RESEARCH ARTICLE
Mono-canalicular Lacrimal Stent Intubation for Congenital Nasolacrimal Duct Obstruction Treatment
Ali Nema Abushnein1, Muthanna Basheer Yasir1, *, Wissam Yosif2
Article Information
Identifiers and Pagination:
Year: 2024Volume: 18
E-location ID: e18743641298283
Publisher ID: e18743641298283
DOI: 10.2174/0118743641298283240315153809
Article History:
Received Date: 22/11/2023Revision Received Date: 01/03/2024
Acceptance Date: 06/03/2024
Electronic publication date: 02/04/2024
Collection year: 2024

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background
Epiphora, marked by tear overflow at the eyelid margin, is a prevalent condition in ophthalmology, affecting over 20% of infants. The causes involve hypersecretion due to anterior segment diseases or compromised lacrimal drainage systems. While congenital nasolacrimal duct obstruction (CNLDO) in children often resolves spontaneously, persistent cases may necessitate surgical intervention. The management, which includes probing, stent insertion, and dacryocystorhinostomy, remains challenging due to the miniaturized and variable anatomy of the lacrimal pathways.
Objective and Aims
This study aims to investigate the efficacy of mono-canalicular Lacrijet stent insertion in managing congenital nasolacrimal duct obstruction (CNLDO) in pediatric patients, particularly those aged over 24 months. It focuses on assessing success rates in cases with prior probing or no previous probing. The study aims to contribute valuable insights to the existing literature on the effectiveness of Lacrijet intubation as a management option for CNLDO.
Patients and Methods
A prospective observational study following 25 pediatric patients diagnosed with epiphora in an ophthalmology hospital. The procedure included using mono-canalicular Lacrijet intubation. Patients were followed for 180 days post-operatively via subjective and objective measures. Independent and paired t-tests were used for numerical variables. Chi-square was applied to check the significant association of variables with outcome. A p-value less than or equal to 5% is considered significant.
Results
More than half of the sample was 3-6 years of age (56%), males (52%), and had previous probing attempts (56%). Seven (28%) patients were relieved from symptoms within less than 5 days, 12 (48%) recovered within 5-9 days, and 2 (8%) patients were symptom-free after 10 days. The success rate was 84%. Only 4 patients (16%) had unsuccessful outcomes. There was no significant difference in outcome regarding patients’ age, gender, affected eye, previous probing, and site of intubation.
Conclusions and Recommendations
Mono-canalicular Lacrijet stent insertion appears as a simple, safe, and reliable outpatient procedure for treating CNLDO in children. Age and prior failed probing did not significantly impact success rates. Early and detailed assessments are recommended for children with epiphora, with consideration for mono-canalicular stenting. Future research could compare outcomes between probing and intubation as initial treatments for pediatric epiphora.
1. INTRODUCTION
Epiphora, the overflow of tears at the eyelid margin, is a common presentation in ophthalmology clinics. It affects at least 20% of children in the first year of life, with spontaneous resolution occurring in approximately 85% within a year [1, 2]. Epiphora is mainly a result of two mechanisms: either hypersecretion secondary to anterior segment diseases such as dry eye (‘paradoxical watering’) or inflammation, or it is the consequence of a compromised lacrimal drainage system [1].
In children, congenital obstruction occurs due to unsuccessful canalization at any point along the drainage system, from the punctal region to the Hasner valve. Although the lower end of the nasolacrimal duct is usually the last portion of the lacrimal drainage system to canalize, complete patency most commonly occurs soon after birth [1]. The obstruction can result from the persistence of a membrane, narrowing of the inferior meatus, or bony obstruction [3]. While acquired nasolacrimal duct obstruction occurs due to infections and traumatic impediments [4].
Even though congenital nasolacrimal duct obstruction (CNLDO) is managed conservatively in the first year of life, it usually resolves naturally, matching the elongation and volume expansion of the nasolacrimal duct. Yet, in the case of the epiphora, which persists after the age of one year, it may require surgical intervention since the conservative treatment success rate declines with increasing age [5].
