All published articles of this journal are available on ScienceDirect.
Acute Macular Neuroretinopathy (AMN) following Ergotamine intake in the Postpartum Period: A Case report from Conakry’s Medical Ophthalmologic Center
Abstract
Introduction:
We present a clinical case of postpartum acute macular neuroretinopathy (AMN) and describe clinical characteristics and subsequent pathophysiology.
Case Description:
A twenty-seven-year-old woman previously diagnosed with chronic hypotension developed acute paracentral scotomas in the left eye following an uncomplicated delivery. Best-corrected visual acuity was 20/20 in both eyes. Fundus examination revealed flat, well-demarcated, reddish parafoveal lesions in the left eye.
Corrected visual acuity was 20/20 in both eyes. On fundus examination, well-defined, reddish parafoveal abnormalities were seen in the left eye. Multimodal imagining demonstrated a wedge-shaped defect on near-infrared imaging (NIR), co-located with altered external retinal layers on spectral-domain optical coherence tomography (SD-OCT). Optical coherence tomography angiography (OCTA) demonstrated the presence of non-perfused deep capillary plexuses and choriocapillaris. Detailed investigation disclosed that 200 micrograms of ergotamine had been taken to avoid postpartum hemorrhage. Three months follow-up, a reduction in scotoma was reported.
SD-OCT demonstrated reflectivity defect remediation in the outer retinal layers, and OCTA revealed attenuation of vascular flow vacuity.
Conclusion:
In brief, AMN in the post-partum setting remains exceptionally high. Clinicians must be mindful of this feature and take care when using ergotamine in women with added AMN risks, notably hypotension.
1. INTRODUCTION
Acute macular neuroretinopathy (AMN) was reported initially by Bos and Deutman in 1975 when they described a series of four women with acute visual disturbance and paracentral scotomas consistent with cuneiform macular damage [1].
The pathogenesis of AMN has yet to be fully elucidated, but some evidence points to the existence of deep ischemia of the retinal capillary plexus [2].
Optical coherence tomography angiography (OCTA) enables full visualization of retinal vascular flow, providing a key tool for assessing the extent of a vascular defect [3]. The most frequently documented association with AMN is viral infection. Other associations include oral contraception, high coffee consumption, vasoconstrictive drug intake, hypotension and, recently, vaccination [4].
We report a rare case of postpartum acute macular neuroretinopathy following ergotamine intake. We aim to highlight the importance of identifying this clinical entity in the postpartum context and to provide a credible hypothesis on the mechanism inherent in this disease on the basis of the OCTA findings.
2. CASE DESCRIPTION
We report the clinical presentation of a 27-year-old woman who presented with paracentral scotomas in the left eye immediately after a normal full-term delivery. She suffered from chronic hypotension with a blood pressure of approximately 85/60 mmHg. To prevent postpartum hemorrhage, the patient received a total dose of 200 micrograms of ergometrine administered intramuscularly (IM).
Corrected visual acuity was 20/20 in both eyes. Anterior segment examination showed no abnormalities. Fundus examination revealed reddish, well-delineated parafoveal defects in the left eye (Fig. 1A) and no abnormalities in the right eye.
