RESEARCH ARTICLE
Evaluation of the Anterior Chamber Parameters by Pentacam after Toric Implantable Phakic Contact lens (IPCL) Implantation in Moderate to High Myopia with Astigmatism
Mohamed Salah El-Din Mahmoud1, *, Mohamed Abdel Hamid1, Mohamed Esmail Khalil Esmail1, Ahmed Abdel Halim1
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187436412208200
Publisher ID: e187436412208200
DOI: 10.2174/18743641-v16-e2208200
Article History:
Received Date: 15/2/2022Revision Received Date: 27/4/2022
Acceptance Date: 15/5/2022
Electronic publication date: 31/10/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
The toric IPCL is posterior phakic intraocular lens used for correction of moderate to high myopia with astigmatism, but after the implantation, there were changes in the parameters of the anterior chamber (AC).
Purpose:
The purpose of this study is to assess the parameters of the AC and lens vault after toric IPCL in patients with moderate to high myopia with astigmatism by Pentacam.
Patients and Methods:
In a prospective interventional case series, 30 eyes with moderate to high myopia with astigmatism were treated with toric IPCL implantation. Pentacam was done preoperatively, after 1 month, 3 months and 6 months of toric IPCL implantation for evaluation of the AC parameters as the angle of the anterior chamber (ACA), depth of the anterior chamber (ACD) and volume of the anterior chamber (ACV). Also, the lens vault and intraocular pressure (IOP) were evaluated.
Results:
The ACD was 3.3±0.1 mm preoperatively and changed to 2.5±0.1 mm after 1 month and remained stable at 3 and 6 months postoperatively (p-value =0.001). The ACV was 198.06±25.02 mm3 preoperatively and reduced to 131.5±20.7, 131.8±21.4 and 131.5±20.2 mm3 after 1 month, 3 months and 6 months, respectively(p-value =0.001). The ACA was 42.9±4.1 preoperatively and changed to 26.7±4.3, 26.4±4.2 and 26.7±4.9 after 1 month, 3 months and 6 months, respectively (p-value =0.001). The vault was 458±126.2 um after 1 month, 461±129.6 um after 3 months and 464.6±130.6 um after 6 months (p-value =0.005). The IOP was slightly high during the first month, then reduced to a level near the preoperative values during the second and third follow-up.
Conclusion:
The Pentacam was a useful tool for follow up of the AC parameters after toric IPCL implantation in patients with moderate to high myopia astigmatism.
1. INTRODUCTION
The phakic posterior chamber intraocular lenses (PIOLs) have many advantages over corneal refractive surgery as being suitable for a moderate and high degrees of errors of refraction with better contrast sensitivity [1, 2]. PIOLs also have a unique advantage over other treatment modalities such as clear lens extraction and accommodation preservation. PIOLs have some complications as any intraocular surgery as potential damage to anterior segment structures, secondary glaucoma, cataract and endophthalmitis [3].
Several types of anterior chamber IOLs as the angle-supported anterior chamber IOLs which are less used nowadays because of their higher incidence of complications such as corneal decompensation, cataract, glaucoma, and abnormal pupil configuration. In contrast, iris fixated and posterior chamber (PC) IOL have better efficacy and safety profile, with stable outcomes [4].
The IPCL V2.0 TORIC (Caregroup, India) is a hydrophilic acrylic copolymer single-piece PIOL. It can be injected through a 2.8 mm incision. It has a wide range of power from +15.0 to −30.0 D with astigmatic correction up to 10.0 D. It has six haptics. It has a central opening of about 380 μm designed to decrease light scattering and glare and to facilitate aqueous humor circulation to eliminate the need for peripheral iridectomy. The optical zone diameter ranges from 5.75 to 6.20 mm, with an overall diameter of 11.0–14.00 mm (with a 0.25 mm steps). The toric design could be customized according to the size and shape of each eye. The Visian implantable collamer lens (ICL – Staar Surgical AG, Nidau, Switzerland) is considered a safe and efficient method for the correction of moderate and high myopia, but the IPCL has an advantage over the ICL is that it is more economical, especially in our country [4-7].
The Pentacam (OCULUS Optikgerate GmbH, Wetzlar, Germany) is a Scheimpflug tomography device which is the most popular instrument used in refractive surgery providing data about anterior and posterior corneal surfaces, corneal thickness and anterior chamber parameters [8].
Our study evaluated the parameters of the AC, IOP, and lens vault after toric IPCL in patients with moderate to high myopia with astigmatism by Pentacam.