Management includes probing, stent insertion and dacryocystorhinostomy, either externally or endo-nasally [6]. Nasolacrimal stents are small tubes placed within the nasolacrimal system. The first stent dates back to 1932, and it was made by Graue using silver wire. Numerous substances have been used, like silk, nylon, polyethylene, and polypropylene. Today, the tubes are usually manufactured using silicone [7].
Unlike the Masterka, the Lacrijet system includes a longitudinally slit metal probe with the mono-canalicular stent inside it. Once the metal probe is positioned, the handpiece is withdrawn, the Monoka is released, and it remains in the desired position [8, 9]. It was specially designed for the treatment of epiphora, nasolacrimal duct obstruction, and canalicular stenosis and is also used for canalicular lacerations [7]. Although silicone is the ideal material in use, being an inert material that is flexible and can maintain an open lumen when placed, it can cause adverse reactions such as biofilm formation and tear flow resistance due to its extreme hydrophobicity [8].
Mono-canalicular stent intubation has been reported to be effective and mitigates the need for multiple staged surgeries. Epiphora receives growing attention worldwide due to the increase in air pollution levels. Additionally, managing epiphora in children is challenging because of the miniaturized and variable anatomy of the lacrimal drainage pathways [4, 8]. The study aims to explore the success of mono-canalicular insertion for CNLDO treatment in patients who underwent previous probing with no recovery or have not undergone prior probing, particularly in those over 24 months of age, where probing carries a low success rate.
2. PATIENTS AND METHODS
A prospective non-randomized observational study following a convenient sample of 25 pediatric patients diagnosed with epiphora in Ibn Al Haitham Teaching Eye Hospital for a period from the 24th of August 2022 to the 1st of November 2023.
Epiphora diagnosis relies on both a subjective assessment, which involved checking symptoms (such as epiphora, increased tear lake, and mucous discharge, monitored by the patient’s family), and an objective measurement of the tear meniscus height, which was conducted using slit lamp image analysis (the height of photographed tear meniscus was measured by using image J 1.53 image analysis software).
This study adhered to the principles outlined in the Declaration of Helsinki. It was conducted after gaining approval from the Ethics Committee on Human Research in Ibn Al Haitham Teaching Eye Hospital (Approval No. 206 on the 4th of July 2022). Additionally, both verbal and signed informed consent forms were obtained from the parents of the patients before they participated in the study. Parents' contact details were documented, and they were also informed about the aim of the study and the long follow-up period required for their participating children post-operatively to ensure no loss of following. A brief explanation of the procedure was provided. Also, the regular checkups needed post-operatively with careful recording and reporting on days of symptom improvements were affirmed. Case sheets were filled, and information was recorded pre and post-intervention. All data were kept anonymous, and no divulging of information occurred; it was only for research purposes.
2.1. Inclusion Criteria
All children aged 1-12 years who were admitted to Ibn Al Haitham Teaching Eye Hospital during the study period and were diagnosed with epiphora due to CNLDO.
The children who were less than three years of age, who had persistent epiphora in spite of previous probing and lacrimal sac massage and those aged 3 to 12 years who had previous probing or not were recruited.
2.2. Exclusion Criteria
Children with punctual atresia, canalicular obstructions (soft stops), bony or traumatic nasolacrimal duct obstruction, dysmorphic facial features, dacryo- cystoceles, dacryocystitis, down syndrome and previous tear duct surgery were excluded.
