SI Group | PIACI Group |
|---|---|---|---|
| Cases | 12 | 6 | 30 |
| Patients/Eyes (n) | 12/12 | 6/6 | 30/30 |
| Age (y, Mean ± SD) | 73.0±10.7 | 68.6±8.5 | 70.6±7.4 |
| Males/Females (n) | 7/5 | 2/4 | 13/17 |
| Right/Left eye (n) | 4/8 | 3/3 | 19/11 |
2.6. Clinical Data Collection and Follow-up
For the conservative treatment group, the following data was collected: the anterior segment examination results, visual acuity, average recovery time, and AS-OCT recovery status of patients before and after treatment.
For the group receiving simple anterior chamber air injection and the group receiving peripheral iridectomy combined with anterior chamber air injection, the following data were collected: the preoperative and postoperative anterior segment examination results, preoperative and postoperative visual acuity, recovery time, and AS-OCT status of the patients.
2.7. Statistical Analysis
Data were analyzed using SPSS software (version 26.0, IBM, USA). Continuous variables were presented as mean ± standard deviation (SD) based on normality tested by the Shapiro-Wilk test. Categorical variables were compared using the Chi-square test or Fisher’s exact test.
2.8. Retrieve Literature
A systematic literature search of articles published from January 1, 2014, to September 1, 2024, was performed on September 2, 2024, in two electronic databases: MEDLINE (PubMed) and Scopus. Eligibility criteria included the adult population with DMD related to cataract surgery. Exclusion criteria included reviews, studies with no full-text availability, articles not conducted on humans, videos, and comments.
3. RESULTS
All patients in the three groups were successfully followed up for 1 day, 7 days, and 1 month after surgery. The conservative treatment group consisted of 12 cases, with an average age of 73.0±10.7 (SD) years. The male-to-female ratio was 7:5, and the ratio of right to left eye involvement was 4:8. The average recovery time was 13.7 days. There were 6 cases in the simple anterior chamber gas injection group, with an average age of 68.6±8.5(SD) years. The male to female ratio was 2: 4 and the ratio of the right to left eye involvement was 3:3. There were 30 cases of iris peripheral surgery combined with anterior chamber air injection group, with an average age of 70.6±7.4(SD) years. The male-to-female ratio was 13:17, and the ratio of right-to-left eye involvement was 19:11. Only one patient, a 75-year-old man with right eye involvement, underwent a corneal suture (Table 1).
3.1. Comparison of Preoperative and Postoperative Visual Acuity and AS-OCT
The preoperative visual acuity in the conservative treatment group ranged from 20/200 to 20/50 (n=12), and the visual acuity on postoperative day 1, postoperative day 7, and postoperative month 1 ranged from 20/200 to 20/40, 20/50 to 20/20, 20/50 to 20/20 (n=12). In the simple injection group, the peripheral iridectomy was combined with anterior chamber gas injection group, and the preoperative visual acuity ranged from count fingers (CF) 1 foot to 20/100 (n=6) and hand movements (HM) 6 feet to 20/100 (n=30). The visual acuity on the 1 day, 7 days, and 1 month after surgery ranged from: CF 6 feet to 20/100 (n=6), CF 4 feet to 20/40 (n=30); HM 6 feet to 20/70 (n=6), 20/70 to 20/20 (n=30); 20/70 to 20/20 (n=6), 20/50 to 20/20 (n=30).
Most of the Descemet's membrane recovered after surgery. Fig. (2) shows anterior segment photographs and anterior segment OCT images before DMD and after peripheral iridectomy combined with anterior chamber gas injection.
3.2. Comparison of Intraoperative and Postoperative Complications
In the single injection group, on the first day after surgery, all cases of DMD were able to recover. Among them, 3 cases had elevated intraocular pressure on the first day after surgery, and were treated with anterior chamber deflation and medication to reduce intraocular pressure. Two cases recovered to normal intraocular pressure 3 days after surgery, and 1 case developed ciliary ring block glaucoma. Posterior vitrectomy combined with peripheral iridectomy was performed to control intraocular pressure. In the peripheral iridectomy combined with anterior chamber air injection group, on the first day after surgery, two cases had elevated intraocular pressure, which was restored through drug treatment. One week after surgery, one case of DMD did not recover, but was restored through corneal suturing and anterior chamber air injection. The remaining 27 patients had normal intraocular pressure, DMD recovery, and resolution of corneal edema on the first day after surgery. In both the simple anterior chamber air injection group and the combination therapy group, there was one case of slight anterior chamber bleeding on the first day after surgery, which was completely absorbed on the third day after surgery. The postoperative complication rates in the simple air injection group and the combined iridectomy group were 83.33% and 13.33%, respectively, with a statistically significant difference between the two groups (p=0.003) (Table 2).
