CASE REPORT
Virtual Eye Simulation: An Aid in Evaluation of Capsular Block Syndrome
Joseph L. Hu1, Chao-Chien Hu2, *
Article Information
Identifiers and Pagination:
Year: 2019Volume: 13
First Page: 51
Last Page: 56
Publisher ID: TOOPHTJ-13-51
DOI: 10.2174/1874364101913010051
Article History:
Received Date: 13/02/2019Revision Received Date: 22/03/2019
Acceptance Date: 24/04/2019
Electronic publication date: 31/05/2019
Collection year: 2019

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective:
To demonstrate the findings of three consecutive cases of postoperative Capsular Block Syndrome (CBS) diagnosed with the aid of Pentacam virtual eye simulation images.
Methods:
Observational case series report. Three patients underwent uneventful cataract removal and presented with blurry vision ranging from 4 days to 5 years after the surgeries were performed.
Results:
In a case of early-onset postoperative CBS, virtual eye simulation images clearly revealed a reduced posterior chamber depth caused by the accumulation of transparent fluid in the area between the intraocular lens and the posterior capsule. In two cases of late-onset postoperative CBS, virtual eye simulation images better visualized the alignment between intraocular lens (IOL) and iris than slit lamp examination and Schiemflug images. All three of the cases underwent neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy, and their capsular bag distensions were resolved immediately. The patients with misalignments between IOL and iris experienced more improvement in best-corrected visual acuity as opposed to the one who did not.
Conclusion:
Virtual eye simulation is found to be a useful way in visualizing misalignment between IOL and iris and assisting diagnoses of both early- and late-onset postoperative capsular block syndrome.
1. INTRODUCTION
Capsular Block Syndrome (CBS) is a rare complication of cataract removal that is categorized into three types depending on the time of onset: intraoperative, early postoperative, and late postoperative [1]. Early-onset postoperative CBS is characterized by shallow Anterior Chamber Depth (ACD), capsular bag distension, and postoperative myopic shift in refractive status, while late postoperative CBS is typified by capsular bag distention and the accumulation of a milky-white liquefied substance between the intraocular lens (IOL) and posterior capsule [2]. Possible treatments include neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy or surgical lysis of adhesions [3]. Scheimpflug imaging has shown advantages in detecting changes in the anterior segment and peri-IOL region including the posterior capsule caused by CBS [4, 5]. We present clinical findings of three cases of post operative CBS diagnosed with the aid of Pentacam Scheimpflug imaging and virtual eye simulation.
Three patients underwent uneventful cataract surgery at our hospital. Pentacam Scheimpflug imaging (PentacamAXL ; OCULUS Optikgeräte GmbH, Wetzlar, Germany) were performed before and after Nd:YAG laser posterior capsulotomy. The clinical features of the patients are summarized in Table 1.
| Clinical Features | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Gender | Male | Male | Female |
| Age (years old) | 71 | 67 | 70 |
| Size of CCC (mm) | 5.5 | 5.5 | 5.5 |
| Time of presentation after cataract surgery | 4 days | 4 years | 5 years |
| Intraocular Pressure (mm Hg) | 10 | 16 | 11 |
| BCVA | – | – | – |
| Pretreatmenta | 20/40 | 20/100 | 20/25 |
| Post-treatmenta | 20/25 | 20/25 | 20/25 |
| Refraction (D) | – | – | – |
| Pretreatmenta | -4.0/-4.0 x 85 | +1.0/ -2.0 x 90 | +0.0/ -0.5 x 100 |
| Post-treatmenta | -0.5/-2.25 x 65 | +0.0/ -1.0 x 75 | -0.5/ -0.5 x 95 |
| Posterior distention of capsule (mm)b | Clear fluid about 3 mm thick |
Milky-white fluid about 1 mm thick |
Milky-white fluid about 1 mm thick |
| ACD (mm) | – | – | – |
| Pretreatmenta | 1.99 | 3.94 | 4.71 |
| Post-treatmenta | 3.14 | 4.08 | 4.40 |
| Changes in ACD (mm) | +1.15 | +0.14 | -0.31 |
| Previous surgery | Macula pucker, s/p PPV OD a year before | PDR with Vitreous hemorrhage, s/p PPV OS 5 years before | None |
| Intraocular Lens | – | – | – |
| Axial length (mm) | 24.37 | 23.23 | 22.83 |
| Power | 21.5 D | 23.5 D | 20.0 D |
| Material | hydrophilic acrylic lens | hydrophilic acrylic lens | hydrophilic acrylic lens |
aUCVA, BCVA, refraction, and ACD changes of capsular block syndrome cases before and after Nd:YAG laser capsulotomy.
bData detected by Pentacam Scheimpflug imaging before Nd:YAG laser capsulotomy. Approximated by measuring the relative thickness of the posterior distension to anterior chamber depth.