Fig. (1) depicts the procedure using a mono-canalicular Lacrijet intubation (0.64 mm stent diameter). Firstly, dilation of the punctum was done, and insertion of a sizer was performed, searching for a bony contact; this was followed by a rotation of 90 degrees and vertical catheterization through the insertion of a second wider lacrimal probe with a blunt tip. Steering it gently through
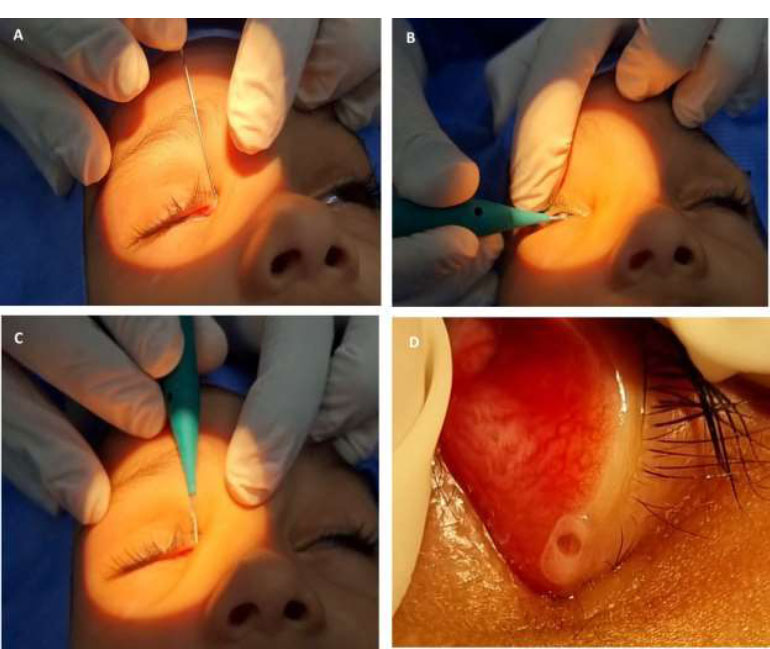 |
Fig. (1). Mono-canalicular Lacrijet intubation. (A). Lacrimal sizer, (B). Lacrijet insertion, (C). Rotation of 90 degrees, (D). Lacrijet installed. |
the inferior nasal meatus until metal-to-metal contact was achieved. Then, the appropriate mono-canalicular stent length was selected with the help of the black marks on the sizer. The silicone tube was then released and left in place to avoid future blockage.
At the end of the procedure, attention to the contact between the fixation head and the punctum is carefully ensured. The fixation plug was inserted into the punctum with the help of the plug inserter. Once the plug is in the right site, the collarette is maintained flush against the eyelid margin.
The follow-up period included both a subjective assessment, which involved checking symptoms, and an objective measurement of the tear meniscus height. The measurement of the tear meniscus height was done pre-operatively. Other measurements were performed on follow-up endpoints: at one month post-operative (30 days post-operatively), at three months (90 days post-operatively) and another measurement was performed at 120 days postoperatively, i.e., after stent removal, in order to avoid the possible effects of intubation-associated ductal inflammation on. The final measurement was done at 180 days postoperatively, and this measurement was compared statistically to the pre-operative tear meniscus height. The follow-up plan was as follows:
2.3. Pre-Op
A detailed history and examination, data collection regarding age, gender, previous probing, and affected eye were all documented. If there is evidence of conjunctivitis, Tobramycin Eye drops 1x3 were prescribed; Pre-op subjective and objective assessments (tear meniscus height measurement) were done.
2.4. Post-op Day 0
Operation Day, all intra-surgical notes were recorded, and the duration of surgery was calculated from the first dilation of the punctum till the end of the procedure. Post-operative Tobramycin and Dexamethasone eye drops were prescribed for 3 weeks.
2.7. Post-op Day 120
Clinical assessment, including both subjective assessment and measurement of the tear meniscus height.
2.8. Post-op Day 180
Extended follow-up, involving both subjective and objective assessment, showed the same result as in post-operative day 120 with no recurrence of epiphora.
Clinical success was defined as symptom resolution and/or improvement, and with improvement of tear meniscus height.
