CASE REPORT
Workplace Trauma with Massive Intraorbital Foreign Body, A Dramatic Outcome
Hala M. Nassim1, Mohammed H. Alam2, *, Saleh M. Alshuraim2, Abdullah A. Alfrayyan2
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187436412209290
Publisher ID: e187436412209290
DOI: 10.2174/18743641-v16-e2209290
Article History:
Received Date: 13/5/2022Revision Received Date: 4/8/2022
Acceptance Date: 30/8/2022
Electronic publication date: 03/11/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Intra-orbital foreign bodies [IOFB] are considered a rare condition, and an enormous challenge to surgeons, as it might be difficult to diagnose in some cases even with the current advances in imaging technology. Retained IOFB can be a cause of major visual morbidity and blindness, especially in the working population.
Purpose:
In this article, we report a case of IOFB that occurred as a result of workplace related trauma while drilling ceramic.
Methods:
Case report and literature review using PubMed.
Case Presentation:
we present a case of a 30 years old male, not known to have any medical illness, the patient presented to the emergency department after getting trauma while drilling ceramic. Orbital computed tomography [CT] showed multiple high-density objects situated in a circumferential pattern around the globe.
Results:
The patient underwent lateral canthotomy and cantholysis in the emergency department, followed by three exploratory operations to remove intraorbital foreign bodies [FBs] . Luckily, the patient in our case regained a 0.5 visual acuity, with an impressive improvement in the extraocular muscle motility, with only mild restriction in the upper and lower gazes. The patient was followed up for 2 years after the incident, he was stable during that period.
Conclusions:
IOFB is an ophthalmological emergency, careful history, examination, and investigations are important steps in diagnosing IOFB since it can be easily missed when depending solely on imaging. Timely management is crucial to prevent irreversible complications.
1. INTRODUCTION
Intra-orbital foreign body [IOFB] is defined as an object, located completely or partially within the orbital wall. It is further classified upon the location into intraconal or extraconal [1-3].
IOFB is considered a rare condition, and an enormous challenge to surgeons, as it might be difficult to diagnose in some cases even with the current advances in imaging technology. Management of IOFB depends on the location, extension, and foreign bodies (FBs) material; thus, management of such cases must be tailored individually [4, 5].
Identifying the material of FBs, possess a valuable role in the management plan, it can be classified into metallic and non-metallic, non-metallic objects are further classified into organic and inorganic [3].
In this article, we report a case of IOFB that occurred as a result of workplace-related trauma while cutting ceramic.
2. CASE PRESENTATION
2.1. Patient Information and Clinical Findings
We present a case of 30 years old male, not known to have any medical illness, the patient presented to the emergency department after getting trauma while drilling ceramic.
Patient was complaining of severe pain, associated with ptosis, chemosis, proptosis and ophthalmoplegia of the left eye.
On examination, externally, the left eye was proptotic with significant chemosis (Fig. 1).
Visual acuity 1.0 in the right eye and counting fingers in the left eye, the pupil was regular, round, mid dilated and non-reactive. Extraocular muscles were severely restricted in all directions (Fig. 1).
Cornea was intact, no abrasion noted with fluorescein, marked conjunctival injection and congestion. Anterior chamber was deep and quiet, with a clear lens.
Right eye examination was within normal.
2.2. Diagnostic Assessment
Fundus photograph showed a massive scleral indentation near the macula (Fig. 2) which was also noted in the b-scan ultrasound in addition to high density objects posteriorly (Fig. 2b).
