All published articles of this journal are available on ScienceDirect.
Argentinian Flag Sign during Cataract Surgery: Case Reports
Abstract
Purpose
Three case reports involving the Argentinian Flag Sign (AFS) during cataract surgery are presented in this paper with a discussion of the relevance to patients with a history of vitrectomy and silicone oil usage. Insights into the management of cases with similar complications, including surgical strategies, intraoperative findings, and post-surgical outcomes, are offered.
Case Presentations
Cases 1, 2, and 3 involved a 47-year-old female, a 26-year-old female, and a 57-year-old male, all of whom had a history of retinal detachment, vitrectomy, and silicone oil use. The AFS was observed during cataract surgery in all patients. Intraocular Lens (IOL) implantation was successfully achieved and visual acuity improved in all cases.
Conclusion
The observation of AFS is more common in younger patients and those with a history of vitreoretinal surgery, and poses surgical challenges to avoid significant impact on postoperative visual acuity. Appropriate preoperative assessment to inform the choice of surgical technique is vital to ensure successful outcomes. Stable anterior chamber pressure should be maintained and the emulsified cortex must be carefully removed. Individualized adjustment of fluid dynamics is required to minimize the risk of radial tearing of the anterior capsule. In conclusion, favorable outcomes may be achieved despite the appearance of the AFS during cataract surgery.
1. INTRODUCTION
The Argentinian Flag Sign (AFS) refers to a blue and white striped pattern recalling the national flag of Argentina, which may be observed after indocyanine green or trypan blue staining during cataract and refractive surgeries [1]. The appearance of the AFS is indicative of radial tearing of the anterior capsule following the initial puncture, and careful management during surgery is required to prevent an adverse outcome for visual acuity. Indeed, the appearance of the AFS is considered to present a great challenge to the ocular surgeon [1, 2]. AFS occurrence is greatly influenced by age, affecting 3.85% to 28.3% of patients in the 1-3 year age group [3, 4]; it is also more commonly associated with patients who have a history of vitrectomy and silicone oil use. There have been reports that trypan blue staining of the diabetic eye may also be a factor. There is a great deal of debate and controversy surrounding the choice of surgical approach to prevent the appearance of the AFS or minimize damage following its appearance [2, 5-14]. The current study has presented three cases where the AFS has been observed and correlated this phenomenon with surgical techniques and patient characteristics. Insights into the AFS as a visual indicator of intraoperative conditions or complications are provided.
2. CASE REPORTS
2.1. Case 1
A 47-year-old female presented with a 2-month history of progressive vision loss in her right eye. She had a history of severe myopia and had undergone vitrectomy, retinal detachment restoration, and silicone oil injection at a different hospital 8 months previously with the removal of the silicone oil a few months later. She had visual acuity of manual/20cm in the right eye and 0.05 in the left eye. Correction led to no improvement in visual acuity in the right eye and exhibited -11.75DS/-1.50DCX167=0.8 in the left. Intraocular Pressure (IOP) was within the normal limits. The right eye showed a deep anterior chamber with emulsified silicone oil vesicles visible above, a dilated pupil with a milky cloudy lens and liquefied, swollen cortex, and no evidence of intraocular entry. Auxiliary examinations showed no significant abnormalities. A preliminary diagnosis was made of concurrent cataract, postoperative retinal detachment, and postoperative silicone oil removal in the right eye with severe myopia in both eyes. Cataract surgery was performed with indocyanine green staining of the anterior capsule membrane. The capsule needle was cut off immediately; it made contact with the anterior capsule and the AFS was observed. The emulsified cortex was extracted via an incision of the anterior capsule membrane using capsule forceps to complete two semicircular tearing motions. Ultrasonic emulsification aspiration was performed, which revealed residual large silicone oil bubbles in the vitreous body, an intact posterior capsule membrane, and a cloudy lens. An intraocular lens (IOL, Zeiss 509M) was implanted with the IOL long axis aligned with the anterior capsule radial direction of the tear. The surgical procedure is illustrated in Fig. (1). One month after the operation, an examination of the dilated pupil showed the torn anterior membrane capsule edge with the IOL located in a stable position in the capsule bag and the cloudy posterior capsule (Fig. 2). Nd:YAG laser incision of the right eye posterior capsule membrane was made. The patient's visual acuity was 0.2 for the naked eye and -3.50DS/-1.00DCX10=0.5 with correction.
