All published articles of this journal are available on ScienceDirect.
Comparison of Efficacy and Safety of Slow Coagulation Transscleral versus Micropulse Cyclophotocoagulation in Refractory Glaucoma
Abstract
Background
Cyclodestructive laser technology has been developed with the aim of achieving a greater reduction in Intraocular Pressure (IOP) with minimal complication. Micropulse transscleral cyclophotocoagulation (MP-TSCPC) and slow-coagulation continuous-wave transscleral cyclophotocoagulation (SC-TSCPC) are considered to have less complications than conventional techniques using continuous-wave transscleral cyclophotocoagulation.
Purpose
To compare IOP reduction and complications in refractory glaucoma after SC-TSCPC and MP-TSCPC procedures.
Methods
This study is a prospective interventional study in refractory glaucoma patients. Measurement of IOP using Goldmann applanation tonometry was performed preoperatively, and all patients were monitored at days 1, 7, and 30 in the postoperative period. Success was defined as postoperative IOP reduction of > 20% from baseline with or without glaucoma medication. Complications were identified by evaluating subjective complaints and slit lamp examination.
Results
The study included a total of 66 eyes, with 33 eyes in each group. Baseline IOP was 50.58 ± 9.937 mmHg and 48.45 ± 12.792 mmHg in SC-TSCPC and MP-TSCPC group, respectively. The mean IOP reduction was 27.44 ± 19.96% vs 14.39 ± 23.52% (p=0.018) in day 1, 46.19 ± 27, 7 3% vs 45.83 ± 24,80% (p=0,956) in day 7 and 46.49 ± 24.63% vs 27.09 ± 23.86% in day 30 (p=0.002), in SC-TSCPC and MP-TSCPC group respectively. Complications between groups were not significantly different. However, hypotonia (IOP < 6 mmHg) was found in the SC-TSCPC group.
Conclusion
SC-TSCPC showed greater IOP reduction than MP-TSCPC, with no significant differences in complications between the two groups.
1. INTRODUCTION
Glaucoma is the major cause of irreversible blindness. Based on data from the International Agency for the Prevention of Blindness (IAPB) Vision Atlas 2020, glau-coma is the third leading cause of blindness globally, accounting for 11% [1, 2]. The continent with the most glaucoma sufferers is Asia. In Indonesia, outpatient glaucoma patient visits to outpatient services during 2015-2017 increased from 65,774 visits to 427,091 visits [3].
Intraocular Pressure (IOP), as a modifiable risk factor for glaucoma progression, is shown in clinical trials to slow or halt disease progression [4-6]. Therefore, the main glaucoma management is IOP reduction. [6] The initial management is topical medications, but the majority of the patients have a comorbidity, namely ocular surface disease [6]. In addition, suboptimal IOP control and blindness can be caused by topical medications. [6] The long-term complications, namely hypotony, infectious endophthalmitis, and bleb-related complications, are the main concern, even managed by filtering surgery for reducing IOP [6]. Conventional trabeculectomy does not show good results on certain glaucomas; glaucoma that does not respond to medical or conventional surgical treatment is called refractory glaucoma, which is often recurrent. Namely, childhood, neovascular, uveitic, traumatic, glaucomas with wide conjunctival scars, post-vitrectomy, post-keratoprosthesis, post-keratoplasty, ciliary block, recurrent, aphakic glaucoma and pseudo-phakic glaucoma. Some glaucoma needs specific manage-ment, yet surgical is needed in most cases, namely anti- metabolites-assisted trabeculectomy, drainage implants, cyclodestructive surgeries, and others. [7] Glaucoma drainage devices and cyclodestructive lasers can be used to treat refractory glaucoma cases that do not achieve target therapy after maximum medical therapy with incisional surgery such as trabeculectomy [4,5]. The Transscleral Cyclophotocoagulation (TSCPC) is a cyclo-destructive laser that uses an 810 nm diode laser, which will be absorbed in the pigmented epithelium of the ciliary process, hence reducing the formation of aqueous humor. It aims to decrease the production of aqueous humor, which will lead to a reduction in IOP. Ciliary body photocoagulation is caused by an absorption of melanin in the ciliary processes from the transmission of a laser beam through the sclera. Continuous semiconductor diode laser (810nm) laser has been used for TSCPC due to its efficacy, cost, and portability. However, the conventional continuous wave TSCPC (CW-TSCPC) laser may sometimes cause visual impairment, namely Cystoid Macular Edema (CME), vitreous hemorrhage, hyphema, sympathetic ophthalmia, persistent hypotonia, and phthisis bulbi. Continuous-wave TSCPC (CW-TSCPC) can be used as a final attempt for refractory glaucoma, which has severe visual potential or high risk for incisional glaucoma [5-9].