All data were refined, collected and summarized in tables and graphs. Numerical data were presented as means and standard deviations (M±SD). The difference between numerical variables was checked using an independent t-test. The difference in tear meniscus height pre- and post-surgery was tested using a paired t-test. The categorical variables were presented in frequencies (n) and percentages (%). The association of categorical variables with successful outcomes was tested by applying the Chi-square test or Fischer exact test accordingly. In all statistical analyses, a p-value less than or equal to 5% is considered significant.
3. RESULTS
Twenty-five patients were recruited for this study. Seven (28%) patients were completely relieved from symptoms subjectively within less than 5 days postoperatively, and another 12 (48%) witnessed recovery within a period of 5 days to 9 days. As for the remaining 6 (24%) patients, two of them (8%) patients were symptom-free after 10 days, while 4 (16%) patients had no resolution of symptoms.
Half of the sample was 3 to 6 years of age (56%), males (52%) with left eye involvement (64%), and had no previous probing (44%). The intubation site was in the upper canaliculus for 22 (88%) of cases. Table 1 demonstrates the characteristic features of the sample.
Twenty-one out of the 25 recruited patients showed successful outcomes, giving a total success rate of 84%. Fig. (2) illustrates the distribution of patients according to subjective improvement of symptoms reported through the follow-up period. Only 4 (16%) had unsuccessful outcomes.
There was no significant difference in outcome regarding patients’ age, gender, affected eye, previous probing, site of intubation, and pre-stenting tear meniscus height. As seen in Table 2, no failure outcome occurred among children less than 3 years of age, and only four patients (aged 3, 5, 7 and 11 years) witnessed unsuccessful outcomes (three patients had lost stent, and one patient had nasal deviation). Yet, age showed no significant difference in outcome.
| Characteristic Features | Frequency | Percentage | |
|---|---|---|---|
| Age | <3 | 1 | 4.0 |
| 3-6 | 14 | 56.0 | |
| >6-11 | 10 | 40.0 | |
| Gender | Male | 13 | 52.0 |
| Female | 12 | 48.0 | |
| Laterality | OD | 9 | 36.0 |
| OS | 16 | 64.0 | |
| History of previous probing | No previous trials | 11 | 44.0 |
| One previous trial | 10 | 40.0 | |
| Two trials | 4 | 16.0 | |
| Site of the intubation | Upper Canaliculus | 22 | 88.0 |
| Lower Canaliculus | 3 | 12.0 | |
| Total | 25 | 100.0 | |
| - | (M±SD) | - | |
| Pre-operative tear meniscus height (mm) | 1.87±0.3 | ||
