All published articles of this journal are available on ScienceDirect.
Corneal Collagen Cross-Linking Mushroom Shape Demarcation Line Profile After Limited Bowman’s Membrane Removal by Phototherapeutic Keratectomy
Abstract
Purpose :
To report a corneal collagen cross-linking (CXL) mushroom shape demarcation line profile after limited Bowman’s membrane removal by phototherapeutic keratectomy (PTK).
Methods :
Case report.
Results :
A twenty-one-year-old male with progressive keratoconus underwent mechanical epithelial debridement (at an 8.5 mm zone) followed by PTK (at a 5.0 mm zone and in a 10 μm depth) and CXL. No intra- or early postoperative complications were found. Evaluation of the corneal stromal demarcation line depth using anterior segment optical coherence tomography revealed a mushroom shape profile.
Conclusion :
It seems that removal of the Bowman’s layer leads to greater depth of the corneal stromal demarcation line.
INTRODUCTION
Excimer laser phototherapeutic keratectomy (PTK) is a surgical procedure that has been applied for the treatment of anterior corneal diseases, including anterior corneal dystrophies, degenerations, recurrent corneal erosions and corneal scars [1]. Corneal collagen cross-linking (CXL) is a surgical method, which is used to increase corneal rigidity and halt the keratoconus progression [2]. Phototherapeutic keratectomy is combined with corneal collagen cross-linking in order to improve the visual and refractive outcomes of CXL [3-5]. After application of CXL, anterior stromal alterations caused by the treatment produce a corneal stromal demarcation line, which is identified clinically in slit-lamp examination, or with the use of imaging techniques, such as confocal microscopy and anterior segment optical coherence tomography (AS-OCT) [6-10].
In the current article, we report a case of a patient with keratoconus, who was treated with mechanical epithelial debridement (at an 8.5 mm zone) followed by limited PTK (at a 5.0 mm zone and in a 10 μm depth) and CXL. AS-OCT revealed a mushroom shape demarcation line profile indicating the possible role of the Bowman’s layer removal for greater corneal stromal demarcation line depth.
CASE REPORT
A twenty-one-year-old male patient with topographically confirmed progressive keratoconus presented to our institute for consultation. During examination, his uncorrected distance visual acuity (UDVA) was 20/63 in the right and 20/250 in the left eye, while corrected distance visual acuity (DCVA) was 20/20 in both eyes. Keratometric readings were 46.13 / 42.40 and 43.62 / 42.82 in the right and the left eyes, respectively. Corneal topography revealed a centrally located corneal cone configuration. The corneal pachymetric values, estimated with the use of ultrasound, were 472 nm in the right eye, and 504 nm in the left eye. The keratoconus was graded as stage 2, according to the Amsler – Krumeich classification. Slit-lamp examination of anterior segment and fundoscopy did not reveal any pathological features. The patient underwent uneventful CXL treatment in his right eye.
SURGICAL TECHNIQUE
After instillation of proxymetacaine hydrochloride 0.5% eyedrops (Alcaine; Alcon Laboratories, Inc, Fort Worth, Texas, USA) as a topical anaesthetic, corneal epithelium debridement was achieved with the use of a rotating brush at an 8.5 mm zone. After mechanical epithelial removal, PTK was performed at a 5.0 mm zone in a 10 μm depth. After PTK, riboflavin (0.1% solution of 10 mg riboflavin-5-phosfate in 10 ml dextran-T-500 20% solution, Medicross, Medio - Haus, Behrensbrook, Neudorf, Germany) was applied repeatedly on the central cornea every 3 minutes for a duration time of approximately 30 minutes. The cornea was irradiated with Ultraviolet-A (UV-A) illumination with the use of an UV-A optical device (CCL-365, Peschke Meditrade GmbH, Huenenberg, Switzerland). Before treatment, the device was calibrated using the UV-A light meter YK-35UV (Lutron Electronic, Coopersburg, PA), which is supplied with the UV-X device, in order to ensure that the irradiance was 3.0 mW/cm2, as intended. Total irradiance time was 30 minutes, as required in order to administer a total surface dose of 5.4 J/cm2. During UV-A irradiation procedure, riboflavin solution instillation was continued repeatedly every 3 minutes to maintain corneal saturation with riboflavin. At the end of the procedure, a silicone-hydrogel (Lotrafilcon B, Air Optix, Ciba Vision - 14.0 mm diameter, 8.6 base curvature, Dk=140 barrers) bandage contact lens (BCL) was applied until complete epithelium healing.