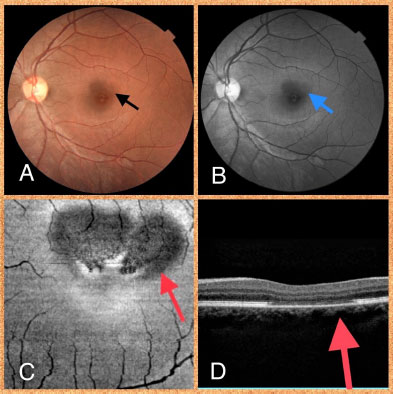

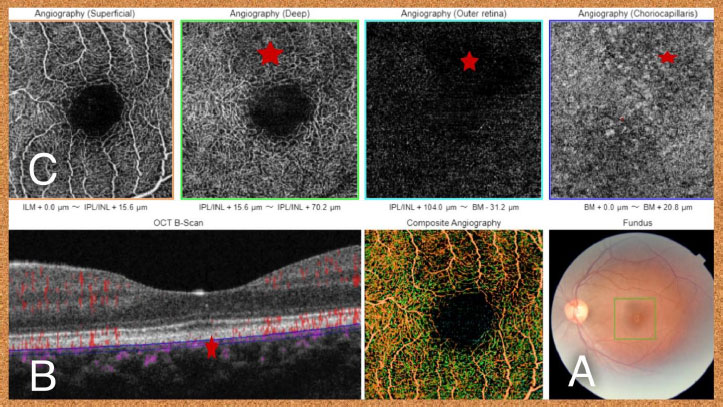
In the red-free imaging, there were dark petalloid perifoveal lesions with the tips pointed toward the fovea (Fig. 1B). Near-infrared (NIR) imaging revealed two petal-shaped hyporeflective upper parafoveal lesions (Fig. 1C). SD-OCT revealed a thinned outer nuclear layer with hyperreflective of the outer retina and rupture of the ellipsoid zone, the outer limiting membrane, and the interdigitation zone (Fig. 1D). OCTA demonstrated superficial capillary plexus normal vascular flow (Fig. 2A), and a vascular flow void (red asterisk) in deep capillary plexus (B), outer retina (C) and choriocapillaris (D) matching the hyporeflectivity noted on near-infrared reflectance imaging (E). Optical coherence tomography angiography (OCTA) revealed normal vascular flow in the superficial capillary plexus (Fig. 2A) and a vascular flow void (red asterix) in the deep capillary plexus (B), outer retina (C) and choriocapillaris (D) that colocalize with the hyporeflectivity seen on NIR imaging (E). Acute macular neuroretinopathy was diagnosed in a post-partum patient.
The patient described a marked reduction in scotomas after three months of follow-up. On ocular examination, visual acuity was stable at 20/20 in both eyes, and fundus lesions had diminished (Fig. 3A). SD-OCT revealed recovery of the reflectivity damage in the outer retinal layers (Fig. 3B, red asterisk), and OCTA revealed attenuation of vascular flow vacuity (Fig. 3C, red asterisk).
| Author | Age | Background | Eye | Lesion Description | Imaging | Recovery |
|---|---|---|---|---|---|---|
| Corver et al 2007 [7] | 30 | Bilateral paracentral scotoma following Caesarean section complicated by the drop in blood pressure treated with intravenous methylergometrin and oral etilephrine. | OU | Bilateral reddish-brown petaloid lesions in both macular regions. |
FA: unremarkable Red-free: abnormal foveal Reflex OCT: Thinned area in the corresponding macular region. |
Reduction in the intensity of the scotoma |
| Vance et al 2011 [8] | 34 | Bilateral paracentral scotoma following caesarean section for a pregnancy complicated by hypertension and proteinuria. | OU | Bilateral reddish-brown, wedge-shaped lesions in the foveal region; | IR: Hyporeflective lesions better delineating the macular lesions. OCT: focal areas of IS/OS boundary loss with thinning of the ONL |
Improved at 3 months |
| Ranjan et al 2012 [9] | 26 | Bilateral central scotoma 1 month after uncomplicated full-term vaginal delivery. | OU | well-circumscribed bean-shaped areas of retinal discoloration superonasal to center of fovea OD and nasal to center of fovea OS | OCT: defect in the reflectivity of the outer retinal layer adjacent to the RPE | Reduction in the intensity of the scotoma |
| Rauchegger et al 2019 [10] | 26 | Bilateral flickering, c-shaped defect of the visual field following Caesarean section complicated by the drop in blood pressure treated with intravenous ephedrine (10 mg) and epinephrine (1 mg). | OU | Bilateral reddish-brown, wedge-shaped lesions | IR: hyporeflective parafoveal wedge-shaped areas OCT: para-foveal disruptions of the ellipsoid and interdigitation zone of the photoreceptor layers ERG: diminished parafoveal amplitudes |
un-changed visual symptoms |
| Our patient 2023 |
27 | paracentral scotomas in the left eye immediately after uncomplicated full-term delivery. | OS | Well-demarcated, reddish parafoveal lesions in the left eye | IR:petal-shaped hyporeflective lesions OCT: thinning of the outer nuclear layer and a disruption of the external limiting membrane, the ellipsoid zone and the interdigitation zone OCTA: flow void in the deep capillary plexus, outer retina and choriocapillaris |
Reduction in the intensity of the scotoma |
3. DISCUSSION
Acute macular neuroretinopathy typically occurs in in young women with risk factors including migraine, oral contraceptives, ergotamine or ephedrine use, hypotension and viral infection [5]. Patients usually present with acute symptoms, such as paracentral scotomas, blurred or preserved vision and metamorphopsia [5]. The course of the disease varies from a few weeks to several months, with results ranging from total recovery of vision to persistent scotomas [6].