| Duration of surgery (minutes) | 7.40±2.12 | ||
| Post-operative tear meniscus height (mm) | 0.67±0.5 | ||
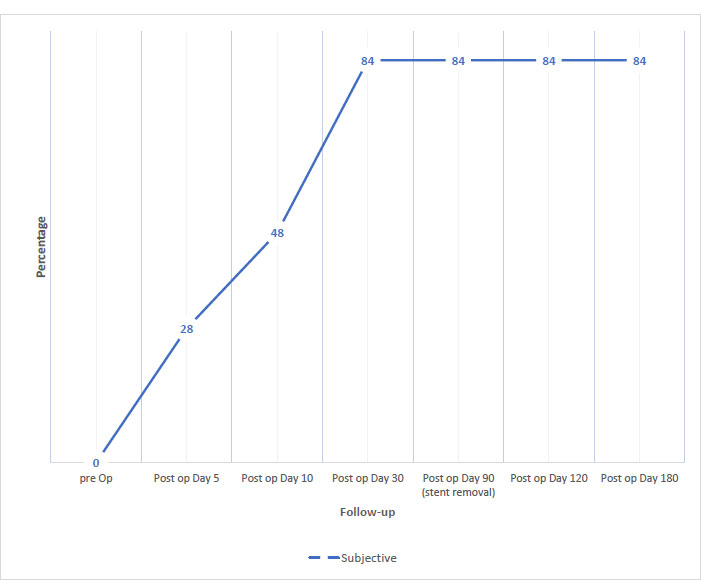 |
Fig. (2). The percentage of patients with subjective improvements reported through the follow-up period. |
| Characteristic Features | Successful Stenting (n=21) | Unsuccessful Stenting (n=4) | P-value | |
|---|---|---|---|---|
| Age | <3 | 1 (100%) | 0 | 0.844* |
| 3-6 | 12(85.7%) | 2 (14.3%) | ||
| >6-11 | 8(80.0%) | 2 (20.0%) | ||
| Gender | Male | 10(76.9%) | 3(23.1%) | 0.593* |
| Female | 11(91.7%) | 1(8.3%) | ||
| Laterality | OD | 8(88.9%) | 1(11.1%) | 0.617* |
| OS | 13(81.3%) | 3(18.8%) | ||
| Previous probing | No previous trials | 8(72.7%) | 3(27.3%) | 0.355* |
| One trial | 9(90.0%) | 1(10.0%) | ||
| Two trials | 4(100.0%) | 0 | ||
| Site of intubation | Upper Canaliculus | 18(81.8%) | 4(18.2%) | 0.420* |
| Lower Canaliculus | 3(100%) | 0 | ||
| Pre-operative tear meniscus height (mm) | 1.84±0.38 | 2.00±0.00 | 0.084§ | |
| Duration of surgery (minutes) | 7.2±2.1 | 8.0±2.4 | 0.615§ | |
| Post-operative tear meniscus height (mm) | 0.48±0.06 | 1.67 ±0.58 | 0.026§ | |
Although 72.7% of pediatric patients with no previous probing had successful outcomes, the percentage increases to 90% and 100% for patients with one trial and two trials of probing, respectively. Yet, no significant association was found.
Although the duration of surgery was shorter among the children in the successful stenting group in comparison with those with unsuccessful outcomes (7.2±2.1 vs. 8.0±2.4) minutes, respectively, the difference was not significant (p-value = 0.615).
In regard to tear meniscus height, preoperatively, both groups were similar; children who had a successful outcome had an average tear meniscus height of 1.8±0.3 mm, and it showed no difference in mean tear meniscus height from those with unsuccessful stenting (2.00±0.00) mm (p-value= 0.084). Table 3 shows the improvement in the tear meniscus height measurement throughout the follow-up period among the studied sample. The study demonstrated a significant difference in post-operative tear meniscus height between the children in the successfully stented cases (21 patients) and those who failed the stenting (4 patients), p-value =0.027, as illustrated in Fig. (3). Patients with successful stenting experienced an improvement in tear meniscus height of about 1.4 mm (from 1.8±0.3 mm to 0.48±0.06 mm) postoperatively, while children with unsuccessful stenting maintained a higher tear meniscus height (the change was only 0.3 mm); their average tear meniscus height changed from 2.00±0.00 mm to 1.67 ±0.58 mm.