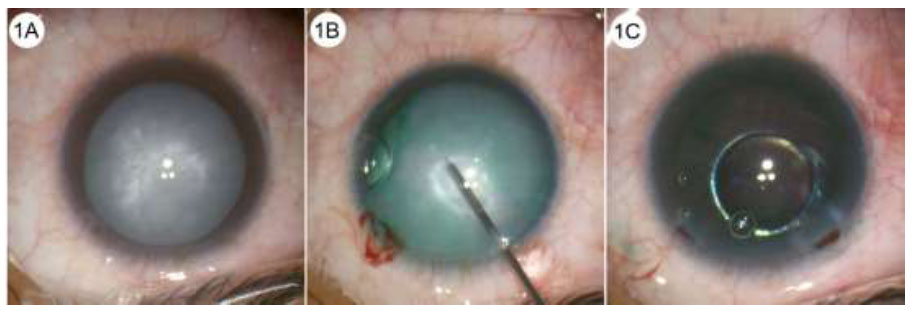
Case 1: Intraoperative screenshot. (A): The patient had a pre-operative clear cornea, emulsified silicone oil droplets in the anterior chamber, distended crystals, milky cloudiness, and cortical liquefaction. (B): Indocyanine green staining showed the anterior capsule to be split on puncture at the main incision and the Argentinian flag sign was visible. (C): Ultrasonography showed the posterior capsule to be intact and residual silicone oil bubbles could be seen in the vitreous body.
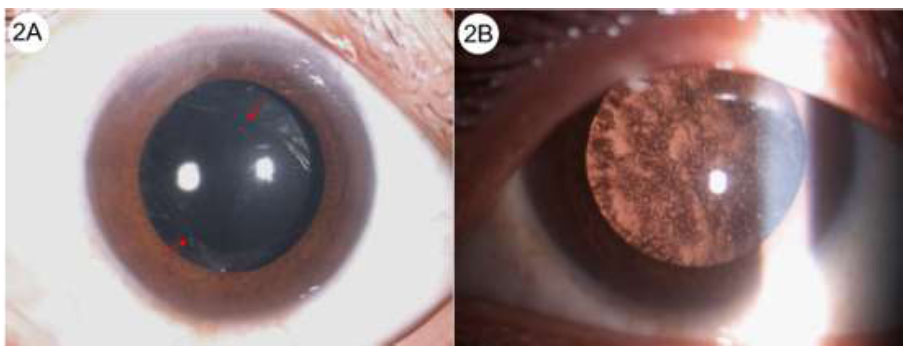
Case 1: (A): 1-week postoperative images. The anterior segment showing a clear cornea with a “shuttle” opening of the anterior capsule (red arrow) and the IOL located in the capsule bag. (B): Posterior right eye segment with pearly clouding of the posterior capsule.
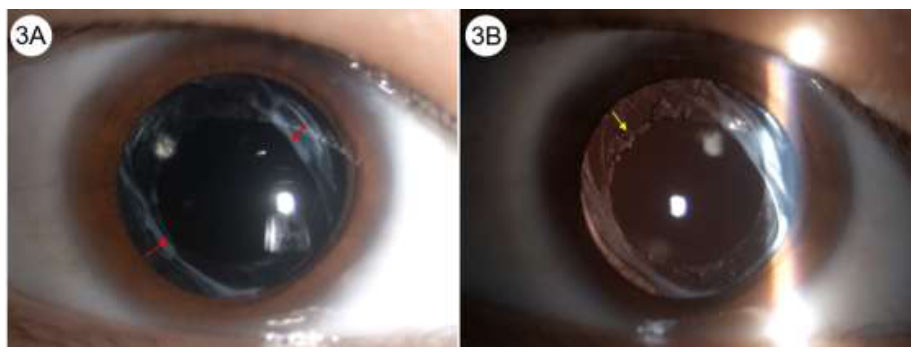
Case 2: Six-month postoperative images. (A): Anterior segment with clear cornea and “pike-shaped” cleavage of the anterior capsule (red arrow). The IOL is located in the capsular bag. (B): The posterior photograph showing the pike-shaped cleavage of the anterior capsule and the YAG incision of the posterior capsule (yellow arrow). The IOL can be seen to be correctly located.
2.2. Case 2
A 26-year-old female presented with a three-month history of decreased vision in her right eye. She had severe myopia (right eye: -8.00, left eye: -7.25) and had undergone vitrectomy, retinal detachment restoration, and silicone oil injection in the right eye two years previously with 5-month post-operative removal of silicone oil. Manual/optical (Vod) assessment of visual acuity on admission gave a value of 0.8 for the left eye (Vos). IOP was within normal limits. The right eye had a deep and clear anterior chamber with dilated pupil examination showing white clouding, emulsification, and swelling of the cortex. Fundus examination did not reveal any abnormalities, and no anomalies were seen in the left eye. Intraoperative staining of the anterior capsule with indocyanine green revealed the AFS on the anterior capsule puncture with tearing forceps. The anterior capsule was trimmed with capsule scissors and ultrasonic emulsification surgery was completed. The vitreous body had a silicone oil vesicle with residual parietal pressure on the posterior capsule. An IOL (Zeiss 509M) was implanted in the capsule bag. Nd:YAG laser incision of the posterior capsulorhexis was performed after 1 month of postoperative stabilization. The visual acuity of the naked right eye was 0.15 at the last follow-up and the corrected visual acuity was -2.75DS/-0.75DCX180=0.6. A dilated right eye pupil examination showed a torn capsular border, partially machined capsular membrane, and IOL located in the capsule bag (Fig. 3).
