All published articles of this journal are available on ScienceDirect.
Choroidal Neovascularization Following Implantation of Verisyse™ Iris-Supported Phakic Intraocular Lens in a Pregnant Myopic Patient
Abstract
Both choroidal neovascularization during pregnancy, and choroidal neovascularization following implantation of phakic intraocular lenses have been reported in the literature. To our knowledge, this is the first case reported of a gravid woman developing choroidal neovascularization in an eye with a phakic intraocular lens. A 31-year-old woman became aware of her pregnancy three weeks after placement of the Verisyse™ iris-supported phakic intraocular lens. She was at 15 weeks gestation when she developed a Fuch’s spot consistent with choroidal neovascularization. By eight months gestation, her symptoms nearly resolved. While the development of choroidal neovascularization in this patient may appear incidental, women of childbearing age considering phakic intraocular lenses warrant additional discussion on the possible increased likelihood of choroidal neovascularization.
INTRODUCTION
It has long been known that pregnancy has an impact on various diseases including hypertension, diabetes, and graves disease. It can also precipitate disease, as in pregnancy-induced-hypertension and gestational diabetes. Very little has been written concerning choroidal neovascularization (CNV) in pregnancy. One case report describes CNV as a complication of pre-eclampsia in a patient with antiphospholipid syndrome [1]. Another publication looked at the association between development of CNV and pregnancy [2]. There have also been case reports of CNV occurring in myopes receiving phakic intraocular lenses [3-6]. To our knowledge, no cases have reported CNV in a pregnant patient with the Verisyse™ (Abbott Medical Optics Inc. Abbott, IL, USA) iris-supported phakic intraocular lens (IOL). While no current evidence exists showing a correlation, such an association would have an impact on advising women of childbearing age considering anterior chamber intraocular lenses for vision correction.
CASE REPORT
A 39-year-old woman with a manifest refraction (MR) of -14.25+1.50x53º, and a corrected distance visual acuity (CDVA) of 20/20 OS, underwent surgery with placement of a -14.00 diopter iris-supported phakic IOLs (Verisyse™) without knowing she was pregnant. Resultant uncorrected distance visual acuity (UDVA) was 20/30. Three weeks after Verisyse™ implantation she became aware of her pregnancy and was determined to be at 15 weeks gestation. At this time, she developed acute vision loss in the left eye. She reported seeing a dark blue/brown circle in her central vision, and blurriness without pain. The patient denied trauma or flashes of light. Her only medications were a daily prenatal vitamin and artificial tears as needed. On examination her CDVA was 20/60 OS with mild metamorphopsia. Anterior segment exam showed a well-positioned Verisyse™ lens. Fundoscopic exam of the left eye revealed a small area of hemorrhage directly in the fovea, consistent with a Fuch’s spot (Fig. 1). Stratus optical coherence tomography (Carl Zeiss Meditec, Dublin, CA) demonstrated findings consistent with CNV (Fig. 2). She had a normal optic disc size, shape, and color, with sharp margins and a cup-to-disc ratio of 0.2. The major retinal vasculature appeared to be normal. In the foveal region, pigmentary mottling and some intraretinal hemorrhage extended temporal to the fovea. Fluorescein angiography and visudyne photodynamic treatment were not done due to the pregnancy. The plan was observation and to return if vision worsened. Her vision stabilized one month later, and UDVA remained 20/60. Two months after her onset of symptoms (23 weeks gestation), UDVA improved to 20/40 with less distortion and blurriness. Dilated fundus exam showed subtle hemorrhages just temporal to the fovea.
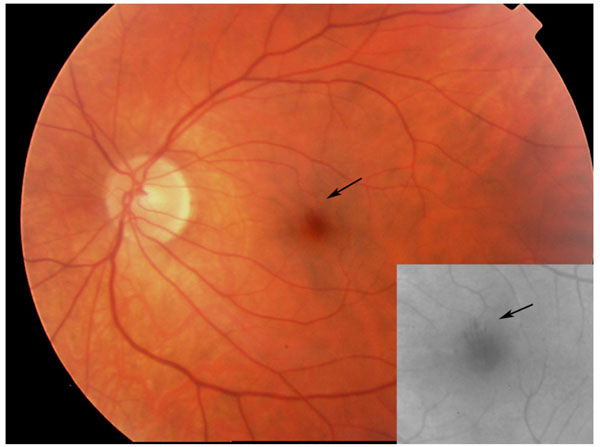
Color fundus photograph and red free fundus photograph (insert) of the left eye taken at 15 weeks pregnant showing a Fuch’s spot with hemorrhage (arrows) over the fovea.
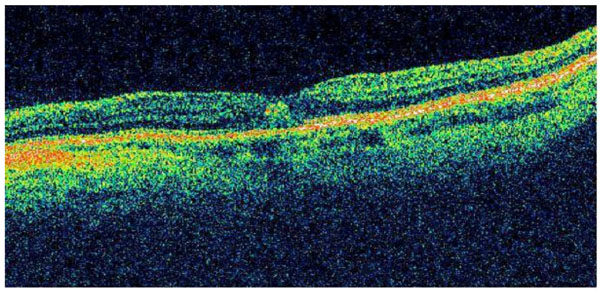
Optical coherence tomography of the left eye demonstrating a subfoveal lesion consistent with CNV.
There was concern that valsalva manouvres during vaginal delivery might lead to increased retinal bleeding, therefore, cesarean section was performed at term. By phone interview one week after delivery, she reported her vision was near baseline and there was only slight distortion on using Amsler grid.
DISCUSSION
Choroidal neovascularization following correction of high myopia with phakic intraocular lenses has been reported to develop in 1.70% to 2.38% of patients [3, 5, 6]. Time to development of CNV from implantation has been reported to range from 1-87 months with an average time of 33 months [6]. Choroidal neovascularization in pregnancy has also been reported to develop around the 6th month of pregnancy [1, 2]. To our knowledge, this is the first report of CNV developing in a gravid patient with an anterior chamber phakic intraocular lens. Current guidelines recommend against implantation of the Verisyse™ lens if a woman is pregnant or nursing [7]. Complications from surgery may require medications that can cross the placenta and affect the fetus, or be transmitted through breast milk to the infant.
Other than being highly myopic, our patient had no other known risk factors to explain the development of CNV during her pregnancy. The phakic lens, pregnancy, high myopia, undiagnosed lacquer cracks, or a combination of these may have caused the CNV. Further research is needed to help elucidate these complex relationships. We are reporting this case in an attempt to alert the surgeon of a potential increased risk of CNV, should a woman become pregnant after receiving a phakic anterior chamber lens.
ACKNOWLEDGEMENT
None declared.
CONFLICTS OF INTEREST
None declared.