Cyclodestruction laser has been developed with the aim of achieving a significant impact of IOP reduction with minimal complications. Recently, a micro pulsed laser has been developed for transscleral cyclophotocoagulation. [8] It administers a series of short pulses of diode laser separated by pauses. The cyclic laser allows energy to build up in targeted pigment tissues, which reaches a phototherapeutic state; simultaneously, the pauses allow the adjacent non-pigmented tissues to soothe and remain below the photo coagulative threshold. It minimizes the collateral tissue damage after CW-TSCPC [8]. These cyclodestructive laser approaches include micro pulse TSCPC (MP-TSCPC) and slow coagulation TSCPC (SC-TSCPC). The MP-TSCPC laser uses a 31.3% on-and-off cyclic method to allow a rest period with minimal damage to the collateral tissue, with a laser power of 2000 mW. The non-pigmented tissues are not damaged due to less energy per burst that pauses between pulses. Therefore, they accumulate less energy per unit of time and rarely reach the critical energy threshold for photocoagulation. [9] Slow coagulation TSCPC laser procedure uses continuous waves but with a lower power parameter, which is 1250 mW, and a duration of 4000-45000 ms without a “pop” sound. Its settings and technique utilize fixed low energy based on iris pigmentation degree. SC-TSCPC laser shows IOP reduction as well as CW-TSCPC with minimal complications [1, 10]. Until now, there has been no study that directly compares the SC-TSCPC procedure with MP-TSCPC. This study aims to compare the IOP reduction and postoperative complications between SC-TSCPC and MP-TSCPC procedures in refractory glaucoma.
2. MATERIALS AND METHODS
This study was an interventional study, and the subjects were divided into two groups: MP-TSCPC and SC-TSCPC. Data collection was conducted from October 2022 until March 2023 after the Ethical Committee of the National Eye Center Cicendo Eye Hospital, Bandung, Indonesia, approved. Inclusion criteria in this study were patients with refractory glaucoma, both old and new patients, who had received maximum medical therapy with or without prior incisional surgery; an adult older than 18 years old; a low vision potential of 1/300; light perception (LP) or no light perception (NLP); patients with or without a prior history of TSCPC, with minimum interval 3 months from previous TSCPC; as well as patients who refused or were not included in the list of candidates for filtration surgery. Exclusion criteria in this study were patients who refused to participate in this study, as well as patients with contraindications to TSCPC, such as patients with thin sclera. The criteria for dropping cases out of this study were patients who did not show up for day 7 and/or day 30 follow-up visits or patients who were uncooperative during the TSCPC procedure or examination process. The criteria for success in this study was >20% IOP reduction.
The patient underwent a pretreatment examination including visual acuity, IOP measurement using the gold standard Goldmann applanation tonometry, the anterior segment using a slit lamp, and the posterior segment examination. After block randomization, the patients were divided into two groups based on the intervention: SC-TSCPC and MP-TSCPC. The TSCPC procedure was previously performed in the operating room under peribulbar anesthesia. Post-laser medication contained the topical steroid prednisolone acetate 10 mg/mL and paracetamol 500 mg orally as analgesics. Post-laser monitoring was carried out on the 1st, 7th, and 30th days, including subjective assessment, IOP, visual acuity, and examination of the anterior and posterior segments with or without diagnostic tests.
