LETTER
Anomaly of the Deep Lateral Orbital Wall in Two Cases
Hirohiko Kakizaki*, 1, Akihiro Ichinose2, Yasuhiro Takahashi1, Masayoshi Iwaki 1
Article Information
Identifiers and Pagination:
Year: 2011Volume: 5
First Page: 25
Last Page: 26
Publisher ID: TOOPHTJ-5-25
DOI: 10.2174/1874364101105010025
Article History:
Received Date: 13/10/2010Revision Received Date: 30/12/2010
Acceptance Date: 3/3/2011
Electronic publication date: 14/4/2011
Collection year: 2011

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http: //creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
TO THE EDITOR,
Deep lateral orbital wall decompression is considered the first choice procedure [1] in treating disfiguring proptosis, as well as, compressive optic neuropathy and congestive orbitopathy [2,3]. Although detailed normal anatomy of the deep lateral orbital wall has already been reported [1,4,5], there are no reports of anomalies of the wall. We experienced two types of anomalies of the deep lateral orbital wall in patients who underwent deep lateral orbital wall decompression.
The first patient was a 35 year-old woman who showed bilateral orbital inflammation from Graves’ orbitopathy, and underwent 2 cycles of steroid pulse therapy (1 cycle: methylprednisolone 10 mg/kg/day × 3 days). Although the inflammation subsided completely after the therapy, her Hertel exophthalmometry measurements remained 21 mm OU. Therefore, she hoped to have orbital decompressions to both orbits. We performed bilateral deep lateral orbital decompressions and her final Hertel measurements improved to 14 mm OD and 13 mm OS.
She demonstrated bilateral bone defects of the inferior part of the sphenoid door jamb without tumor invasion as shown by preoperative computed tomography (CT) (Fig. 1A). During the operations, the defects were clearly identified and no tumor invasion was found, consistent with CT. (Fig. 1B). The bone defects continued to the inferior orbital fissure, and the orbital fat was herniated into the defect, continuing to the buccal fat.
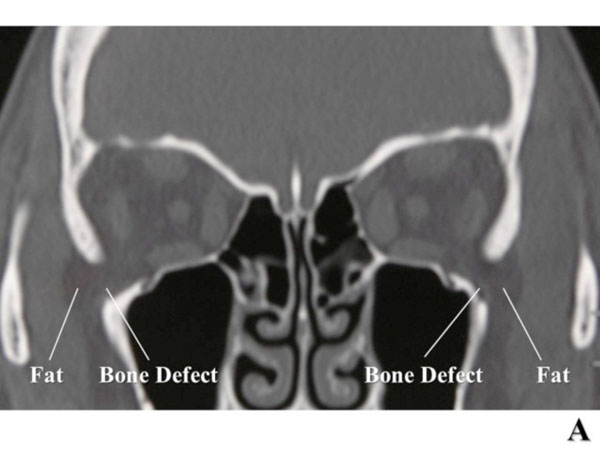 |
Fig. (1A). Bilateral defects of the inferior part of the sphenoid door jamb are shown on computed tomography (CT). |
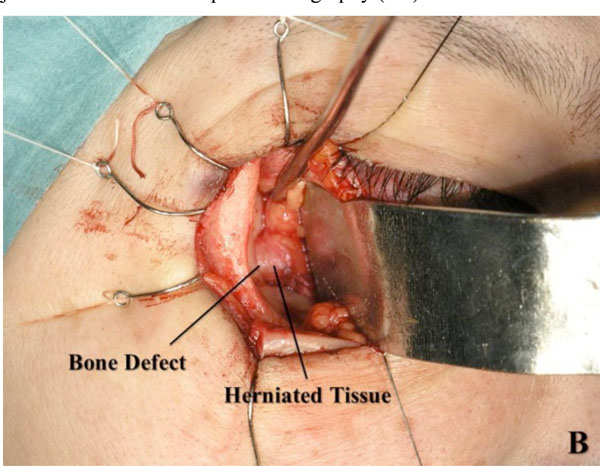 |
Fig. (1B). A defect is identified during deep lateral orbital wall decompression surgery. |
 |
Fig. (2A). A cystic formation in the left lower part of the sphenoid door jamb is shown on axial computed tomography (CT). |
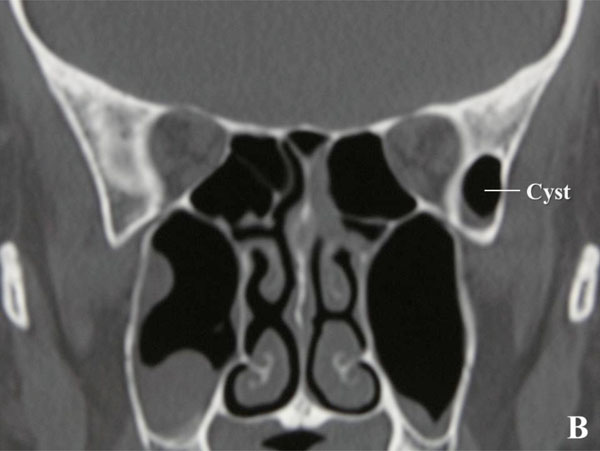 |
Fig. (2B). Coronal CT is unable to show continuity from the cyst to the maxillary sinus. |
 |
Fig. (2C). The cyst continues to the maxillary sinus. |
The other patient was a 40 year-old woman who suffered from Graves’ orbitopathy with left orbital inflammation. She also underwent 2 cycles of steroid pulse therapy. The inflammation subsided completely, but her Hertel exophthalmometry measurements remained at 16 mm OD and 18 mm OS. She hoped to have a left orbital decompression. We performed a left deep lateral orbital decompression and her final left Hertel measurement was 15 mm.
She showed a cystic formation with a little fluid collection in the left lower part of the sphenoid door jamb as shown by preoperative CT (Fig.2A). The cyst was separated by a thin cortical bone to the middle cranial fossa and it was filled with air without fluid. During the deep lateral orbital wall decompression surgery, the cyst was clearly identified, and the inner wall was lined by thin paranasal sinus mucosa. With enlarging the cyst and following it inferiorly, it was found to continue to the maxillary sinus (Fig.2B). No osteolytic lesion was found in the operation. The cyst was an expansion of the maxillary sinus.
The first anomaly described above, a defect in the bones, continued to the extraorbital space, and the orbital fat was directly connected with the buccal fat. Therefore, the orbital space was easily enlarged during decompression surgery by removing the buccal fat, and the orbital fat was also easily removed by incising the periosteum around the bone defect.
The second anomaly described above—an expansion of the maxillary sinus—enabled the present surgeon to perform a decompression surgery safely and efficaciously. Since the space was only divided by a thin cortical bone to the middle cranial cavity, maximum bone removal could be achieved by tracing the cortical bone superiorly with bone gliding.
Knowledge of anomalies of the deep lateral orbital wall presented here could be helpful for other surgeons to perform a safe and efficacious deep lateral orbital wall decompression surgery.