2. MATERIALS AND METHODS
2.1. Study Design
A prospective interventional case series. We analyzed the results of the toric IPCL implantation in 30 eyes of patients with moderate to high myopia with stigmatism at the Minia University Hospital and International eye centre, Minia, Egypt, from January 2020 to September 2021. The study was approved by the Minia University Faculty of Medicine Research Ethical Committee (FMREC) with approval number 230-2022. Our research adhered to the tenets of the Declaration of Helsinki. A written informed consent was taken from all study subjects for both the surgical intervention and inclusion in the study after a thorough explanation of the nature of the study and all possible risks and benefits of surgery. The study included patients with age more than 18 years, myopia more than -8 D with astigmatism up to -10 D. Minimal depth of the anterior chamber (ACD) was 3.00 mm not including the pachymetry by Pentacam, normal IOP and normal endothelial cell count by specular microscopy (Tomey EM-3000, Tomey Co, Japan). The study excluded patients with shallow ACD less than 3 mm, a history of ocular trauma or surgery, cataract, optic nerve disorders, glaucoma, diabetes mellitus and young patients less than 18 years
2.2. Toric IPCL Power Calculation
Manifest and cycloplegic refraction, ACD, keratometric measurements, pachymetry which were measured by Pentacam and white-to-white (WTW) using a Castroviejo caliper (Ambler Surgical, Germany) were the data needed for the toric IPCL measurement which was calculated using the software PICL Power choice of Care group Surgical.
2.3. Surgical Procedure
All Toric IPCL implantation surgeries were performed using V2.0 design under general anesthesia by the same surgeon. Tropicamide 1% (Alcon Lab, Inc, Fort Worth, TX) was installed every 10 minutes for a minimum of 30 minutes for adequate pupil dilation. To avoid cyclotorsion, the zero horizontal axis was detected at slit lamp in the upright position. 2.8 mm clear temporal corneal incision was made, and the anterior chamber was partially filled with viscoelastic. The IPCL was slowly injected into the AC for detection of the orientation. Gentle pressure was done on the four footplates to place them under the iris plane. Toric lens is always placed on the horizontal axis between 0 and 180 degrees, so rotation was not needed. Irrigation aspiration of the viscoelastic was done and hydration of the wound was performed.
Postoperative treatment included topical antibiotics such as moxifloxacin 0.5% and topical steroids with antibiotic as dexamethasone 0.1% and tobramycin 0.3% for 2 weeks and tapered gradually with follow-up was after 1 day, 3 days, 1 week and 2 weeks,1 month, 3 months and 6 months after the surgery with evaluation of the uncorrected distance visual distance acuity (UCVA), best corrected distance visual acuity (BCDVA), postoperative refraction, IOP and slit lamp to evaluate the IPCL position, iris configuration and clarity of the crystalline lens.
Pentacam was done preoperatively and 1, 3 and 6 months after toric IPCL implantation by the same observer with detection of the following parameters:
- -ACA and ACV were automatically measured by the device’s software.
- -The postoperative anterior chamber depth (ACD) was defined as the distance between the central posterior corneal endothelium and the anterior implantable phakic contact lens (IPCL) surface.
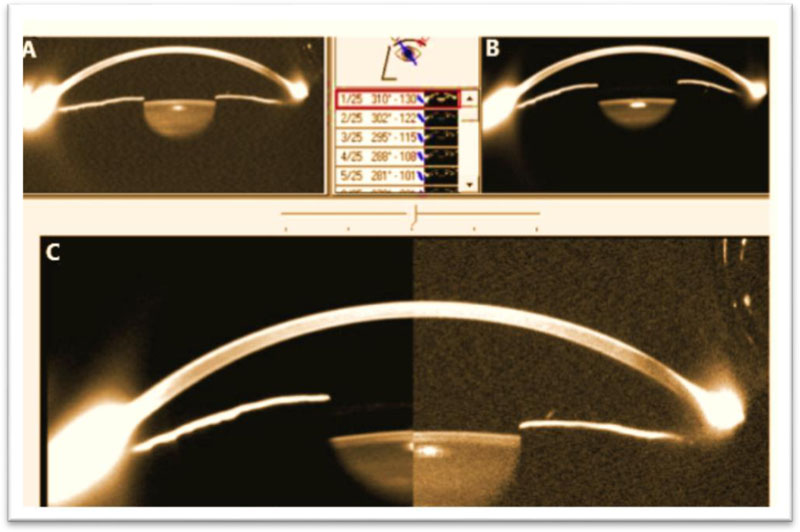
- -The vault was measured as the central distance between the posterior IPCL surface and the anterior crystalline lens capsule. (Fig. 1).