2.1. Laser Procedure
The MP-TSCPC laser used an IRIDEX machine with an MP3 probe. The laser wave was cyclic, with a laser period of 0.5 ms followed by a rest period of 1.1 ms (31.3%). The laser moved 360° on the posterior limbus, avoiding the 3 and 9 o'clock meridians. The energy used for IOP <50 mmHg was 2250 mW for 80 seconds/hemisphere, while for IOP >50 mmHg, the energy used was 2500 mW for 80 seconds/hemisphere. The SC-TSCPC laser used a continuous-wave 810 nm diode laser with a G probe. The laser was carried out 360° at as many as 16–20 points in the posterior limbus area without being followed by a “pop” sound. The energy used for the Indonesian population, which had a dark iris color, was 1250 mW for 4500 ms for patients aged <50 years and for 4000 ms for patients aged >50 years, by avoiding the 3 and 9 o'clock meridians. The duration and power will be reduced when a patient complains. If a 'pop' sound emanated during the procedure, the power will be reduced by 50 mW.
Statistical analysis was performed to compare the two groups. Numerical variables were analyzed using the paired test to see if the data were normally distributed, and the Mann-Whitney test to see if they were not normally distributed. Categorical variables were analyzed using the Chi-Square test or the Exact Fisher and Kolmogorov Smirnov test if the Chi-Square test criteria were not met. The significance criterion used was a value of p <0.05, meaning statistically significant. The data obtained was processed using SPSS version 24.0 for Windows and Microsoft Excel.
3. RESULTS
There was a total of 66 eyes from 66 patients, with 33 eyes in each intervention group. The mean age in the SC-TSCPC group was 50.27 ± 14.51 years, and in MP- TSCPC, 52.12 ± 14.58 years, with a male predominance in the SC-TSCPC group (51.5%) while in the MP-TSCPC group, TSCPC was dominated by women (63.6%). Visual acuity in both groups was mostly NLP, with the most etiology of refractory glaucoma in the SC-TSCPC group was neovascular glaucoma (NVG) 45.5% and in the MP-TSCPC group was primary angle closure glaucoma (PACG) 30.3%. Laser action in this study was the primary/first TSCPC procedure in the majority of both groups. The mean total energy used in the SC-TSCPC group was 96.98 ± 13.669 J, while in the MP-TSCPC group was 118.25 ± 6.480 J (p=0.0001). Table 1 presents the demographic data of patients in both groups.
| Variable |
TSCPC SC-TSCPC MP-TSCPC |
P value | |
|---|---|---|---|
| Age (years) | - | - | 0,112 |
| Mean±Std | 50,27±14,507 | 52,12±14,581 | - |
