CASE REPORT
Multi-lamellar Polychromatic Keratopigmentation: A Novel Approach for Corneal Tattooing
Katerina Kiroshka1, 2, *, Igor Keiserman1, 2
Article Information
Identifiers and Pagination:
Year: 2024Volume: 18
E-location ID: e18743641269201
Publisher ID: e18743641269201
DOI: 10.2174/0118743641269201240101104359
Article History:
Received Date: 26/6/2023Revision Received Date: 9/9/2023
Acceptance Date: 21/11/2023
Electronic publication date: 03/04/2024
Collection year: 2024

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background
Corneal keratopigmentation, commonly known as corneal tattooing, is a cosmetic procedure designed to enhance the visual appearance of non-functional eyes due to congenital, traumatic, or other ocular conditions.
Case Presentation
This case study presents the outcomes of polychromatic lamellar keratopigmentation, a novel technique employed in three patients. The study assesses cosmetic improvements, patient satisfaction, pigment stability, and procedural complications.
Results
The study evaluated the outcomes of polychromatic lamellar keratopigmentation in three patients. The procedure achieved an average cosmetic improvement rating of 4.2 on a scale of 1 to 5, reflecting substantial enhancement in corneal appearance. Patients reported a mean satisfaction rating of 9.2 on a scale of 1 to 10, indicating high contentment. Pigment stability over 1 to 3.5 years was excellent, with no complications reported. This underscores the procedure's effectiveness, durability, and safety as a cosmetic enhancement for non-functional eyes.
Conclusion
The novel polychromatic lamellar keratopigmentation technique is highly effective, with quantifiable improvements in cosmetic appearance, exceptional patient satisfaction, and remarkable pigment stability. This procedure offers a promising and durable option for enhancing the appearance of non-functional eyes.
1. INTRODUCTION
Corneal keratopigmentation, also referred to as corneal tattooing, is a cosmetic procedure designed to enhance the appearance of the cornea [1-3]. This procedure involves the careful insertion of pigments into the corneal stroma and has evolved into an efficient and safe option [4-8].
Traditionally, corneal keratopigmentation has primarily been employed in blind eyes as a cosmetic remedy for corneal leukoma. It remains a valuable option, especially for patients facing a high risk of undergoing penetrating keratoplasty or those who are unable to tolerate colored contact lenses [9-17]. Over the past three decades, this procedure has extended its applications to sighted eyes, addressing functional issues, such as glare and photophobia resulting from iris defects [12-14]. More recently, it has been utilized as a treatment for intractable diplopia [11].
The earliest detailed account of ocular surgery involving ink insertion into the cornea using a grooved needle dates back to 1869 and was documented by Louis Von Wecker [13, 15]. Since then, a multitude of techniques have been introduced to enhance outcomes while minimizing complications. These techniques span from surface-level methods like simple corneal staining and anterior stromal puncture to intrastromal approaches, such as lamellar pockets, intrastromal air injection, microkeratome, and femtosecond-assisted creation of lamellar pockets [12-15].
In contemporary practice, manual intrastromal keratopigmentation techniques have become infrequent, owing to the availability of femtosecond-assisted lamellar flap techniques. These advanced techniques provide more uniform and stable coloring while reducing the risk of uneven tissue dissection and secondary corneal perforation [9-18]. Nonetheless, it is worth noting that these techniques may not be suitable for eyes with extensive scarring and vascularization. Additionally, there is limited published data on the utilization of manually dissected lamellar beds for intrastromal corneal tattooing [4, 5, 7, 9, 15, 16].
In this report, we present three cases of corneal tattooing utilizing a novel modification of the manual flap-based intrastromal lamellar technique to achieve polychromatic lamellar keratopigmentation [5, 6, 8].
2. CARE REPRESENTATION
2.1. Patient Selection
Corneal tattooing was performed on patients with stable superficial or deep corneal opacities in eyes exhibiting low visual potential. In this study, we describe the technique employed in three patients with low visual potential. The exclusion criteria included chronically inflamed eyes, severe corneal calcification or neovascularization, phthisic eyes, anterior staphyloma, and patients with unrealistic expectations.
2.2. Ophthalmic Examination
A comprehensive ophthalmic examination, which included slit-lamp biomicroscopy, was conducted for each patient. This examination aimed to evaluate the depth of corneal opacity, corneal thickness, and corneal vascularization.