2.4. Statistical Analysis
Data was revised for its completeness and consistency. The SPSS (Statistical Package for Social Sciences) software for Windows, Version 25 (IBM Corp., Armonk, NY, USA) was used for data entry. One-way variance analysis (ANOVA) was used for the analysis of the time course of changes, the Dunnett test was used for multiple comparisons and the Wilcoxon signed-rank test was used to compare the pre- and post-surgical data. A value of p<0.05 was considered statistically significant.
3. RESULTS
3.1. Demographic Data
This study included 30 eyes of 30 patients, 16 females (53.3%) and 14 males (46.7%). Mean age was 27.9±4.7 (range, 20–34) years. All patients had unilateral surgery (20 right eye and 10 left eye) (Table 1).
Table 1. Age and sex of the studied cases.
| Total N= 30 | ||
|---|---|---|
| Age | Range Mean ±SD |
20-34 27.9±4.7 |
| Sex | Male Female |
14(46.7%) 16 (53.3%) |
3.2. Refractive Outcome
Regarding the spherical error, it was -13.4±2.4 preoperatively and corrected to -0.83±0.2 after 1 month then -0.56±0.1 after 3 months and remained stable after 6 months. Regarding the cylindrical error, it was-3.8±0.5 preoperatively and corrected to-0.87±0.4 after 1 month, then -0.80±0.1 after 3 months and -0.73±0.17 after 6 months. The UCDVA was 1.03±0.03 preoperatively, which improved to 0.35±0.05 after 1 month and remained stable up to 6 months. The BCDVA was0.35±0.11 and improved significantly up to 6 months postoperatively (Table 2).
Table 2. Refractive outcome.
| P-value | After 6 months | After 3 months | After 1 month | Preoperatively | |
|---|---|---|---|---|---|
| 0.001* | -0.56±0.15 | -0.56±0.1 | -0.83±0.2 | -13.4±2.4 | Sphere |
| 0.001* | -0.73±0.17 | -0.80±0.1 | 0.87±0.4- | -3.8±0.5 | Cylinder |
| 0.001* | 0.28±0.03 | 0.3±0.01 | 0.35±0.05 | 1.03±0.03 | UCDVA (Log Mar) |
| 0.001* | 0.25±0.05 | 0.24±0.05 | 0.27±0.07 | 0.35±0.11 | BCDVA (Log Mar) |
3.3. The AC Parameters
The ACD was 3.3±0.1 mm preoperatively and changed to 2.5±0.1 mm after 1 month and remained stable at 3 and 6 months postoperatively. The ACV was 198.06±25.02 mm3 preoperatively and reduced to 131.5±20.7, 131.8±21.4 and 131.5±20.2 mm3 after 1 month, 3 months and 6 months, respectively. The ACA was 42.9±4.1 preoperatively and changed to 26.7±4.3, 26.4±4.2 and 26.7±4.9 after 1 month, 3 months and 6 months, respectively. The vault was 458±126.2 um after 1 month, 461±129.6 um after 3 months and 464.6±130.6 um after 6 months (Table 3). Fig. (1) shows the changes in the AC in Scheimpflug images.
The IOP was slightly high during the first month (17.9±1.6 mmHg) and then reduced to a level near the preoperative value in the second and third follow-up visits.
Table 3. Anterior chamber parameters measurement by Pentacam.
| P-value | After 6 months | After 3 months | After 1 month | Preoperatively | |
|---|---|---|---|---|---|
| 0.001* | 2.5±0.1 | 2.5±0.1 | 2.5±0.1 | 3.3±0.1 | AC depth (mm) |
| 0.001* | 131.5±20.2 | 131.8±21.4 | 131.5±20.7 | 198.06±25.02 | AC volume (mm3) |
| 0.001* | 26.7±4.9 | 26.4±4.2 | 26.7±4.3 | 42.9±4.1 | Angle |
| 0.005* | 464.6±130.6 | 461±129.6 | 458±126.2 | VAULT (um) |
Table 4. IOP.
| P-value | After 6 months | After 3 months | After 1 month | Preoperative | |
|---|---|---|---|---|---|
| 0.001* | 14.5±1.2 | 14.7±1.7 | 17.9±1.6 | 13.4±1.7 | IOP(mm Hg) |
4. DISCUSSION
The toric IPCL is used for correction of moderate to high myopia with astigmatism up to -10 D. The initial design V1 has no central hole with a need for peripheral iridectomy (PI) while the new design V2.0 has 380 micrometer central hole, which has several advantages as no need of PI, reduced risk of pigment dispersion, easy removal of viscoelastic, low risk of pupillary block glaucoma, low risk of cataract formation due to the continuous aqueous current between anterior capsule of lens and posterior surface of IPCL [9].