| Median | 52,00 | 54,00 | - |
| Range (min-max) |
22,00-77,00 | 19,00-83,00 | 0,215 |
| Gender | - | - | - |
| Male | 17(51,5%) | 12(36,4%) | - |
| Female |
16(48,5%) | 21(63,6%) | 0,843 |
| Visual Acquitye | - | - | - |
| 1/300 | 8(24,2%) | 5(15,2%) | - |
| LP | 4(12,1%) | 2(6,1%) | - |
| NLP |
21(63,6%) | 26(78,8%) | 0,448 |
| Glaucoma Diagnosise | - | - | - |
| POAG | 0(0,0%) | 2(6,1%) | - |
| PACG | 5(15,2%) | 10(30,3%) | - |
| PEXG | 1(3,0%) | 1(3,0%) | - |
| NVG | 15(45,5%) | 9(27,3%) | - |
| JOAG | 1(3,0%) | 3(9,1%) | - |
| Uveitic glaucoma | 6(18,2%) | 4(12,1%) | - |
| Other secondary glaucoma | 4(12,1%) | 4(12,1%) | - |
| Ghost-cell glaucoma |
1(3,0%) | 0(0,0%) | 0,969 |
| Lens Status | - | - | - |
| Phakic | 28(84,8%) | 24(72,7%) | - |
| Pseudophakic | 4(12,1%) | 8(24,2%) | - |
| Aphakic |
1(3,0%) | 1(3,0%) | 0,438 |
| Previous Glaucoma Interventions | - | - | - |
| Yes | 10(30,3%) | 13(39,4%) | - |
| No |
23(69,7%) | 20(60,6%) | 0,999 |
| History of Glaucoma Intervention 1e | - | - | - |
| No | 23(69,7%) | 20(60,6%) | - |
| Trabeculectomy | 2(6,1%) | 6(18,2%) | - |
| TSCPC | 6(18,2%) | 4(12,2%) | - |
| Trabeculectomy + IOL | 0(0,0%) | 1(3,0%) | - |
| Combined + IOL |
2(6,1%) | 2(6,1%) | 0,999 |
| History of Glaucoma Intervention 2e | - | - | - |
| No | 30(90,9%) | 27(81,8%) | - |
| Trabeculectomy | 0(0,0%) | 1(3,0%) | - |
| TSCPC | 3(9,1%) | 5(15,2%) | - |
| Trabeculectomy + IOL | 0(0,0%) | 0(0,0%) | - |
| Combined + IOL |
0(0,0%) | 0(0,0%) | 0,769 |
| TSCPC Procedure | - | - | - |
| Primary | 26(78,8%) | 25(75,8%) | - |
| Re-treatment | 7(21,2%) | 8(24,2%) | - |
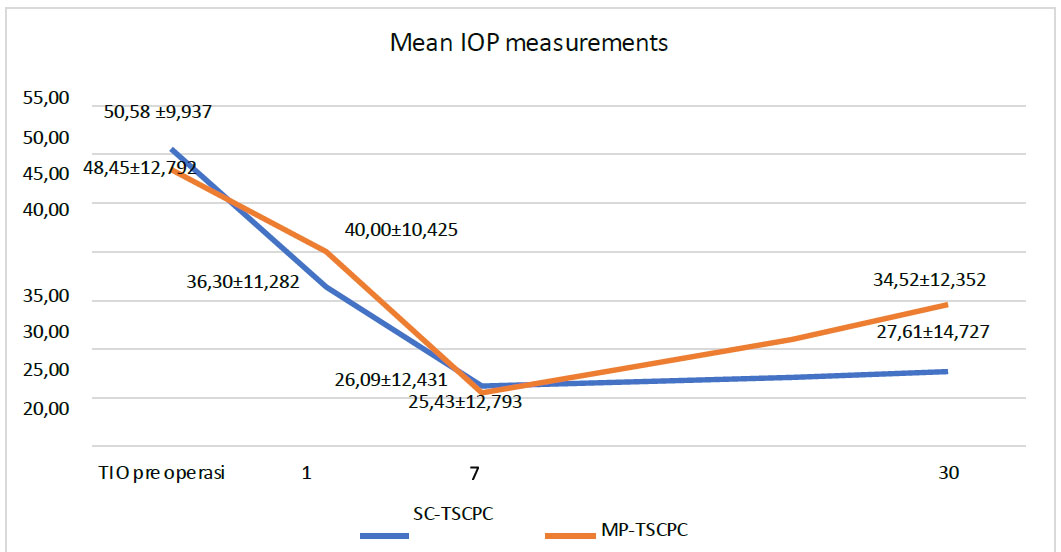
Mean IOP measurements between SC-TSCPC and MP-TSCPC.
Fig. (1) depicts the evolution of IOP in both groups over time. Baseline intraocular pressure in both groups was 48.45 ± 12.792 mmHg (MP-TSCPC) and 50.58 ± 9.937 mmHg (SC-TSCPC). Both groups displayed a decline of IOP on the 1st and 7th days of monitoring but increased on the 30th day. Intraocular pressure reduction after the SC-TSCPC on the 1st, 7th, and 30th monitoring days showed a greater percentage compared to MP-TSCPC, 27.44± 19.96% vs 14.39±23, 52% on the first day (P=0.018), 46.19±27.73% vs 45.83±24.80% on the 7th day (P=0.956), and 46.49±24.63% vs 27.09±23.86% on day 30 (P=0.002). The degree of IOP reduction and the number of patients with a successful rate of IOP reduction > 20% on the 7th and 30th days of monitoring were found to be greater in the SC-TSCPC group, although this difference was not statistically significant (Table 2).