 |
Fig. (1). The left eye was proptotic with significant chemosis. |
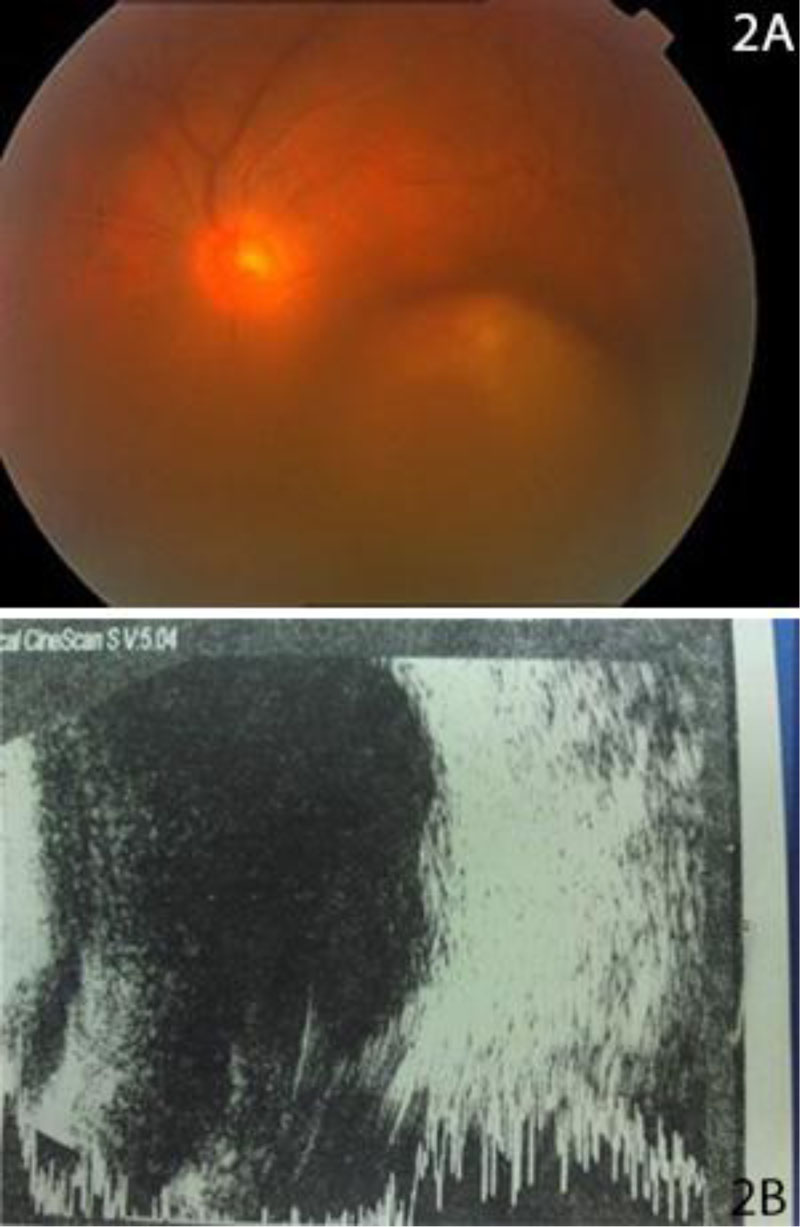 |
Fig. (2). A: Fundus photograph B: : B-scan ultrasound. |
 |
Fig. (3). Shows orbital computed tomography [CT]. |
Orbital computed tomography [CT] was done, showing proptotic left eye globe, multiple high-density objects situated in a circumferential pattern around the globe, extending from the superior rectus supra-laterally, to the lateral rectus, inferior rectus and just inferior to the medial rectus. It was extending from the equator in the extraconal space, until near the apex of the orbit posteriorly. Causing severe mass effect and inward displacement of the lateral rectus muscle. The globe was intact. Minimal displacement of left optic nerve. Right eye within normal (Fig. 3).
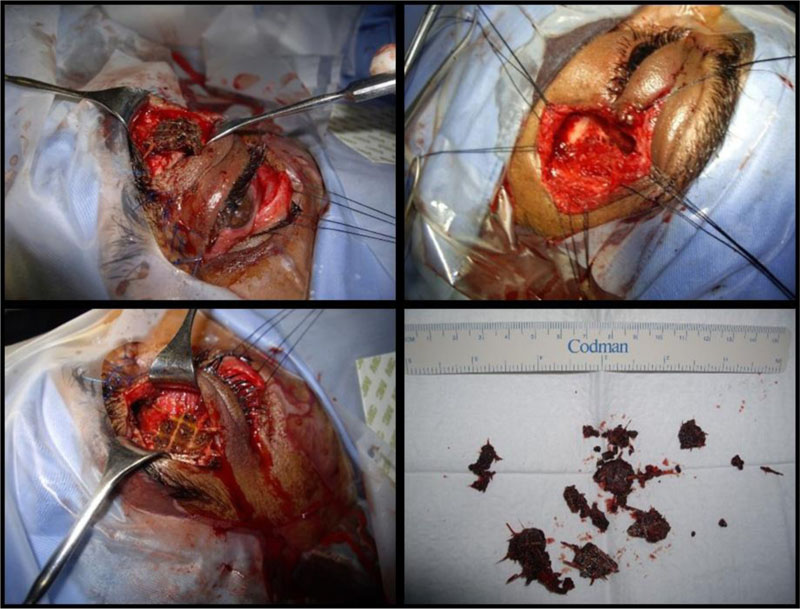 |
Fig. (4). Intraoperative pictures and the removed foreign bodies. |
2.3. Therapeutic Interventions
The patient underwent three operations, with a 2-week interval between each. Management of eye compartment syndrome was done in the emergency department; it was achieved by performing lateral canthotomy and cantholysis. Afterwards, the patient underwent his first operation, two exploratory incisions were done to remove FBs; superior crease incision and a subconjunctival incision in the inferior fornix, which resulted in the removal of multiple FBs (Fig. 4). The FBs appeared as ceramic and wood; the wood part was laid out in sheets that are attached below the ceramic blocks to prevent friction.