The most common complications after phakic IOLs (pIOL) are cataract and an increase in IOP [10]. Pentacam, ultrasound biomicroscopy (UBM) and anterior segment optical coherence tomography (AS-OCT) were used for the assessment of the anterior segment parameters after pIOL [11]. In our study, toric IPCL V 2.0 was used with no need for peripheral iridectomy and Pentacam was used to evaluate ACA, ACV, ACD and vault 1, 3 and 6 months after surgery as compared to the preoperative parameters. Also, the IOP was monitored.
ACA was decreased significantly from 42.9±4.1 preoperatively to 26.7±4.3 at 1 month postoperatively and remained stable for 6 months postoperatively, the reduction in ACA mostly due to the convex design of the IPCL. The results agreed on similar results studying toric phakic intraocular lenses as toric implantable collamer lens (ICL) as Fernández-Vigo et al who used AS-OCT for detection of the iridocorneal angle [12].
The ACD was measured from the back surface of the cornea to the anterior surface of the IPCL. The ACD was 3.3±0.1 mm preoperatively which decreased significantly to 2.5±0.1mm after one month postoperatively and remained stable after 3 and 6 months postoperatively. These results agreed with results of Ju et al which found that mean preoperative ACD measured with AS-OCT was 3.28 ± 0.14 mm and 2.45 ± 0.22 mm 3 months postoperatively [13].
The AC volume decreased significantly to one month postoperatively when compared to preoperative value and remains stable after 3 and 6 months postoperatively.
The vault was measured as the central distance between the posterior surface of the IPCL and the crystalline lens anterior surface. Low values of the vault increase the incidence of cataract formation due to the increased possibility of crystalline lens touch. On the other side, high values of the vault lead to shallow anterior chamber with an increased possibility of angle closure glaucoma. A value between 250 to 750 um was considered as a safe vault. A vault greater than 150 um was able to avoid the contact of the crystalline lens on a study done on V4 ICL [14]. Our results showed stable lens vault during the follow-up period with no cases of low or high vault reported.
On measuring the IOP, it was high in the first month in some cases, mostly due to retained viscoelastic substance which was managed by topical antiglaucoma medications and then decreased during the second and third follow up. Some cases had a mild rise in IOP during the follow up period, possibly due to topical steroid use, which returned to normal values after steroid stopping. This was in agreement with Almalki et al who found elevated IOP in 10.8% of cases [15].
Other studies on posterior chamber phakic IOL as ICL using AS-OCT, Pentacam and UBM as Zhang et al reported that AS-OCT gave significantly higher vault measurement than UBM in eyes after ICL implantation [16]. Wang et al reported that Pentacam had smaller values for vault measurements than UBM [17].
The safety of the IPCL was evaluated by other studies as Elkareem AM et al who implanted the IPCL V2 in 46 eyes of 32 patients with a high degree of myopia and followed up to 12 months. The mean spherical equivalent at baseline was −13.8±4.1 D and improved to −0.6±0.7 D at 12 months postoperatively (P<0.003) [4].
Sachdev GS et al. compared the clinical outcomes following implantation of the ICL and IPCL and demonstrated similar efficacy and safety profile in both types, but the IPCL is an effective and economically viable option for the correction of myopia [18].
A study was conducted by Rateb M et al on 60 eyes of 60 patients (28 in the ICL group and 32 in the IPCL group) with a follow-up period of 12 months and concluded that both ICL and IPCL are effective methods to correct high myopia in adults with no statistically significant differences between the two lenses as regarding adverse effects [19].
CONCLUSION
Our study concluded that toric IPCL was a safe lens for correction of moderate to high myopia with astigmatism with significant changes in the AC parameters (ACD,ACV, and angle) following the implantation with the stability of these parameters and IOP during the follow-up period. Also, Pentacam was a reliable method for evaluation of the anterior segment after toric IPCL implantation.
LIST OF ABBREVIATIONS
| AC | = Anterior Chamber |
| IOP | = Intraocular Pressure |
LIMITATIONS
Our study has some limitations as the number of subjects was relatively small, the follow up period was short and lack of measurement by other imaging modalities such as UBM and AS-OCT.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the Minia University Faculty of Medicine Research Ethical Committee (FMREC) with approval number 230-2022.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
A written informed consent was taken from all study subjects for both surgical intervention.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data sets used and/or analysed during this study are available from the corresponding author upon request.
FUNDING
None.
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.