2. CASE REPORTS
2.1. Case 1
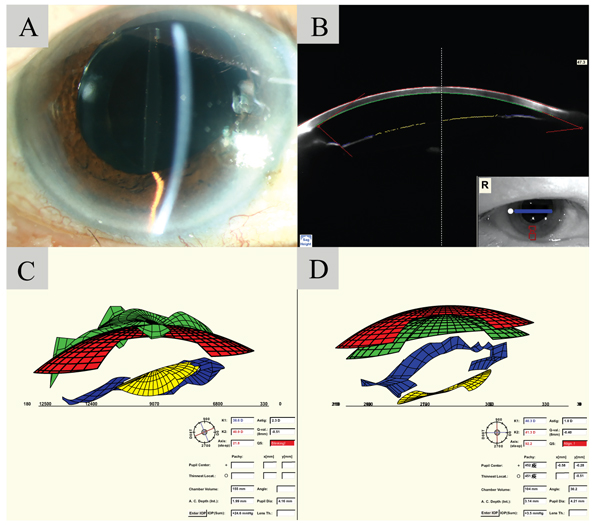
A 71-year-old man presented with blurry vision in his right eye 4 days after he had undergone phacoemulsification with IOL (Rayner 970C) implantation in his right eye. His best-corrected visual acuity at presentation was 20/40. There was an increase in myopia after cataract surgery within 4 days ranging from −0.50 diopters (D) to −4.00 D. At presentation, virtual eye simulation presented by Pentacam examinations better visualized a reduced depth of posterior chamber (depth between iris and IOL) than slit lamp examination and Scheimpflug images (Fig. 1). Slit lamp examination and Pentacam images also indicated a reduced anterior chamber depth. Fluid between IOL and posterior capsule was so transparent that it could barely be seen with slit lamp or Pentacam scheimpflug images, although a distended posterior capsule was visualized by fine-tuning the focus of the slit lamp. After Nd:YAG laser capsulotomy was performed, capsular bag distension and the myopic shift were both resolved, and the IOL returned to a parallel position with the iris with normal posterior chamber depth.
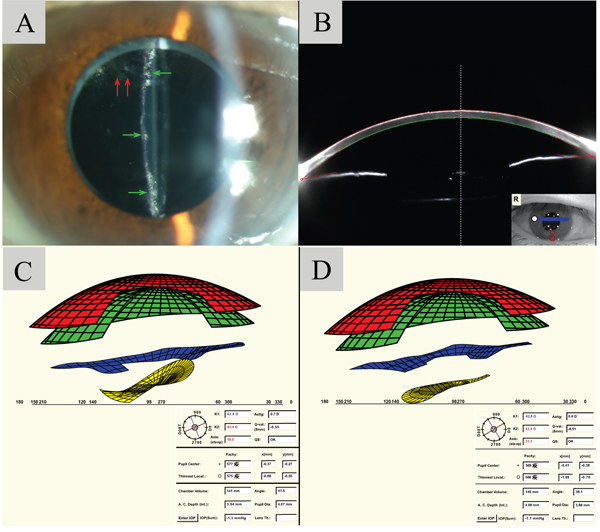
2.2. Case 2
A 67-year-old man presented with blurry vision in his left eye lasting 2 months. He had undergone phacoemulsification with IOL (Rayner 570C) implantation in his left eye 4 years earlier. His best-corrected visual acuity had deteriorated from 20/33 to 20/100 in the past 2 months. Slit lamp examination revealed opacification of the posterior capsule, distention of the capsular bag, and accumulation of milky-white liquid in the post IOL region. Proliferating lens epithelial cells was also observed superiorly within the pupillary zone (Fig. 2A). Scheimpflug imaging visualized mild accumulation of fluid in the peri-IOL region and parts of the IOL, yet failed to visualize its complete contour (Fig. 2B). Virtual eye simulation, giving a better visualization of the IOL, demonstrated misalignment between IOL and iris (Fig. 2C). After Nd:YAG laser capsulotomy was performed, capsular bag distension was successfully resolved, and the IOL returned to a parallel position with the iris (Fig. 2D).