Post-operative CT reported that the FBs displacing the lateral rectus were removed, and the muscle was intact. Residual FBs were seen on the floor of the left orbit. Intact optic nerve (Fig. 5).
The purpose of the second operation was to further explore the orbit, which was done by a conjunctival incision, and more particles of the FBs were removed (Fig. 6).
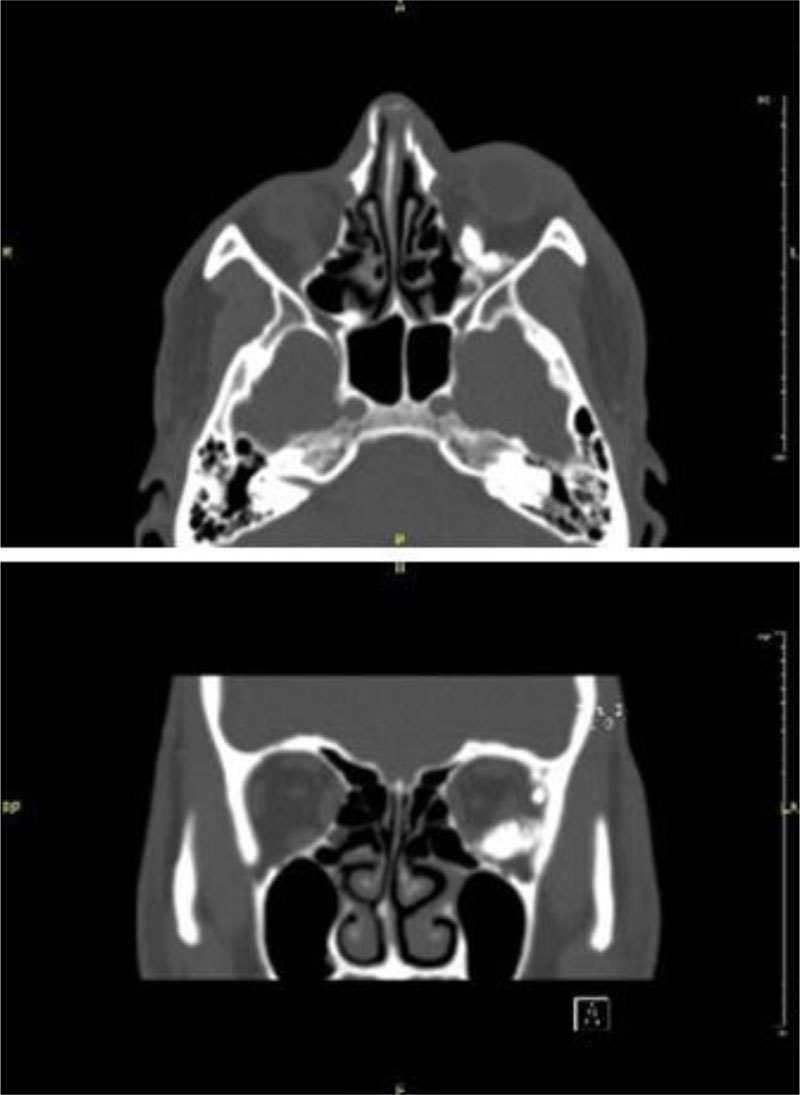 |
Fig. (5). Additional foreign body particles removed in the second operation. |
 |
Fig. (6). Additional foreign body particles removed in the second operation. |
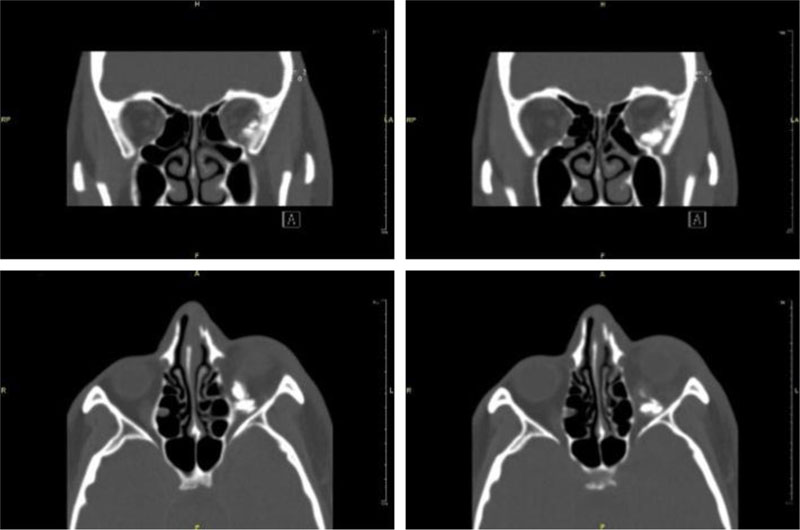 |
Fig. (7). Computed tomography [CT] done after the second operation. |
Upon the second post-operative CT, the residual FBs in the extraconal space, inferior to the inferior and lateral rectus were partially removed, and fragmented FBs remained in that area.