| Follow-up End Points | Successful Stenting (n=21) | Unsuccessful Stenting (n=4) |
|---|---|---|
| Pre-operative tear meniscus height (mm) | 1.84±0.38 | 2.00±0.00 |
| Post-operative Day 30 | 0.57±0.06 | 1.98±0.00 |
| Post-operative Day 90 (stent removal) | 0.55±0.05 | 1.95±0.02 |
| Post-operative Day 120 | 0.49±0.04 | 1.70±0.50 |
| Post-operative Day 180 | 0.48±0.06 | 1.67 ±0.58 |
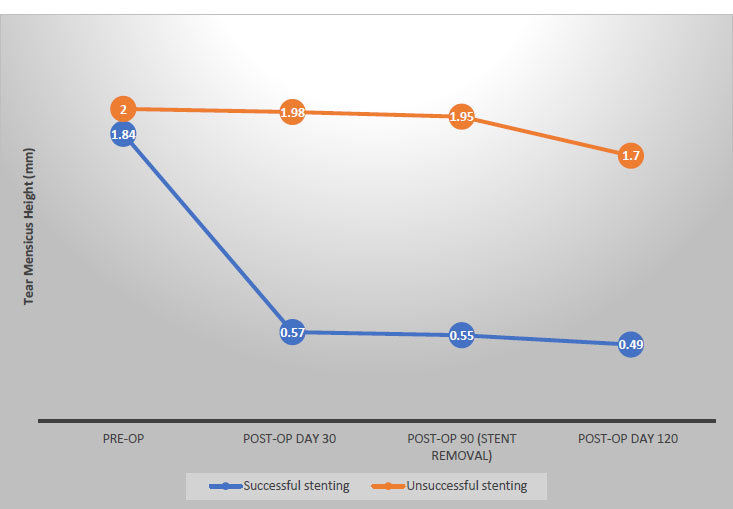 |
Fig. (3). Distribution of patients according to tear meniscus height measurements by days of follow up. |
Finally, we compared the pre and post-operative mean tear meniscus height among all the participants. Table 4 illustrates a highly significant improvement in the measure before and after surgery (P<0.001), indicating a successful procedure.
| Variable | Pre-op | Post-op | P-value |
|---|---|---|---|
| Tear meniscus height | 1.87±0.3 | 0.67±0.5 | 0.000§ |
4. DISCUSSION
Although previous literature agrees on considering intubation after unsuccessful probing, after nasolacrimal duct endoscopy, and after traumatic lacerations [9], intubation is reported to be both more practical and less traumatic. In the current study, twenty-one out of the 25 recruited patients showed successful outcomes, giving a total success rate of 84%. This result is in alignment with findings reported in a study by Eshraghi et al. [10], where the success rate reached 85%. The finding is also comparable to that reported by Pinilla et al. [11] and Fayet et al. [12], where the published success rates were 88.4% and 88.8%, respectively. The current results were also comparable to outcomes described in a study by Wladis et al., where the procedure success rate ranged from 79% to 100% [13].
The current success rate was higher than that reported by Khatib et al. (71%) [14] and Mangan et al. (78.6%) [15]. This difference might be related to the sampling technique and the complexity of cases. The success rate was achieved within a short follow-up period, as 28% of patients were relieved of symptoms within less than 5 days, followed by 48% within 10 days. This finding brought to the benefit of stent removal in office placing, no risk for stent retention, with less jeopardy for corneal inflammation, punctual slitting and iatrogenic harm (compared to bicanalicular stent intubation); this makes Lacrijet (0.64 mm stent diameter) a contemporary technique for nasolacrimal duct intubation in pediatric patients [9, 16].
Four patients had unsuccessful outcomes; the main cause was lost stents. This is in alignment with findings published by Mangan et al., where premature stent loss disrupts the healing of peri-canalicular tissues, resulting in fibrosis and stenosis, which diminishes the surgical success rate [15]. It is also considered as one of the major causes of reoperation. Likewise, the results published by Katowitz et al. showed that early stent loss was significantly associated with a higher risk of surgical failure [17]. The current finding also agrees with the results described in a study by Fayet et al., where 5 cases (17.8%) failed to show successful outcomes [18]. Our present result was lower than the rate reported in research by Mihailovic et al., where 25% of patients had a dislocation or complete loss of intubation [9], and results reported in an article by Wladis et al., where stent extrusions ranged from 0% to 29% [13]. Alternatively, the current unsuccessful outcome rate was higher than the results described in Pinilla et al. study, where technical errors occurred in 11.6% of patients, and it was mainly due to the inability to pass the guide wire through the lacrimal system [11]. Whereas another study by Katowitz et al. showed no failure rate [16]. This variation is probably related to the demographical characteristics of the selected cases.