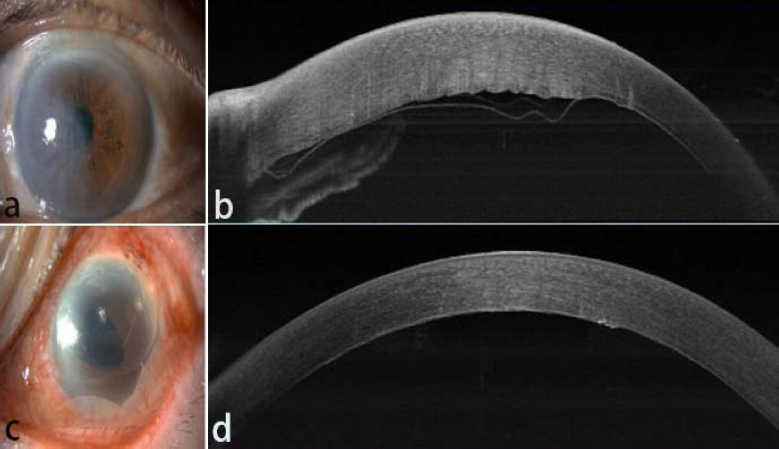
Preoperative and postoperative anterior segment photographs and AS-OCT images. (a) Anterior segment photograph: preoperative corneal edema with DMD.(b) AS-OCT: preoperative DMD. (c) Anterior segment photograph: postoperative day 1 showing resolved edema. (d) AS-OCT: postoperative day 1 demonstrating DMD.
| Groups | ACH | PHIP | DMD RF | Other | Incidence of Complication | p |
|---|---|---|---|---|---|---|
| CT Group | 0/12 | 0/12 | 0/12 | 0/12 | 0 | 0.003 |
| SI group | 1/6 | 3/6 | 0/6 | 1/6 | 83.33% | |
| PIACI group | 1/30 | 2/30 | 1/30 | 1/30 | 13.33% |
3.3. Comprehensive Literature Analysis of Risk Factors, Treatment Methods, and Treatment Outcomes
According to the cases we collected, the related factors of DMD are as follows: age over 65 years, cataract surgery, especially transparent small incision. The primary treatment methods are conservative treatment, simple anterior chamber air injection treatment, and more advanced anterior chamber air injection combined with iridectomy, with a lesser proportion of the use of the corneal suture method. The main complications were increased intraocular pressure, hyphema and detachment without reduction after operation.
Literature review [3, 7-17] has revealed that the risk factors include advanced age, previous chemical injury, dense cataract, clear corneal small incision surgery, and corneal congenital dystrophy. The treatment method is not uniform. The main treatment is anterior chamber gas injection, including sterile gas or SF6, etc. The main postoperative complications were increased intraocular pressure, and in more severe cases, poor Descemet's membrane attachment. Table 3 shows DMD and its risk factors, treatment modalities, and complications found in the literature.
| Study | Date | Surgery Performed | Associated Risk Factor(n) | Management(n) | Position of Incision | Outcome (n) | Comlication |
|---|---|---|---|---|---|---|---|
| Doi et al. [10] | 2021 | Cataract surgery | Over 65 years old, | SF6 injection | NA | DMD reattached | NA |
| Li et al. [7] | 2023 | NA | Trauma,congenital glaucoma | C3F8 injection | Scleral limbus | DMD reattached | High IOP |
| Jain et al. [3] | 2013 | Cataract surgery | Small-incision | Air or mixture of 14% C3F8 injetion | Corneal | 57 patients (95%) had a successful reattachment, 3 patients (5%) with persistent DMD |
Pupillary block was seen in 7 cases (11.66%) in which C3F8 |
| Trindade et al. [8] |
2023 | Cataract surgery | FECD | Air or 18% diluted SF6 gas injection | Corneal | 4 patients had a successful reattachment, 1patien with persistent DMD | NA |
| Marcon et al. [9] |
2002 | Cataract surgery | Over 65 years old, cataract surgery | Medical treatment alone or SF6 injection | Corneal | 13 eyes had a successful reattachment,2 eyes required a penetrating keratoplasty. | NA |
| Sunita Chaurasia et al. [11] | 2012 | Cataract surgery | Small-incision,cataract surgery | Air (100%) injection | Limbal site | 13 patients had a successful reattachment,1patien withpersistent DMD | Raised IOP in 14.3% of cases |
| Berger et al. [12] | 2023 | PKP,cataract surgery | PKP,pellucid marginaldegeneration, FECD, herpetic keratitis | Air/Gas-Descemetopexy | Corneal | The postoperative course was uneventful in 16 of 18 eyes. | NA |
| Odayappan et al. [13] | 2017 | Cataract surgery | NA | Air (100%) injection | Corneal paracentesis | Successful reattachment after primary descemetopexy 71%. 15 patients underwent repeat descemetopexy with 60% success rate | Persistent DMD (21.8%), corneal decompensation (7.3%), appositional angle closure (18%), pupillary block with air (2.7%) and uveitis (2.7%). |
| Kumar et al. [14] | 2015 | Post-phacoemulsification | Fuchs dystrophy | Surgical intervention:14% C3F8 or 20% SF6 or sterile air injection. Medical management included a topical hyperosmotic agent, prednisolone acetate 1.0%, and ofloxacin 0.3% | NA | Successful outcome in 95.8% cases of surgical therapy and 96.9% cases of medical therapy. No difference in CDVA |
Pupillary block glaucoma (7.7%) |
| Sharma et al. [15] |
2015 | Post-intraocular surgery | Small-incision | Intracameral air or14% C3F8 | Corneal | Success rate was 100%. |
Two cases in the C3F8 group had raised IOP. One case required repeat injection |