The use of anti-glaucoma medications in the SC-TSCPC and MP-TSCPC groups had the same median both before treatment. Days 7 and 30 monitoring had a median of two anti-glaucoma medications. The two groups showed significant differences on the 7th day of follow-up (P<0.05) (Table 3).
Table 2.
| Variable |
TSCPC SC-TSCPC MP-TSCPC |
P value | |
|---|---|---|---|
| IOP reduction day-1a | - | - | 0,018* |
| Mean±Std | 27,44±19,96 | 14,39±23,52 | - |
| Median | 29,82 | 16,67 | - |
| Range |
-16,67-64,58 | -50,00-58,82 | 0,956 |
| IOP reduction day-7a | - | - | - |
| Mean±Std | 46,19±27,73 | 45,83±24,80 | - |
| Median | 46,67 | 48,15 | - |
| Range |
-10,00-91,07 | -16,28-93,75 | 0,002* |
| IOP reduction day-30a | - | - | - |
| Mean±Std | 46,49±24,63 | 27,09±23,86 | - |
| Median | 53,33 | 34,43 | - |
| Range |
1,79-93,75 | -39,53-65,52 | 0,523 |
| IOP reduction day-7 >20%c (n = 33) | - | - | - |
| Yes | 28(84,8%) | 26(78,8%) | - |
| No | 5(15,2%) | 7(21,2%) | - |
| IOP reduction day-30 >20% (n = 33) | - | - | 0,122 |
| Yes | 24(72,7%) | 21(63,6%) | - |
| No | 9(27,3%) | 12(36,4%) | - |
| Variable |
TSCPC SC-TSCPC MP-TSCPC |
P value | |
|---|---|---|---|
| Number of medication pre-treatments | - | - | 0,362 |
| Mean±Std | 2,27±0,517 | 2,39±0,496 | - |
| Median | 2 | 2 | - |
| Range | 1-3 | 2-3 | 0,030* |
| Number of medication day-7 | - | - | - |
| Mean±Std | 2,00±0.,33 | 1,70±0,728 | - |
| Median | 2 | 2 | - |
| Range |
0-3 | 0-3 | 0,657 |
| Number of medication day-30 | - | - | - |
| Mean±Std | 1,94±0,659 | 1,91±0,579 | - |
| Median | 2 | 2 | - |
| Range | 0-3 | 0-3 | - |
| Variable |
TSCPC SC-TSCPC MP-TSCPC N=33 N=33 |
P value | |
|---|---|---|---|
| Complications day-1e | - | - | 0,999 |
| Absent | 28(84,8%) | 28(84,8%) | - |
| Pain | 1(3,0%) | 3(9,1%) | - |
| Hypotonia | 0(0,0%) | 1(3,0%) | - |
| AC infl. |
4(12,1%) | 1(3,0%) | 1,000 |
| Complications day- 7e | - | - | - |
| Absent | 22(66,7%) | 24(72,7%) | - |
| Pain | 8(24,2%) | 7(21,2%) | - |
| Hypotonia | 1(3,0%) | 1(3,0%) | - |
| AC infl. | 1(3,0%) | 1(3,0%) | - |
| Hematoma |
1(3,0%) | 0(0,0%) | 1,000 |
| Complications day-30d | - | - | - |
| Absent | 32(97,0%) | 33(100,0%) | - |
| Hypotonia |
1(3,0%) | 0(0,0%) | 0,843 |
| Baseline Visual Acuitye | - | - | - |
| 1/300 | 8(24,2%) | 5(15,2%) | - |
| LP | 4(12,1%) | 2(6,1%) | - |
| NLP | 21(63,6%) | 26(78,8%) | - |
| Visual acuity day-1e | - | - | 0,843 |
| 1/300 | 8(24,2%) | 5(15,2%) | - |
| LP | 4(12,1%) | 2(6,1%) | - |
| NLP | 21(63,6%) | 26(78,8%) | - |
| Visual acuity day-7e | - | - | 1,000 |
| 1/300 LP |
5(15,2%) 4(12,1%) |
5(15,2%) 2(6,1%) |
- |
| NLP | 24(72,7%) | 26(78,8%) | - |
| Visual acuity day-30e | - | - | 1,000 |
| 1/300 LP |
5(15,2%) 3(9,1%) |
4(12,1%) 2(6,1%) |
- |
| NLP | 25(75,8%) | 27(81,8%) | - |
| Decreased visual acuity | - | - | 0,197 |
| Yes | 5(15,2%) | 1(3,0%) | - |
| No | 28(84,8%) | 32(97,0%) | - |