There was no significant difference in outcome regarding patient age, pre-stenting tear meniscus height, gender, previous probing, or affected eye. This agrees with results reported by Eshraghi et al. [10], Gupta et al., and Sahan et al. [19, 20]. In contrast, the current finding disagrees with Katowitz et al. [17] and Khatib et al. [14], who found a significant difference in outcomes associated with child age. This discrepancy might be related to the difference in the sample sizes and complexity of nasolacrimal obstruction.
The average duration of the surgery was 7.4±2.1 minutes, agreeing with the results described by Hamed Azzam et al. (8.5 minutes) [21]. Meanwhile, Pinilla et al. reported an average of 15 minutes as surgery duration [11]. The alteration is probably related to surgical preparations and the center protocols. Although the duration of surgery was shorter in terms of successful outcomes, no statistically significant difference was obtained. The study showed a highly significant change in tear meniscus height after surgery, which agrees with the results stated in studies by Hamed Azzam et al. [21] and Hoshi et al. [22], where Lacrijet intubation resulted in statistically significant improvements in tear meniscus height, which indicate a successful intervention. This study is the first to follow patients with CLNDO pre- and post-Lacrijet intubation, although one limitation was that it did not compare the cases to a control group. Further studies might probably compare the outcomes of Lacrijet versus probing, which was introduced as the first procedure in the treatment of epiphora. The study chose not to repeat a probing procedure that a significant number of patients had undergone previously. Notably, 14 out of 25 patients (56%) had experienced at least one unsuccessful probing before. The current study found no significant association between a history of previous probing and having a successful Lacrijet intubation outcome.
CONCLUSIONS AND RECOMMENDATIONS
The Mono-canalicular Lacrijet stenting system is simple, safe, and can be administered in an outpatient setting. It is reliable, well-endured, and provides rapid relief of symptoms. The procedure is relatively as safe as probing without presenting additional risks associated with the insertion of bicanalicular lacrimal stenting. These risks include punctual and canalicular trauma (cheese wiring), irritation, foreign body sensation, and potential difficulties in stent placement due to its dual stent nature. The absence of serious complications, coupled with its well-tolerated nature, underscores Lacrijet's safety profile.
Neither age nor previous failed probing affected the success rate. It is recommended that children with epiphora undergo a detailed, careful and early assessment and probably suggested for mono-canalicular stenting. Further studies might compare the outcomes and success rates of probing and intubation as the first procedures among children with epiphora.
LIST OF ABBREVIATION
| CNLDO | = Congenital Nasolacrimal Duct Obstruction |
| M±SD | = Means and Standard Deviations |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Ethics Committee on Human Research in Ibn Al Haitham Teaching Eye Hospital (Approval No. 206 on 4 July 2022).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Additionally, both verbal and signed informed consent forms were obtained from the parents of the patients before they participated in the study. Parents' contact details were documented.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.