| Jain R and Mohan N [16] | 2014 | Cataract surgery | Small-incision | 100% air or isoexpansile mixture of 14% C3F8 | Corneal | Successful outcome in 92.3% cases No difference in reattachment rate between air and C3F8. |
Pupillary block glaucoma in one case of C3F8 |
| Jyoti Garg et al. [17] | 2016 | Cataract surgery | NA | Intracameral C3F8 | Corneal | EK required in 1 case Complete reattachment in 72% cases, Partial reattachment in 18% 100% success rate in planar type while 54% for nonplanar type. |
Pupillary block and raised IOP in 13.4% cases |
4. DISCUSSION
DMD normally occurs as aqueous humor enters the pre-descemetic space along a tear in Descemet’s membrane (DM). DMD can also be caused by preoperative corneal endothelial lesions, corneal stromal diseases, corneal contusions or neovascularization, but the main reason is still iatrogenic intraocular surgery [18]. Inocular surgeries such as corneal transplantation, glaucoma surgery, or vitreoretinal surgery, but more importantly, cataract surgery such as extracapsular cataract extraction and phacoemulsification are the main cause of DMD, with the incidence rates of 2.5% and 0.5%, respectively [19].
Surgical intervention, such as Descemetopexy, mechanical tamponade, or suture fixation, is considered the primary treatment option for postoperative patients who cannot be treated conservatively or with medication. Descemetopexy is the surgical reattachment of the detached DM with an injection of air and/or isoexpansile gases like perfluoropropane (C3F8, 12 -14%) and sulfur hexafluoride (SF6, 15-20%), which is widely recognized as the most effective treatment for DMD [9]. Ti et al. [18] used sterilized air packing in the anterior chamber to restore corneal clarity in 87.5% of DMD patients after phacoemulsification. However, there is currently no unified consensus on the timing of surgery, the selection of surgical incision location, the injection of air or isoexpansile gases into the anterior chamber, and combination of peripheral iridectomy.
The widely recognized treatment for DMD reduction involves early detection and treatment to reduce permanent damage to the cornea [15]. Some people also believe that different treatment timing and methods should be chosen based on the scope of departure, but there are significant individual differences among patients, making it difficult for a single patient to make a specific choice [10]. In our treatment options, for cases where corneal edema does not subside one week after cataract surgery, AS-OCT examination is routinely performed to determine the presence of DMD. One month after cataract surgery, if conservative treatment has not resolved surgical intervention measures should be taken. For the patients we treated, the longest treatment time was 6 months after surgery, and all patients achieved complete recovery. So there is no need to advance the surgical treatment time too much, as some patients may have the possibility of self-healing. For cases where DMD has not recovered, one month after cataract surgery is an ideal time for surgical intervention.
Injecting filtered air or isoexpandable gases into the anterior chamber is the main method for DMD reduction [11]. Isoexpandable gases can theoretically increase the probability of successful reduction due to their long residence time in the anterior chamber. During surgery, it is also recommended to fill the anterior chamber with gas for 10-15 minutes, which will inevitably increase the surgical time [13]. The long-term absorption of isoexpandable gases in the anterior chamber prolongs the postoperative visual recovery time for patients. All of our cases involved injecting air into the anterior chamber, with a success rate of 96.7% (29/30), except for one case that underwent surgical suturing. At the same time, the anterior chamber is filled with air during surgery to achieve an intraocular pressure of TN+3. This is maintained for 5 minutes, and approximately one-third of the air is released before the end of the surgery to reduce the intraocular pressure to TN+1. After the surgery, a supine position is maintained for 2 hours. Almost all cases had corneal edema subside on the first day after surgery, and air was absorbed in two days, resulting in complete recovery of the patient.
