Clinical Spectrum of Indirect Traumatic Optic Neuropathy in South Indian Subjects Observational Study
Abstract
Purpose:
To report the aetiology, visual outcome, and clinical features of indirect traumatic Optic Neuropathy (TON) patients from the tertiary eye care center in South India.
Methods:
It is a retrospective and observational study. Details of age, gender, number of days of presentation after injury, Snellen visual acuity at presentation and last follow-up, visual evoked potentials, visual field findings using the Humphrey visual field analyser, associated ocular complications, and mode and time of treatment were obtained from the medical records of all indirect TON patients.
Results:
Indirect TON patients are mainly young males (94%) and road traffic accident (RTA) (65%) is the main cause of TON, followed by falls (19%) and sport-related activities (11%). Visual acuity loss was severe in more than 50% of the subjects and only 16%% of the patients showed improvement in visual acuity greater than one line. Pattern visual evoked potentials and visual fields are recordable only in 15% of the subjects. Commonly associated ocular complications in indirect TON patients were orbital fracture (43%), lid tear (16%), sub-conjunctival haemorrhage (13.5%), and angle recession (13.5%). Three out of four patients who received methylprednisolone and oral steroids within a week showed an improvement in visual acuity of greater than three lines, while just one patient out of four who received the same medication after a week improved visual acuity of three lines.
Conclusion:
RTA (road traffic accidents) is the most common cause of indirect TON and mainly young males were the affected individuals. IVMP along with oral steroids within a week, would help TON patients for reasonable visual recovery. Presenting Visual acuity of > 6/600 and recordable pattern VEPs would be the prognostic factors for good visual outcomes in indirect TON patients.
1. INTRODUCTION
Indirect Traumatic Optic Neuropathy (TON) is an indirect injury to the optic nerve following an episode of trauma that leads to severe vision loss [1, 2]. Usually, the diagnosis is based upon the history of trauma, reduced vision, presence of relative afferent pupillary defect (RAPD), reduced colour vision, and an associated field defect [3]. The incidence of TON is estimated between 0.7% and 2.5% of all head trauma cases [4-8]. Males between 20-40 years make up the majority of those suffering from TON, accounting for 60–95 percent of cases [7, 9]. The majority of the cases involved closed head injuries, and various studies have found that loss of consciousness is associated with TON in 40–70% of cases [10, 11]. Reduced best-corrected visual acuity, loss of visual field, loss of colour vision, and the presence of a RAPD (unilateral TON) are the defining features of TON. Electrophysiological tests such as the visual evoked potential (VEP) may aid in the diagnosis of TON in comatose patients with RAPD or bilateral TON. The visual prognosis can also be estimated using VEP [12, 13]. Optical coherence tomography (OCT) could help track axonal damage among TON patients over a time period [14].
The management of TON is contentious [9]. Conservative management, high-dose steroids, low-dose steroids, and surgical management in the form of optic canal decompression in canalicular fracture and optic nerve sheath fenestration in anterior TON and a combination of them have all been tried [15-18]. There are many studies that have shown the clinical profile of Indirect TON patients from the western population, however, there are hardly any studies that have shown the comprehensive clinical profile of TON patients from South India [18-20]. Mainly these studies were focused on either aetiology or ocular complications or treatment protocol or visual outcome of TON patients. As of now, there are no studies from India that reported additional clinical features such as VEP responses and types of visual field defects in indirect TON patients. For a better knowledge of the natural history and treatment of this illness, clinical databases must be developed. Hence, the current study aimed at reporting the etiology, clinical features (that includes visual field defects and VEP responses), management, and visual outcome of TON patients in South Indian population.
2. METHODS
The current study is a retrospective and observational study. Approval of the current study is obtained from the Institutional Review Board of LV Prasad Eye Institute, Hyderabad, India. Its conduct followed the tenets of the Declaration of Helsinki.
2.1. Inclusion Criteria
All the patients who were diagnosed with Indirect traumatic optic neuropathy were included and their records were verified. History of blunt trauma was only included in the study.
2.2. Exclusion Criteria
Patients diagnosed with direct Traumatic optic neuropathy (optic nerve avulsion, optic nerve transection, optic nerve sheath hemorrhage) or penetrating injuries were excluded.
Retrospective data review of indirect TON case records presented at the electrophysiology lab, L V Prasad eye institute were used in this study. All cases underwent thorough eye exams that also looked at any related ocular damage. The primary outcome measure of the study was visual acuity. At the time of presentation, demographic details such as age, gender, number of days of presentation after injury, cause of the injury, Snellen Visual acuity at the presentation time and the last follow-up, visual evoked potentials, visual field findings using Humphrey visual field analyser, associated complications and mode and time of the treatment were retrieved from the medical records of all TON diagnosed patients. The ocular injuries that were present were thoroughly examined and proper referrals were made to neurologists in required cases after the degree of the damage was assessed by reviewing the brain and/or analyzed CT scans.