There was no significant difference in complication between the two groups. On the first day of evaluation, 12.1% of patients in the SC-TSCPC group had anterior chamber inflammation, whereas 9.1% of MP-TSCPC patients complained of pain. On the seventh day of evaluation, 24.2% and 21.2% of patients in the SC-TSCPC and MP-TSCPC groups complained of pain. Also found one patient with hypotonia on the 30th day. Decreased visual acuity was found in 15.2% of SC-TSCPC patients and 3.0% of MP-TSCPC patients, although the differences between the two were not significant. Complications and decreased visual acuity are presented in Table 4.
4. DISCUSSION
Slow coagulation TSCPC uses the same continuous 810 nm wave laser with a difference in power and duration parameters. It is believed that using 1250 mW power for 4000–4500 mW without making a “pop” sound can reduce IOP just as effectively as CW-TSCPC with fewer complications. The “pop” sound itself is a sign of an explosion of energy and damage to the ciliary process tissue [4, 5, 11]. There hasn't been a study up to this point that compares the degree of IOP reduction and complications between SC-TSCPC and MP-TSCPC procedures.
The IOP measurements of both laser groups on the first and seventh day showed a gradual decrease compared to the baseline IOP, but these IOP measurements showed an increase in POD-30. In a study of MP-TSCPC patients, Zemba et al. found that the average preoperative IOP was 34.7±10.3 mmHg, dropped to 21.4±12.9 mmHg on the seventh day, and then raised back to 23.1±8.5 mmHg over one-month monitoring [12, 13]. According to research by Vries et al. using the MP-TSCPC, the average IOP on days 1, 7, and 30 was 20.2±8.8mmHg, dropped to 16.6±7.2mmHg, and then raised back to 18.2±8.5mmHg [14]. The efficacy of IOP reduction between SC-TSCPC and MP-TSCPC laser cyclophotocoagulation has not yet been directly compared in any previous study. According to Chang et al., the MP-TSCPC demonstrated an average decrease in IOP of 27.3%, 30.6%, 28.8%, and 27.7% on the first, seventh, one-month, and three-month post-operative monitoring visits [6]. In the Jammal et al. investigation, the MP-TSCPC laser demonstrated a lower IOP reduction effect than the conventional CW-TSCPC continuous laser, specifically 44.7% (CW- TSCPC) and 37.8% (MP-TSCPC) on day 7 and 30, respectively [13]. Zemba et al. study revealed that MP-TSCPC had less IOP decrease than CW-TSCPC, with day 1 monitoring at 38.3% and 43.5% and month monitoring at 32.6% and 36.7% [12]. The SC-TSCPC laser, which uses lower power and a longer duration parameter than CW-TSCPC, is said to have the same level of IOP reduction as CW-TSCPC [10]. A study by Khodeiry et al. stated that the TSCPC slow coagulation method had an average IOP reduction of 45.8%, and 72.2% of patients achieved an IOP reduction of >20% [1]. Fong et al.'s study that examined a comparison of CW-TSCPC with SC-TSCPC in 22 respondents showed that SC-TSCPC reduced IOP by 47.6±21.8% at one- week monitoring, 45.3%±31.2% at one- month monitoring, and 35.0±29.1% at 12-month monitoring [5]. Another study by Khodeiry et al. showed a reduction of IOP by 53.2%, 48.2%, and 44.1% at one week, one month, and three months respectively, post SC-TSCPC laser follow-up [1]. Fong et al. concluded that slow coagulation procedures with longer exposure duration and lower continuous power were just as effective as the conventional laser [5].
