All published articles of this journal are available on ScienceDirect.
Transient Cystoid Macular Oedema in Multiple Choroidal Naevi
Abstract
Choroidal Naevi are generally thought to be trivial. However, sometimes they cause visual loss, visual filed defect and rarely transform into malignant melanoma. We report the first case of unilateral numerous choroidal naevi in a healthy female associated with transient cystoid macular oedema and postulate about its pathogenesis.
CASE-REPORT
A 48-year-old female presented with three weeks history of left eye blurred vision. She had no previous ophthalmic or medical problems and was not on any medications. Visual acuity (VA) at presentation was 6/5 right and 6/9 left eye. External ocular and anterior segment examination was normal. Dilated funduscopy of left eye showed numerous flat, pigmented choroidal lesions with indistinct border suggestive of choroidal naevi in the posterior pole and inferior retina with cystoid macular oedema (CMO) (Fig. 1). Fluorescein angiography confirmed CMO with retinal capillary leakage (Fig. 2). Right eye was normal. Examination and investigations by a physician to exclude systemic malignancy were normal. Laboratory tests and electrodiagnostic tests were normal. Six months later, CMO resolved spontaneously and VA improved to 6/5. Six years later, She remains well, choroidal naevi are unchanged and VA is 6/5 OU.
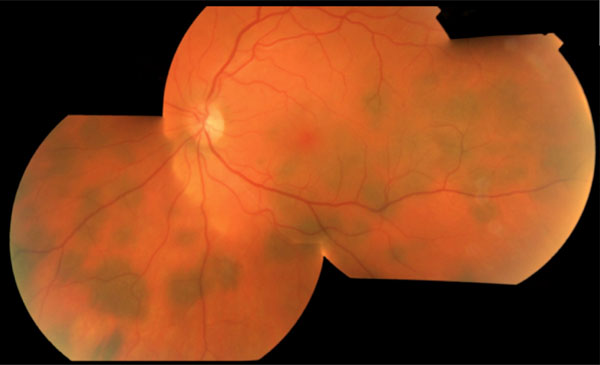
Coluor fundus photograph of left eye showing numerous choroidal naevi.
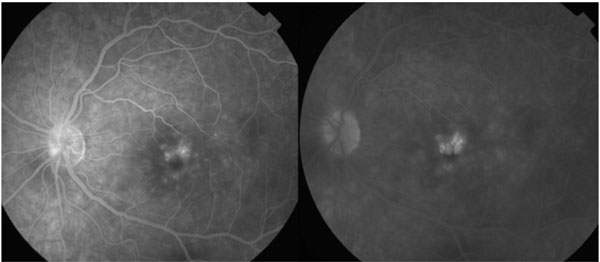
Right; shows retinal capillary leakage on fluorescein angiography of the left eye. Left; shows late phase fluorescein angiography with CMO.
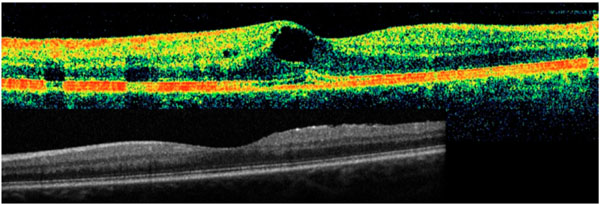
Top; Stratus OCT through fovea shows CMO. Bottom; HRA OCT through fovea showing absence of RPE/photoreceptor layers irregularities following resolution of CMO.
DISCUSSION
CMO represents the common final pathway of a heterogenous group of processes. The tight junctions between retinal pigment epithelial cells (RPE) and retinal capillary endothelial cells can be disturbed in disease process and by cytokines [1].
Choroidal naevi can induce histologic changes in their neighbouring tissues such as narrowing or complete obliteration of the choriocapillaris, degeneration or proliferation of RPE and photoreceptors disturbances [2]. Shield et al. have reported on the presence of retinal oedema overlying a choroidal naevus with associated RPE/choriocapillaris irregularities in 15% of their patients when examined with Optical coherence tomography (OCT) [3].
Multiplicity of choroidal naevi to this extent is unusual. Shield et al. reported a maximum of 10 naevi in less than 1% of their 3422 studied eyes [4].
Multiple naevus-like lesions as a result of proliferation of benign melanocytes in the outer choroid occur in bilateral diffuse uveal melanocytic proliferation. It is a very rare paraneoplastic syndrome occurring in elderly patients with advanced systemic malignancy [5]. This case's clinical picture and outcome are clearly different from this condition.
In this patient, choroidal naevi were scattered in the parafoveal and peripheral retina but spared the fovea. Spectral domain OCT did not show any disturbance of overlying RPE and photoreceptor layer (Fig. 3). There were no other pathologic findings to explain the CMO. In the absence of detectable changes in RPE and photoreceptor layers, we postulate that altered cytokine milieu might have caused the CMO and its subsequent resolution. Nevertheless, unilateral or bilateral macular oedema may occur with no identifiable cause. In some idiopathic cases the oedema may resolve spontaneously or in some others persist despite treatment [6]. Although this case may belong to this category, one would naturally like to speculate about the pathogenesis of unilateral macular oedema in such a rare condition.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
ACKNOWLEDGEMENTS
Declared none.