One month after the treatment CXL procedure, UDVA was improved at 20/40 and CDVA remained stable at 20/20. Slit-lamp biomicroscopy revealed a clear cornea. Anterior segment optical coherence tomography (AS-OCT) was performed in order to identify and measure the depth of the corneal stromal demarcation line depth produced by CXL treatment. Corneal stromal demarcation line depth was measured centrally, at 2.0 mm (4.0 mm diameter) and at 2.5 mm (5.0 mm diameter) nasally and temporally, as described in our previous study [9]. Corneal stromal demarcation line depth was 398 μm centrally, 384 μm and 383 μm at 2.0 mm, 197 μm and 189 μm at 2.5 mm, nasally and temporally, respectively.
DISCUSSION
Excimer laser PTK is a surgical procedure that has been successfully applied for the treatment of anterior corneal pathology, including anterior corneal dystrophies, degenerations corneal scars and recurrent corneal erosions [1]. CXL is a surgical method used to increase the corneal rigidity, stabilize the ectatic cornea and arrest the keratoconus progression [2]. PTK is combined with CXL in order to remove the epithelium, smoothen the anterior corneal surface and decrease the irregular astigmatism induced by the keratoconus [3-5].
Two weeks after CXL, a corneal stromal demarcation line can be identified clinically during slit-lamp examination in a depth of approximately 300μm [6], or with the use of imaging modalities, such as confocal microscopy and AS-OCT representing the depth of the CXL treatment [7-10]. Recently, we showed that both confocal microscopy and AS OCT have similar accuracy in the evaluation of the depth of the corneal stromal demarcation line produced with CXL treatment [10].
In the current case report, a patient with progressive keratoconus is presented, who underwent mechanical epithelial debridement followed by limited PTK and CXL. The aim of combining PTK with CXL at the given size was to demonstrate the increase in treatment depth of CXL after Bowman’s layer removal. One month postoperatively, AS-OCT revealed a mushroom demarcation line profile (Fig. 1); corneal stromal demarcation line depth was greater centrally and at 2.0 mm (nasally and temporally) than at 2.5 mm (nasally and temporally).
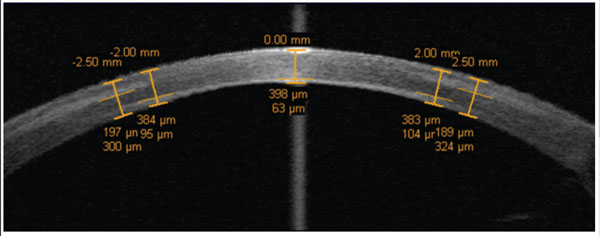
High resolution anterior segment corneal optical coherence tomography scan demonstrating the corneal stromal demarcation line one month after mechanical epithelial debridement followed by phototherapeutic keratectomy and corneal collagen cross-linking in a patient with progressive keratoconus with depths of 398 μm (centrally), 384 μm and 383 μm (at 2.0 mm nasally and temporally, respectively), 197 μm and 189 μm (at 2.5 mm nasally and temporally, respectively).
A possible explanation of this configuration could be the Bowman’s membrane removal. Kolozsvari et al. have shown that Bowman’s layer absorb high amounts of UV irradiation [11]. Therefore, it seems that removal of the Bowman’s layer in our patient increased UV-A penetration in the corneal stroma leading to greater corneal stromal demarcation line depth in the PTK ablated central corneal area. In addition, it is possible that Bowman’s removal may induce corneal thinning through enhanced evaporation. Even though the role of Bowman’s layer in the CXL procedure is unknown this finding indicates indirectly that Bowman’s layer removal could increase the depth of CXL treatment.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
Declared none.