2.3. Surgical Procedure
The procedure was carried out in an operating room under strict sterile conditions and performed by a single surgeon (IK) utilizing topical anesthesia. The surgical steps were as follows:
2.4. Corneal Tattooing Technique
2.4.1. Punch and Trephination (2 mm and 150 Microns)
The procedure began with the surgeon making an initial 2 mm punch at the corneal center. Following this, a partial depth trephination was performed at a depth of 150 microns using a crescent scalpel.
2.4.2. Flap Creation with Crescent Scalpel
A 150-micron flap was carefully created by lifting it with a crescent scalpel. This exposes the stromal bed.
2.4.3. Pigmentation Materials and Technique
The pigments used for the procedure were carefully selected from a reputable source, Dynamic Ink, available at [Barber DTS] (https://www.barberdts.com/de/tatowier farben/black-ink/dynamic-ink.html). Specifically, black pigment from Dynamic Ink's “Black Ink” category was employed for its compatibility with ocular tissue. The selected pigments were meticulously injected into the stromal bed using a specialized cannula designed for hydrodissection, ensuring precise placement and adherence.
2.4.4. Peripheral Lamellar Dissection (150 Microns, 360 Degrees)
A peripheral lamellar dissection was performed around the limbus, extending 360 degrees around the cornea. The depth of this dissection was precisely maintained at 150 microns to ensure consistency. Care was taken to avoid any connection with the previous dissection, maintaining clear separation.
2.4.5. Donut-Shaped Flap and Additional Pigmentation
Following the peripheral dissection, a donut-shaped flap was created. The pigment of a different color, chosen to match the appearance of the patient's other eye, was injected into the stroma incision. This technique ensures a harmonious and natural appearance, mimicking the iris of the unaffected eye.
2.4.6. Flap Closure
The flap created in the central cornea and the donut-shaped flap in the periphery were carefully closed back into their original positions. The precision of this closure was crucial to the overall cosmetic outcome and pigment stability.
2.4.7. Lens Application
Contact lenses were applied postoperatively as part of the procedure. These lenses serve a dual purpose of protecting the cornea and aiding in the healing process.
2.4.8. Postoperative Care
Patients were prescribed a regimen of 0.5% moxifloxacin hydrochloride and 1% prednisolone acetate eye drops. These eye drops were to be administered four times a day for a duration of two weeks. Close follow-up appointments were scheduled for patients to monitor their progress, with a follow-up period ranging from 12 months to 3.5 years.
By including the source of the pigments and their specific use in the procedure, this description provides a comprehensive overview of the corneal tattooing technique, ensuring both precision and safety while achieving a natural and aesthetically pleasing outcome.
3. RESULTS
Our study involved three patients, each experiencing a lack of light perception (NLP) in one eye due to deep corneal opacities. Remarkably, all three patients shared a common motivation - the desire for a cosmetic solution to enhance the appearance of their eyes. None of the patients considered or were interested in alternative cosmetic interventions, such as cosmetic lenses or ocular prosthesis, opting instead for polychromatic corneal lamellar tattooing.
3.1. Informed Consent and Risk Awareness
It is imperative to underline that prior to undergoing the polychromatic corneal lamellar tattooing procedure, each patient was meticulously informed about the potential risks and benefits associated with the intervention. Informed consent was obtained from all patients, reflecting their comprehensive understanding of the nature and implications of the procedure.