REFERENCES
| [1] | Salmon J. Kanski’s clinical ophthalmology. Systematic Approach 9th ed. 2020. |
| [2] | Patel J, Levin A, Patel BC. Epiphora clinical testing. StatPearls 2023. |
| [3] | Avdagic E, Phelps PO. Nasolacrimal duct obstruction as an important cause of epiphora. Dis Mon 2020; 66(10): 101043. |
| [4] | Tai ELM, Kueh YC, Abdullah B. The use of stents in children with nasolacrimal duct obstruction requiring surgical intervention: A systematic review. Int J Environ Res Public Health 2020; 17(3): 1067. |
| [5] | Avram E. Insights in the treatment of congenital nasolacrimal duct obstruction. Rom J Ophthalmol 2017; 61(2): 101-6. |
| [6] | Sooby P, Wynne D. Evaluating the outcomes of children undergoing lacrimal surgery for congenital nasolacrimal duct obstruction with the aim of developing a patient pathway for children presenting to a tertiary paedatric service with epiphora. J Laryngol Otol 2023; 137(7): 815-9. |
| [7] | Ricca A, Kim A, Chahal H, Shriver E. Nasolacrimal stents: An introductory guide. University of Iowa Health care; 2018. 2018. Available from: https://webeye.ophth.uiowa.edu/eyeforum/tutorials/Stents/index.htm (Accessed on: 26th July, 2023). |
| [8] | Park JY, Lee JB, Shin WB, et al. Nasolacrimal stent with shape memory as an advanced alternative to silicone products. Acta Biomater 2020; 101: 273-84. |
| [9] | Mihailovic N, Grenzebach UH, Eter N, Merté RL. Application possibilities of a new preloaded nasolacrimal duct intubation system. Klin Monatsbl Augenheilkd 2021; 238(1): 48-54. |
| [10] | Eshraghi B, Ghadimi H, Karami S, Nikdel M. Outcome of monocanalicular intubation for complex congenital nasolacrimal duct obstruction: The role of age. Rom J Ophthalmol 2022; 66(1): 49-54. |
| [11] | Pinilla I, Prieto FAF, Asencio M, Arbizu A, Peláez N, Frutos R. Nasolacrimal stents for the treatment of epiphora: Technical problems and long-term results. Orbit 2006; 25(2): 75-81. |
| [12] | Fayet B, Racy E, Ruban JM, Katowitz JA, Katowitz WR, Gignac BD. Preloaded monoka (Lacrijet) and congenital nasolacrimal duct obstruction: Initial results. J Fr Ophtalmol 2021; 44(5): 670-9. |
| [13] | Wladis EJ, Aakalu VK, Tao JP, et al. Monocanalicular stents in eyelid lacerations. Ophthalmology 2019; 126(9): 1324-9. |
| [14] | Khatib L, Nazemzadeh M, Revere K, Katowitz WR, Katowitz JA. Use of the masterka for complex nasolacrimal duct obstruction in children. J AAPOS 2017; 21(5): 380-3. |
| [15] | Mangan MS, Turan SG, Ocak SY. Pediatric canalicular laceration repair using the Mini Monoka versus masterka monocanalicular stent. Arq Bras Oftalmol 2023; 86(1): 46-51. |
| [16] | Katowitz WR. Monocanalicular stenting in external dacryocystorhinostomy. J AAPOS 2010; 14(1): e20. |
| [17] | Katowitz WR, Prat DL, Munroe CE, et al. Primary monocanalicular stent intubation for children with congenital nasolacrimal duct obstruction: Surgical outcome and risk factors. Ophthal Plast Reconstr Surg 2022; 38(5): 490-5. |
| [18] | Fayet B, Racy E, Katowitz J, Katowitz W, Ruban JM, Gignac BD. Insertion of a preloaded Monoka™ stent for congenital nasolacrimal obstruction: Intraoperative observations. A preliminary study. J Fr Ophtalmol 2019; 42(3): 248-54. |
| [19] | Gupta N, Neeraj C, Smriti B, Sima D. A comparison of the success rates of endoscopic-assisted probing in the treatment of membranous congenital nasolacrimal duct obstruction between younger and older children and its correlation with the thickness of the membrane at the Valve of Hasner. Orbit 2018; 37(4): 257-61. |
| [20] | Sahan B, Ciftci F. The significance of primary monocanalicular silicone tube intubation in late surgical treatment in children. Eur J Ophthalmol 2022; 32(3): 1464-8. |
| [21] | Azzam HS, Hartstein M, Dolmetsch A, Mukari A. Assessment of Lacrijet monocanalicular intubation for congenital nasolacrimal duct obstruction. Eur J Ophthalmol 2022; 32(6): 3340-5. |
| [22] | Hoshi S, Tasaki K, Hiraoka T, Oshika T. Improvement in contrast sensitivity function after lacrimal passage intubation in eyes with epiphora. J Clin Med 2020; 9(9): 2761. |