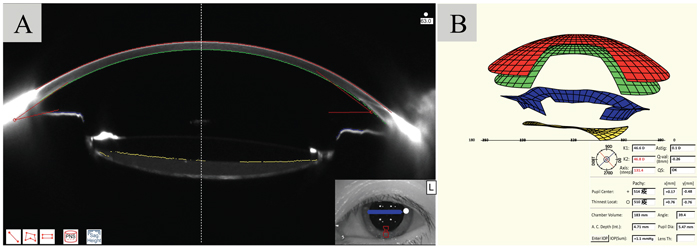
2.3. Case 3
A 70-year-old woman presented with blurry vision in the left eye lasting 1 year. She had undergone phacoemulsification with IOL (Rayner 970C) implantation in the left eye 5 years earlier. Her best-corrected visual acuity during the early postoperative stages was 20/20. At presentation, slit lamp examination and Scheimpflug images demonstrated accumulation of milky-white fluid, and capsular block syndrome in the left eye was diagnosed (Fig. 3A). However, the virtual eye simulation presented by Pentacam reveals no misalignment between the IOL and the iris (Fig. 3B). After Nd:YAG laser capsulotomy was performed, capsular bag distension was resolved.
3. DISCUSSION
Capsular block syndrome is categorized into three types depending on the time of onset: intraoperative, early postoperative, and late postoperative [1]. This report includes three cases of postoperative CBS: Case 1 being early postoperative CBS and Case 2 and 3 being late postoperative CBS. All of the three cases had their cataract removed by Continuous Curvilinear Capsulorhexis (CCC) without the aid of femtosecond laser. A reduction in myopia in accordance with previous reports is observed immediately after Nd:YAG laser capsulotomy was performed on case 1 [6]. In the first two cases, the IOL in both patients returned to a parallel position with the iris with normal posterior chamber depth after Nd:YAG was performed and resulted in improved vision. While in case 3, the changes in the position of IOL was inconspicuous, and the vision improvement was also not evident. The IOL position changes after Nd:YAG can be easily visualized by the virtual eye simulation images (Figs. 1, 2).
Early postoperative CBS is characterized by shallow ACD, capsular bag distension, and postoperative myopic shift in refractive status [3]. Early postoperative CBS may occur when residual OVD becomes trapped within the capsular bag between the posterior capsule and the posterior surface of the IOL, and the liquid accumulated in capsular bags is viscoelastic device, which is transparent [7]. Since milky-white fluid is usually absent in early postoperative CBS, diagnosis largely relies on observing shallowed anterior chamber and distended capsular bag during slit-lamp examination. As opposed to late postoperative CBS, early postoperative CBS usually lacks accumulation of milky white fluid behind the IOL, thus Scheimpflug images offer limited assistance in its diagnosis (Fig. 1). In the virtual eye simulation image in case 1, however, the positioning between patient’s iris and IOL is visualized in a 3D-fashion, and the distance between the iris and IOL is clearly-noted (Fig. 1). Such reduced posterior chamber depth indicates unidentified pressure behind the IOL from capsular bag distension. With the aid of virtual eye simulation, early postoperative CBS cases that were hard to visualize could now be easily detected by slit lamp examinations and virtual eye simulation images combined.
In regard to case 1, one must note the resemblance of presentations between early postoperative CBS and aqueous misdirection when viewing the virtual eye simulation in Fig. (1). Aqueous misdirection is a condition described as a ciliolenticular block induced by anterior movement of the lens-iris diaphragm, poor vitreous fluid conductivity, and choroidal expansion [8]. It most commonly occurs after intraocular surgery in eyes with prior angle-closure glaucoma. The disease presents with a shallowing of the anterior chamber in both central and peripheral portions and leads to a secondary elevation of IOP as a consequence of angle obstruction. In case 1, a distended posterior capsule was observed by slit lamp examination, thus indicating an accumulation of fluid within the capsular bag. The low preoperative IOP (IOP=10 mmHg) also contradicts the secondary elevation of IOP that usually presents in aqueous misdirection. In addition, the capsular bag distension, myopic shift, and the misalignment between IOL and iris all resolved once Nd:YAG laser was performed. These presentations collectively indicate the diagnosis of early postoperative CBS instead of aqueous misdirection in case 1. After all, when utilizing virtual eye simulation, it is crucial to perform comprehensive slit lamp examination and review patient history to differentiate between early postoperative CBS and aqueous misdirection.