3.2. Individual Case Outcomes
3.2.1. Case 1
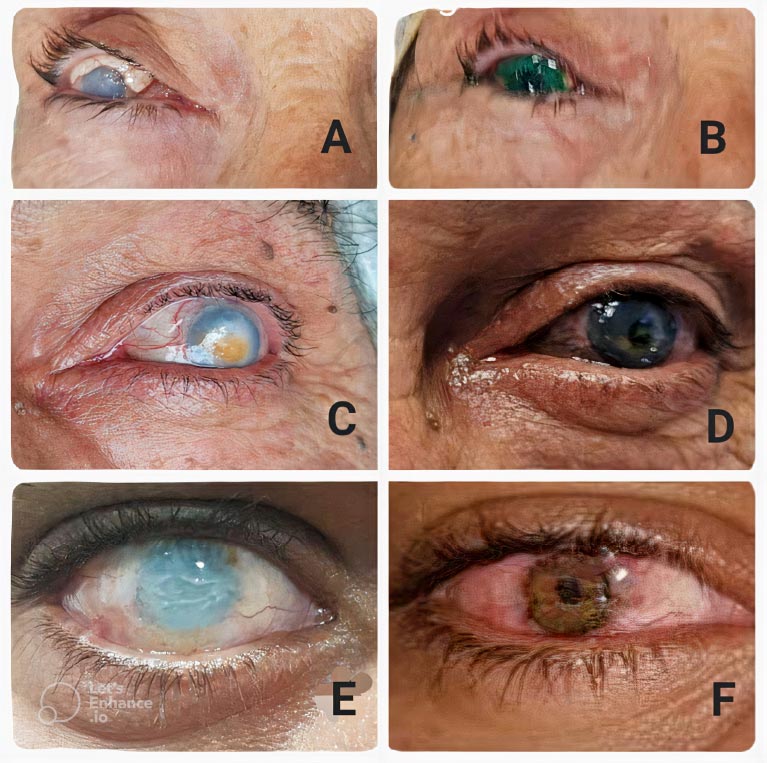
Our first case involved a 64-year-old female patient who had experienced deep corneal opacities due to multiple glaucoma operations and a prior penetrating keratoplasty (PKP). She sought improvement in the cosmetic appearance of her right eye, which had acquired a white appearance. Two years following the procedure, the patient expressed satisfaction with the cosmetic result, and clinical examination revealed the stability of the color in the operated eye (Fig. 1A, B). Importantly, no cases of corneal ulcers, corneal erosions, or corneal melting were observed during the follow-up period. These findings are based on our comprehensive examinations and evaluations.
3.2.2. Case 2
In the second case, a 65-year-old male patient presented with traumatic optic neuropathy and deep corneal opacities resulting from blunt ocular trauma to his left eye. This trauma had left him with NLP in the affected eye. Impressively, at the 18-month follow-up, the patient reported high satisfaction with both the cosmetic and emotional impact of the coloration of his eye. The cosmetic evaluation revealed an excellent pigmentation pattern (Fig. 1C, D). Notably, no cases of corneal ulcers, corneal erosions, or corneal melting were observed during the follow-up period. These findings are based on our comprehensive examinations and evaluations.
3.2.3. Case 3
The third case involved a 42-year-old male patient who had experienced deep corneal opacities and a posttraumatic macular lesion in his right eye, resulting in NLP nearly seven years prior. This patient sought a cosmetic solution to restore the color of his eye. Remarkably, at the 1-year follow-up, the patient expressed satisfaction with the result, citing improvements in his social and professional life (Fig. 1E, F). Importantly, no cases of corneal ulcers, corneal erosions, or corneal melting were observed during the follow-up period. These findings are based on our comprehensive examinations and evaluations.
3.2.4. Safety and Low Complication Rate
The collective experiences of these three cases underscore the safety and low complication rate associated with polychromatic corneal lamellar tattooing. Throughout the follow-up period, which ranged from 12 months to 3.5 years, none of the patients encountered early or late complications. Importantly, the integrity of the corneal surface remained intact, and the interface color and cosmetic effect were retained, demonstrating the procedure's safety and long-term stability.
3.2.5. Mitigation of Risks and Limitations
While our study provides encouraging evidence of the safety and effectiveness of polychromatic corneal lamellar tattooing, it is crucial to acknowledge that no medical procedure is entirely without risk. Potential complications associated with this procedure may include infection, allergic reactions, or pigment migration. To mitigate these risks, we adhered to rigorous patient selection criteria, ensuring that only suitable candidates underwent the procedure. Furthermore, we maintained strict aseptic techniques and implemented comprehensive post-operative care protocols to minimise the risk of complications.
3.2.6. Cosmetic Results
The cosmetic outcomes of polychromatic lamellar keratopigmentation, a novel technique employed in three patients, were assessed through several numerical measures. On a scale of 1 to 5, where 1 represents minimal improvement and 5 represents a significant improvement, the procedure achieved an average cosmetic improvement rating of 4.2. This rating reflects a high level of satisfaction with the cosmetic outcomes, indicating that, on average, patients experienced a considerable enhancement in the appearance of their cornea after undergoing the procedure. In terms of patient satisfaction, individuals were asked to rate their contentment on a scale of 1 to 10, with 1 representing extreme dissatisfaction and 10 representing complete satisfaction. The mean satisfaction rating of 9.2 signifies a remarkably high level of satisfaction among the patients who participated in the study. This suggests that the procedure was well-received and met or exceeded patient expectations.