All the data were analysed using SPSS (Version 21.0) software. Descriptive analysis was reported using Pie and bar charts.
3. RESULTS
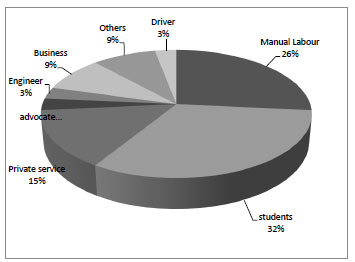
A total of 37 patients were presented for electrophysiology investigation of TON, out of which 94% were males and 6% were females. The median age of this group was 28 years, ranging from 12 to 51 years. The occupation groups of the patients are presented in Fig. (1). The most common occupations of affected patients were students (32%) followed by manual labor (26%). The mean time of presentation after injury was 16 ± 10 days (range: 1 day to 180 days).
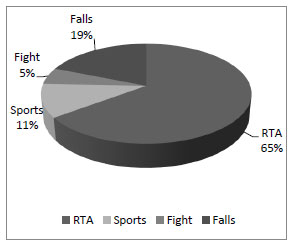
The causes of indirect TON are presented in Fig. (2). Road traffic accident (RTA) is the leading cause of TON (65%) followed by falls (19%) and sports activities (11%) and fight among friends (5%).
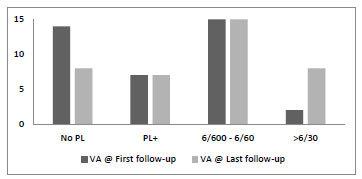
Visual acuity at the presentation and final follow-up were presented in Fig. (3). Presenting visual acuity was 6/60 or less in 35 patients with 14 patients (40%) with no light perception. Improvement of visual acuity, at the last follow-up, was 6/30 or better in 8 (21%) subjects.
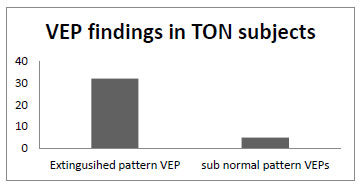
Pattern VEP (Fig. 4) at presentation was extinguished in almost all subjects except five, who have shown subnormal amplitudes with delayed latencies, however, 30 subjects showed reproducible flash VEPs.
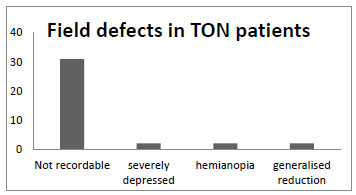
Visual field findings of TON patients at the time of presentation were as shown in Fig. (5). Visual fields were non-recordable in 31 subjects and the remaining subjects showed field defects such as hemianopia, generalized reduction in sensitivity, and central scotoma.
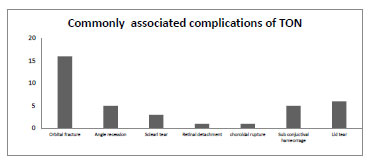
The associated complications among the TON patients are presented in Fig. (6). The commonly associated complication with the trauma was orbital fracture (43%), out of which two were having brain infarcts. Other common complications were angle recession (16%) and lid tear (13%) Fig. (6).
Out of 37 subjects, only 8 patients received IVMP along with oral steroid therapy and reaming 29 patients were treated with topical antibiotics, topical steroids, and nutritional supplements. Visual acuity improvement for two different modalities is presented in Table 1. IVMP along with oral steroid therapy within one week of trauma has shown improvement in visual acuity of greater than three lines in 3 out of 4 subjects. Only one of the four patients, who presented one week after injury and received IVMP therapy, has improved visual acuity better than 3 lines.
| Treatment Strategy | People with IVMP Treatment | Topical Steroids, Topical Antibiotics, or Nutritional Supplements | ||
|---|---|---|---|---|
| - | Within a week | After one week | Within a week | After one week |
| Total patients | 4 | 4 | 2 | 27 |
| > 3 lines of improvement in VA | 3 | 1 | - | - |
| > 1 line of improvement in VA | 1 | 1 | - | - |
| < 1 line of improvement in VA (but can’t be quantified) | - | 2 | 1 | 5 |
| No improvement | - | - | 23 |
4. DISCUSSION
Indirect TON is an uncommon but often devastating cause of permanent vision loss following a blunt injury. Indirect traumatic optic neuropathy is due to the non-penetrating effects of trauma. The mechanisms include bony fragment trauma, optic nerve sheath hematoma, and concussion injury, which occurs when trauma is imparted to the skull and transmitted into the optic nerve [19]. Previous reports from India were mainly studied either with visual outcomes or associated complications or treatment strategies of TON. This is the first study which reported additional clinical features such as visual field defects, pattern VEP response along with the aetiology, visual outcomes and associated complications in indirect TON patients.