Left lateral rectus was edematous and pushed medially (Fig. 7).
The third operation aimed to remove the remnants of the FBs, and to correct ptosis, unfortunately, upon exploring the orbit, only little number of FBs was removed, as the removal of the rest FBs was not possible without injuring the globe, thus, proceeding with the FBs removal was aborted. Ptosis correction was done by levator resection.
2.4. Follow up and Outcomes
The patient recovered well after these multiple sight saving operations, luckily, the patient regained a 0.5 visual acuity, with impressive improvement in the extraocular muscle motility, with only mild restriction in the upper and lower gazes. The patient was followed up for 2 years after the incident, he was stable during that period (Fig. 8).
 |
Fig. (8). Extraocular muscle after the third operation. |
3. DISCUSSION
IOFB is any object located in the bony orbital walls but outside the ocular globe. It can be classified according to foreign body [FB] composition or its location. Locational classification can be either extraconal or intraconal. FB composition can be classified into metallic and non-metallic, non-metallic FBs in turn can be subclassified into organic and non-organic [3, 6].
The rate of occurrence of IOFB in orbital injuries is around 16%, the incidence is unknown [ 7 ]. IOFB is usually associated with occupational accidents, gunshot injuries and motor vehicle accidents.
CT scan is generally considered the gold standard for intra-orbital FBs. Different materials are present in different ways which cause a challenge in identifying the type of material. Wooden FBs -for example- can present with densities similar to that of the intraconal muscles. CT scan
also has an advantage in excluding orbito-cranial extension, abscess formation and diagnosing orbital wall fractures [4]. Other modalities like plain radiograph, ultrasound, and MRI can be
used if CT was not available. Although ultrasound is time-consuming and depends on expertise, it has higher sensitivity than plain radiographs [4], careful consideration must be taken as pressure from the probe could cause wound enlargement in a previously damaged globe wall. MRI should be used when material could not be identified by a CT scan or a false negative CT scan. An important point is that MRI requires a pre-MRI imaging to exclude metallic IOFB [4].
FB material might lead to the decision of surgical removal, organic FBs are a great medium for bacterial growth, thus, all organic FBs must be removed surgically, as they are associated with a high risk of orbital cellulitis. Although most metals are inert, some might cause serious orbital morbidity [8, 9]. Inert and inorganic FBs may be followed up with observation if asymptomatic, however, removal of ferromagnetic FBs should be considered as they may prevent patients from undergoing future magnetic reson ance imaging [MRI] [9].
Possible complications of surgical removal of FBs include orbital hemorrhage, optic nerve damage, and orbital compartment syndrome. (Table 1) summarizes the indications of surgical removal of FBs.
In the current case, the rationale for surgical intervention was the acute presentation of multiple large IOFB, and orbital compartment syndrome which prompt the surgical intervention of canthotomy and cantholysis, the significant displacing effect of orbital tissue including the lateral rectus muscle, and the significant effect on scleral indentation.
The type of surgical approach is influenced mainly by the location of FBs. Anterior orbit FBs are mostly removed by the anterior transpalpebral approach. While for retrobulbar FBs, the lateral approach reached about 45% of cases in a case series conducted by Szabo B. et al. [6] Anterior orbital FBs were associated with local inflammatory signs, while posterior orbit and extraconal FBs were noted to cause not only local inflammatory signs but also hemorrhage, mydriasis and globe displacement [6]. With the modern advances in orbital surgical techniques, surgical removal of most orbital FBs has minimal complication rates [9]. In general, anteriorly placed FBs can be removed regardless of the material, as it is easily accessible.
CONCLUSION
IOFB is an ophthalmological emergency, careful history, examination, and investigations are important steps in diagnosing IOFB since it can be easily missed when depending solely on imaging. Timely management is crucial to prevent irreversible complications.
Many cases of IOFB might require more than one surgery to remove FBs and to aid the recovery of the patient. The decision of surgical intervention versus leaving FBs in place is carried out after careful weighting of the risk versus benefit of each course of action. Luckily, the decisions taken by the ophthalmology team in our case lead to a dramatic improvement in the outcome. Teamwork of ophthalmological subspecialties plays a major role in the outcome, considering the complexity of such cases.
LIST OF ABBREVIATIONS
| IOFB | = Intra-orbital Foreign Bodies |
| FBs | = Foreign Bodies |
| CT | = Computed Tomography |
| MRI | = Magnetic Resonance Imaging |
| FB | = Foreign Body |
AUTHORS’ CONTRIBUTIONS
All authors attest that they meet the current ICMJE criteria for Authorship.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMANS AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient.
STANDARDS OF REPORTING
CARE guidelines have been followed in this study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.