In this study, the MP-TSCPC group had a significantly greater mean energy than the SC-TSCPC group, which was 118.25 ±6.48 J in the MP-TSCPC group and 96.98 ± 13.669 J in the SC-TSCPC group. Fong et al. study used a lower mean energy in the SC-TSCPC group, 58.8 ± 12.4 J. In William et al. study, the mean total energy used in the MP-TSCPC group was 187.2 J. Emanuel et al. showed a decrease in IOP 41.2% using a duration of 320 seconds and a power of 2000mW (199.68 J) [16]. Duerr et al. showed a significant difference in total energy between SC-TSCPC procedure (101.16 Joules) and CW-TSCPC (77.55 Joules). Both procedures showed a significant decrease of IOP by 17.77 and 13.63 mmHg for the slow coagulation TSCPC and CW-TSCPC procedures [10]. The Asian race with higher pigment levels allows the ciliary processes to absorb greater laser energy therefore it only requires lower laser energy at the time of action. [5]
There was no significant difference in complications between the two groups, although there was one eye with persistent hypotonia at day 30 follow-up in the SC- TSCPC group, which was the patient with glaucoma uveitis. Complications of decreased visual acuity in the SC-TSCPC group showed a greater reduction in visual acuity compared to MP-TSCPC, although the difference was not statistically significant. Five patients (15.2%) in the SC-TSCPC group had deterioration of visual acuity to NLP. The decrease in visual acuity experienced by patients can be caused by cyclodestructive laser procedures or the progressivity of the glaucoma itself. Another study stated that complications that occurred in patients who underwent MP-TSCPC laser included hypotonia by 8.8%, inflammation of the anterior chamber by 26%, and 16.5% experienced a decreased two or more lines of visual acuity, macular edema by 5%, and 2.5% of patients had phthisis bulbi [15]. A study by Khodeiry et al. showed that postoperative complications in the SC-TSCPC procedure were also minimal, 16.7% of patients had decreased two lines of visual acuity, 11.1% had iridocyclitis at one-month monitoring, and 5.6% experienced cystic macular edema and 5.6% of patients suffered from hypotonia. [1] Fong et al. described that in the SC- TSCPC group, hyphema complications were found in 9% of respondents, hypotonia in 5% of respondents, and decreased visual acuity in 9% of respondents. The majority of SC-TSCPC subjects are patients with neovascular glaucoma, hence causing a hyphema [5].
The limitations of this study were, first, the relatively short follow-up time, which was one month; second, this study did not include refractory glaucoma patients who still have visual potential. Therefore, it was not possible to assess the safety of the SC-TSCPC and MP-TSCPC procedures for visual acuity; third, the wide range of variables in lowering IOP can be influenced by varied diagnoses of glaucoma and history of TSCPC or previous surgery; fourth, power recordings in the laser report paper were not detailed, this could affect the calculation of the total energy used [15, 16].
CONCLUSION
In conclusion, the SC-TSCPC cyclo destruction laser procedure showed a greater level of IOP reduction than MP-TSCPC at days 1, 7, and 30 monitoring and was statistically significant at days 1 and 30. The SC-TSCPC group had a greater successful rate of >20% reduction in IOP than the MP-TSCPC group. There were no statistically significant differences between complications of the two procedures. However, there was a greater decrease in visual acuity in the SC-TSCPC group.
AUTHORS’ CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| IOP | = Intraocular Pressure |
| SC-TSCPC | = Slow-coagulation Continuous-wave Transscleral Cyclophotocoagulation |
| MP-TSCPC | = MiCropulse Transscleral Cyclophotocoagulation |
| IAPB | = International Agency for the Prevention of Blindness |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by Ethical Committee of the National Eye Center Cicendo Eye Hospital, Bandung, Indonesia (Number: LB.02.01/2.3/ 13363/2022).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available in the Cicendopedia at https://s.id/cicendopedia.