It is recommended to make an incision in the area without DM detachment based on the preoperative AS-OCT examination results for anterior chamber injection, which can avoid causing DMD to enlarge again. At the same time, it is common to choose a transparent corneal incision or a corneal limbal incision, which can reduce the surgical time. However, for DMD patients with severe preoperative corneal edema and a large area, it is sometimes difficult to find an incision on the cornea that can avoid DMD. We, therefore, selected a scleral tunnel incision with a distance of 1mm behind the limbus, a width of 1mm, and a length of 1.5mm, which basically completely avoids the position of DMD and does not increase the possibility of DMD being damaged again. At the same time, using this incision, peripheral iridectomy can be performed, reducing the risk of multiple incision injuries for patients.
Many scholars have different opinions on whether injecting gas into the anterior chamber of DMD should be combined with peripheral iridectomy. Scholars who advocate against the need for peripheral iridectomy, especially in patients with air injection into the anterior chamber, believe that air remains in the anterior chamber for a short period of time and can be quickly absorbed, thus avoiding the need for peripheral iridectomy and reducing surgical trauma for patients. Scholars who advocate for the need for peripheral iridectomy, especially those who believe in injecting isoexpandable gases into the anterior chamber, believe that prolonged presence in the anterior chamber can prevent postoperative intraocular pressure increase or gas from entering the posterior chamber, leading to angle closure glaucoma. We initially chose not to undergo peripheral iridectomy, but the incidence of postoperative ocular hypertension was higher in patients who did not undergo peripheral iridectomy than in those who underwent peripheral iridectomy. The incidence of postoperative intraocular hypertension was 50% and 6.67%, respectively. Among them, there was one case without peripheral iridectomy, which caused ciliary ring block glaucoma due to the complete closure of the anterior chamber angle. Finally, vitrectomy combined with peripheral iridectomy was performed. Our research suggests that anterior chamber air injection with iridectomy may be more effective in preventing complications.
This study also has some limitations, including its retrospective design and small sample size. Given the rarity of DMD, future multicenter prospective studies are needed to validate our findings. Due to short follow-up time, the incidence of postoperative ocular hypertension and other complications is not necessarily accurate, and the safety of its surgical method needs to be evaluated. In the future, we will increase the number of patients and continue to collect cases and follow up to verify its safety and identify other complications.
CONCLUSION
This study confirms the efficacy of anterior chamber air injection combined with scleral tunnel peripheral iridectomy for treating DMD. The results demonstrate that the combined treatment group achieved a high postoperative DMD reattachment rate while effectively preventing serious complications such as glaucoma. The innovative scleral tunnel incision technique avoids the DMD lesion area, significantly reducing the risk of intraoperative secondary damage. Although limited by its retrospective design and sample size, this study provides important evidence-based support for DMD treatment. In cases unresponsive to conservative treatment, the combined approach of scleral tunnel incision with anterior chamber air injection and peripheral iridectomy not only achieves high reattachment rates but also markedly reduces postoperative complications, establishing it as a safe and effective treatment protocol. Future multicenter studies are needed to validate its long-term efficacy further.
AUTHORS’ CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: M.Z., J.K.: Study conception and design; B.T., R.L., and H.W.: Data collection; J.K., M.Z. and F.L.: Analysis and interpretation of results; J.K. and M.Z.: Draft manuscript. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| DMD | = Descemet’s Membrane Detachment |
| SD | = Standard Deviation |
| CF | = Count Fingers |
| FECD | = Fuchs Endothelial Corneal Dystrophy |
| PKP | = Penetrating Keratoplasty |
| EK | = Epithelial Keratomileusis |
| SF6 | = Sulfur Hexafluoride |
| IOP | = Intraocular Pressure |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This retrospective study was approved by the ethics committee of the Hainan Eye Hospital, China. The approval number of the Ethics Committee is: 2024-028-01.
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
The study is supported, in parts, by 1) an unrestricted grant from the National Natural Science Foundation of China, (82060176), 2) Natural Science Foundation of Hainan Province, China (No: 822MS190), and 3) Hainan Province Eye Clinical Medical Center, China.
ACKNOWLEDGEMENTS
Declared none.