4.1. Gender and Aetiology
The majority of the indirect TON patients in the current study were males (94%) with a median age of 28 years and were either students or manual laborers who were hurt in car accidents, falls, or sports. Our findings on the gender and type of trauma experienced by TON patients are generally consistent with earlier studies [6, 9, 20, 21]. According to reports, RTA that results in TON in the younger age group is frequently caused by reckless driving [20].
4.2. Associated Ocular Complications
The commonly associated ocular complications among the TON patients in this study were orbital fractures (43%). Other common complications were angle recession (16%), lid tear (13%) and subconjunctival haemorrhage. Sivakumar et al. [19] study and Deepti [21] et al. studies have also noted that orbital fractures and sub-conjunctival hemorrhages are the most common ocular findings from the Indian cohort of indirect TON patients [19, 21].
4.3. Visual Outcome and Treatment
In the current study, improvement in visual acuity is observed only in 38% of the patients out of which only 16% of the subjects have shown improvement in visual acuity of greater than one line. This is slightly less (50-55%) than the studies reported from India and other parts of the world [15, 17-23]. The probable reason for the difference could be due to most of the current study participants presenting to the eye hospital a week after injury which delayed the treatment plan that lead to poor improvement in visual acuity. Only 4 (11%) patients have an improvement in visual acuity of more than 3 lines after IVMP, along with oral steroid treatment. Three out of four subjects who received IVMP along with the oral steroids within a week time have shown improvement in visual acuity of more than three lines, while only one patient has shown improvement in visual acuity received the same therapy after one week. Out of the 4 subjects who have shown improvement in visual acuity of greater than 3 lines had their presenting visual acuity greater than 6/600. In the current study, visual acuity seems to be the main prognostic factor in determining the final visual outcome. IVMP along with oral steroid therapy, seems to be beneficial within one week of the injury. A recent review [24] on TON suggests that there is no consensus on a preferred treatment for TON based on studies published to date. Each patient's unique needs should be taken into account while creating treatment strategies. To find the best indirect TON treatment plans, more conclusive treatment studies will be required.
4.4. VEP Responses
Pattern VEP response seems to have a diagnostic value and help in the prognosis of vision and rate of visual recovery [25, 26]. The current study has shown only 5 out of 37 patients have shown subnormal pattern VEP responses. All these 5 patients have visual acuity greater than 6/600. Out of these 80% of the patients have shown more than 3 lines of improvement in visual acuity after the IVMP treatment. The current study is in strong agreement with the previous reports [25, 26] that patients with subnormal pattern VEP may tend to improve their vision with steroid therapy.
Despite the fact that patients with TON may have poor visual acuity, automated visual field testing should be considered in all patients [27]. There is no unique visual field defect in TON patients has been observed; nevertheless, arcuate, central, and hemianopic field deficits have been reported [28] previously. The current study has shown that automated perimetry is not recordable in 86% of the patients due to poor vision. However, in the remaining 14% of the patients showed hemianopic, depressed and generalized field defects.
Results from the present study have revealed that most of the patients with TON had ocular and orbital complications and hence there is a need for a multidisciplinary approach. Though this study has shed some light on clinical features, there are some limitations which include a) there is no information in the medical records as to why ophthalmologists selected IVMP therapy in a few patients, not in others; b) patients who were sent to a neurologist or sent for a multidisciplinary approach before they were referred to the electrophysiology clinic may not have been brought back to the hospital. Hence their data may not be included. This may induce bias in the results of the current study; c) RAPD at the presentation was not graded hence it is not analyzed but the observation from the records is that all the patients have RAPD at the time of presentation. Prospective and observational studies with larger samples are needed to confirm our initial findings with randomized control trials on treatment protocols.
5. CONCLUSION
Current study shows that most of the indirect TON patients are usually young males and the main cause of TON is RTA in the south Indian population. Presenting visual acuity of greater than 6/600 and recordable pattern VEP may be prognostic factors for improved visual outcome in TON patients. Most of the TON patients in the current study were treated with conservative treatment, however, results from the current study provide insight that IVMP along with oral steroids within a week of trauma would help the patients recover faster with good visual outcomes.
LIST OF ABBREVIATIONS
| TON | = Traumatic Optic Neuropathy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Institutional Review Board of LV Prasad Eye Institute, Hyderabad, India.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans were used in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013 (http://ethics.iit.edu/ecodes/node/3931).
CONSENT FOR PUBLICATION
Consent is not applicable as it is a retrospective study.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [N.K.C], on special request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