In late postoperative CBS, the margin of the CCC is blocked by the IOL optic, and this produces a closed chamber inside the capsular bag in which the turbid fluid accumulates [9]. Additionally, residual lens epithelial cells and posterior capsule opacification were also noted in previous reports [10]. Diagnosis of late-onset postoperative CBS depends on the identifying of milky-white fluids with slit lamp examination and Scheimpflug images [4]. When the liquefied substance is difficult to identify as shown in case 2, misalignment of iris and IOL shown in virtual eye simulation implies unevenly distributed pressure behind IOL and assists the diagnosis (Fig. 2). However, note that even when IOL aligns with iris in a parallel position, fluid accumulation could still be present (Fig. 3). When suspecting late postoperative CBS, we suggest that ophthalmologists take all slit lamp examination, Scheimpflug images and virtual eye simulation images into consideration before making final diagnoses when these data are available.
Given the different pathogenesis in early and late postoperative CBS, the main complaints of patients in early postoperative CBS are usually the blurred vision induced by the anterior movement of IOL and myopic shift, while that in late postoperative CBS patients are usually the reduced quality of vision caused by the accumulation of turbid fluid behind the IOL. By analyzing the Pentacam virtual eye simulation of all three patients, we suggest that positioning of IOL also plays an important role on whether patients with capsular block syndrome are to experience an improvement in best-corrected visual acuity after receiving Nd:YAG laser. In case 1 and 2, the IOLs of the patients were either misaligned or abnormally close to their irides preoperatively, and both patients experienced a significant improvement in best-corrected visual acuity (Case 1: 20/40 to 20/25; Case 2: 20/100 to 20/25) immediately after Nd:YAG laser was performed. While in case 3, postoperative changes of IOL positioning was absent, and the best-corrected visual acuity of case 3 remains the same after laser was performed (Case 3: 20/25). However, while the visual acuity improvement could be mild in cases resembling case 3, it is still possible that patients experience visual quality improvement due to the clearance of the turbid fluid. Larger studies are required to identify the relationship between IOL positioning changes and best-corrected visual acuity improvements in patients with capsular block syndrome undergoing Nd:YAG laser treatments.
Early CBS is commonly characterized by prominent shallowing of ACD, while the ACD changes in late CBS still remains controversial [11]. In our cases, the ACD in case 1, which is diagnosed with early CBS, increased from 1.99 mm to 3.14 mm after Nd:YAG was performed. The ACD changes in late CBS cases after Nd:YAG were performed, on the other hand, were relatively milder and the statistics may not be statistically significant. (case 2: 3.94mm→4.08mm; case 3: 4.71mm→4.40mm) Studies with larger numbers of patients with late CBS are still required to identify the changes of ACD in late CBS.
In spite of the potential benefits virtual eye simulation has on assisting the diagnosis of capsular block syndrome and predicting visual acuity improvements, it does not come without its limitations. While the virtual eye simulation shows the narrowing of the posterior chamber and the space between IOL and iris, it barely provides any information in the space between IOL and posterior capsule. Also, in cases resembling case 1, ophthalmologists must differentiate capsular block syndrome with aqueous misdirection by slit lamp examination. Therefore, while the tool shows potential in being an aid in evaluating capsular block syndrome, the diagnosis should not be made merely on its findings.
CONCLUSION
In conclusion, Pentacam virtual eye simulation showed potential for being a noninvasive technique for assisting diagnosis and follow-up in both early and late postoperative CBS cases.
LIST OF ABBREVIATIONS
| CBS | = Capsular Block Syndrome |
| ACD | = Anterior Chamber Depth |
| IOL | = Intraocular Lens |
| BCVA | = Best Corrected Visual Acuity |
| CCC | = Continuous Curvilinear Capsulorhexis |
| PPV | = Pars Plana Vitrectomy |
| PDR | = Proliterative Diabetic Retinopathy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by internal ethics committee at Shin Kong Wu Ho-Su Memorial Hospital, Taipei, Taiwan.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
A written informed consent was obtained from all patients when they were enrolled.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analyzed during the current study are available from the corresponding author.
STANDARDS OF REPORTING
This article was written in accordance with CARE guideline.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.