Multimodal imaging allowed the diagnosis of AMN in our patient presenting with paracentral scotomas in a postpartum context. There are only four published reports on cases of AMN occurring after the post-partum period, three of which were delivered by caesarean section and one by vaginal delivery [7-10] (Table 1). Two patients developed hypotension during caesarean section and received oral methylergometrin and etilephrine in one case [5] and ephedrine and epinephrine in the second case [10].
The patient suffered from chronic hypotension, with no evidence of an acute fall in blood pressure before the onset of symptoms. However, she received ergometrine, known to trigger acute ischemic damage and peripheral vessel constriction [8, 11]. Lupton et al. [12] demonstrated changes in retinal microvascularization during pregnancy, consisting of initial vessel dilation in the second trimester, followed by gradual vessel constriction for the rest of the pregnancy. We speculate that these coincident hemodynamic conditions during pregnancy may have exacerbated the ergotamine vasoconstrictive action on the choriocapillaris and retinal microvasculature, leading to ischemia at this level.
Diagnosis of AMN relies on multimodal imaging combining NIR imaging, SD-OCT with B-scan analysis and, more recently, optical coherence tomography angiography (OCTA) [13].
A typical corner-shaped defect on NIR imaging, associated with outer retinal layer defects on SD-OCT and non-perfusion in the deep capillary plexuses and choriocapillaris on OCTA, has been frequently documented in AMN [14].
AMN's pathogenesis is not fully clarified, but it has been suggested that deep retinal capillary plexus and choriocapillaris ischemia cause hypoxic retinal damage [15, 16]. OCTA can represent an invaluable tool in multimodal imaging in AMN, permitting visualization of retinal microvasculature perfusion at different levels. No previous reports on the use of A-OCT in AMN in post-partum settings were identified in our literature review.
Hypotension and ergotamine's vasoconstrictive properties may indeed have contributed to ischemic damage involving the deep capillary plexuses and choriocapillaris, as demonstrated by OCT-A and contributing to the development of AMN [17].
In a similar case reported by Vance et al., the authors suggested that methylergometrine-trine-induced vasoconstriction in the chorioretina leads to AMN in the postpartum period [6].
Acute macular neuroretinopathy is generally a self-limiting disease that does not necessitate treatment. As in our patient's case, resolution of fundus defects and outer retinal layer restoration on SD-OCT are common; however, paracentral scotoma may persist months or even years later [17].
Follow-up is based on the results of multimodal imaging and patient symptomatology. Multimodal imaging, including new diagnostic tools, such as OCTA, was described in post-partum AMN for the first time in this case report. OCTA assists not just in the diagnosis and monitoring of this rare disease but also in describing the retinal microvasculature damage observed in this condition, supporting the hypothesis of the ischemic effect of ergotamine in this report.
Retinal vascular occlusions may occur in the postpartum period, such as central retinal artery occlusion [18], AMN [7-10], central retinal vein occlusion [19], cilioretinal artery occlusion [19], and Purtscher’s-like retinopathy [20]. Pregnancy by itself can be a risk factor for retinal vascular thrombosis. Indeed, normal pregnancy is associated with a state of systemic hypercoagulability, which may continue into the post-partum period to prevent delivery hemorrhage [21].
In conclusion, in the case of post-partum AMN, a systemic workup is necessary to investigate a state of thrombophilia, which may be exacerbated by undiagnosed pre-existing underlying thrombotic disease, hypotension induced by post-partum hemorrhage or the use of vasoconstrictive drugs.
CONCLUSION
Ergometrine is commonly administered in obstetrics for the prevention of postpartum hemorrhage.
We describe here a further case of AMN, which occurred in a young woman in the postpartum setting following ergotamine intake. This event deserves serious consideration by healthcare professionals and must be seriously considered in patients requiring ergotamine, particularly those at additional risk of AMN.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
Written informed consent for publication of the clinical details and clinical images was obtained from the patient.
STANDARDS OF REPORTING
CARE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