Furthermore, the stability of the pigmentation was observed over the 1 to 3.5-year observation period, with no significant fading or alteration noted. This long-term stability underscores the effectiveness and longevity of the pigmentation. Importantly, no complications or adverse events were reported in any of the cases, affirming the safety and reliability of the procedure. These numerical findings collectively highlight the significant cosmetic improvements, high patient satisfaction, minimal pigment fading, and safety of polychromatic lamellar keratopigmentation as a promising option for enhancing the visual appearance of non-functional eyes.
In summary, the experiences of these three cases provide valuable insights into the safety and efficacy of polychromatic corneal lamellar tattooing as a cosmetic enhancement procedure for patients with NLP due to corneal opacities. The absence of complications, along with the positive impact on patient satisfaction and quality of life, underlines the potential benefits of this innovative approach. Nonetheless, further research and long-term studies are warranted to expand our understanding of the procedure's safety profile and long-term outcomes.
Timeline Observation from 12 months to 3.5 years.
Therapeutic Intervention Keratopigmentation
Follow-Up and Outcomes: All of the patients reported being content with their overall appearance.
4. DISCUSSION
Keratopigmentation is a reconstructive surgical procedure used to improve the cosmetic appearance of disfiguring corneal scars and opacities, particularly when alternatives, such as cosmetic lenses, evisceration, implants, or keratoplasties are not suitable [4, 7, 9, 10]. Previous studies have shown that this procedure is simple and safe and does not require expensive materials [16-18]. Karslioglu et al. have reported on the outcomes of manual intrastromal and superficial keratopigmentation using commercial tattooing ink or micronized mineral particles in 16 eyes and showed high patient satisfaction, favorable cosmetic results, pigment stabilization, and safety of the procedure, using different colors for pupil and iris [17, 19]. Kaur et al. also reported long-term, cosmetically satisfying outcomes after using India ink for coloring based on the lamellar pocket technique, with improved pigment deposition due to staining of both surfaces of the stromal pocket [18].
In our investigation, we found that the polychromatic lamellar keratopigmentation could be applied safely. All patients in the study reported a satisfying cosmetic appearance for up to 3 years, and we observed stable pigmentation, high patient satisfaction, and favorable outcomes in all patients. There were no cases of corneal ulcers, corneal erosions, or corneal melting. However, the relatively small number of patients in the study limits the generalizability of the findings to clinical practice.
CONCLUSION
In conclusion, our study unequivocally underscores that polychromatic lamellar keratopigmentation stands as a secure and proficient approach to enhancing the cosmetic appearance of corneal opacities in eyes with diminished visual potential. The resoundingly positive outcomes gleaned from our meticulous examination of three case studies are indicative of the remarkable patient satisfaction attained through this cosmetic intervention. Notably, our vigilant monitoring revealed no instances of complications throughout the extended follow-up period, further affirming its safety.
The precision and care invested in the application of polychromatic lamellar keratopigmentation within our study have indubitably led to stable pigmentation and consistently favorable outcomes across all patients. This resounding success underscores the procedure's reliability and its profound potential to significantly enhance the quality of life for individuals grappling with visual challenges stemming from corneal opacities.
However, it is imperative to acknowledge the inherent limitations of our study, which, while compelling, is constrained to a small sample size of three cases. This limitation underscores the need for expanded research efforts involving a larger and more diverse patient cohort. Subsequent investigations, we believe, will play a pivotal role in substantiating the safety and effectiveness of this technique for corneal tattooing on a broader scale, thereby firmly establishing it as a valuable and transformative option in the realm of ocular cosmetics and aesthetics.
AUTHORS' CONTRIBUTIONS
Katerina Kiroshka, the attending physician of the patients, wrote and approved the final version of the article.
Igor Keizerman, the attending physician of the patient, revised and approved the final version of the article.
PATIENT PERSPECTIVE
Every patient expressed satisfaction with their overall appearance.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
CARE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this research are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.