2.3. Case 3
A 57-year-old male was admitted with left eye vision loss persisting for more than 2 months. He had severe myopia (right eye: -14.00, left eye: -12.50). He had undergone vitrectomy, retinal detachment restoration, and silicone oil injection in his left eye at a different hospital 18 months previously with the oil left in place post-operation. Admission examination showed Vod: manual/in front of the eye and Vos: 0.3 (sc). IOP was normal. The right anterior chamber of the eye was deep and clear, and dilated pupil examination showed white clouding, emulsified swelling of the cortex, and no fundus entry. The status of retinal healing was unknown and cataract surgery was performed to allow inspection of the retina. Radial tearing of the anterior capsule occurred during cataract surgery with the direction of cleavage almost parallel to the corneal tunnel. The AFS was observed. Ultrasonic emulsification was successfully completed, and the capsular bag was implanted with an IOL (Zeiss 509M), which occupied a stable position.
3. DISCUSSION
Cortical liquefaction and high capsular pressure are challenges in the control of the trajectory of capsule tearing, and radial tears of the anterior capsule membrane often occur. Balyan's capsule-tearing difficulty grading system assesses this procedure at the highest level of difficulty [1]. Staining of the radial tears of the anterior capsule gives a distinctive pattern, which has been described as resembling the Argentinian flag by Perrone in 2000, and is designated the “Argentinian flag sign” [2]. This phenomenon primarily manifests during the initial puncture of the anterior capsule and has been reported to have an incidence of 3.85% to 28.3% among patients aged 1 to 3 years [3, 4]. AFS occurrence is influenced by age, corticosteroid use, ocular trauma, and post-vitrectomy or injection surgeries [3, 4]. Radial tearing of the anterior capsule in cataracts has been attributed to elevated vitreous pressure [5], but Figueiredo et al. have highlighted the impact of intra-capsular pressure dynamics [6]. These authors have suggested that progressive cortical emulsification increases the pressure within the capsular bag, which drops on cortical aspiration, while pressure in the posterior space rises. The resulting pressure imbalance promotes tearing, resulting in the visualization of the AFS. Irregular, uncontrolled tears may escalate to severe complications, such as nucleus loss, IOL implantation failure, iris damage, retinal detachment, and choroidal hemorrhage [7], with a significant impact on postoperative visual acuity.
A range of approaches have been implemented to mitigate radial tearing, including segmental capsule tearing [6], separate incision puncture using a 30G needle [1], intraoperative use of high-viscosity viscoelastic agents [8], ultrasonic anterior capsule techniques [2], sewing-needle methods [9], Zepto pulsed anterior capsule membrane dissection [10], and preoperative Nd:YAG laser dissection of the anterior capsule to release emulsified cortex [11]. These approaches have been reviewed earlier [14]. The use of such methods has emphasized the importance of maintaining high, stable anterior chamber pressure to prevent pressure differentials and intraoperative release of the emulsified cortex in order to alleviate pressure imbalances caused by lens nucleus obstruction.
The current authors have previously achieved successful results from cataract surgery by staining the anterior capsule with indocyanine green and performing side incision, skin test needle puncture, and partial cortex extraction prior to capsule tearing. Rapid radial tearing was not observed perhaps due to the patient's relatively young age (47 years), and early-stage cataracts with high capsular pressure from cortical emulsification resulted from vitrectomy and silicone oil presence [12, 13]. In addition, the patient had a “watery eye” with inadequate release of atrial fluid before viscosuppository injection, and improper puncture needle usage may have placed uneven stress on the anterior capsule [12, 13, 15, 16].
CONCLUSION
In conclusion, careful preoperative assessment of expanding cataracts is crucial to inform the choice of surgical treatment, particularly after vitrectomy and in younger patients. Evaluation of the capsular bag is essential to prevent severe complications arising from radial tearing.
AUTHORS’ CONTRIBUTION
All the authors have accepted responsibility for the manuscript's content and consented to its submission. All of them have meticulously reviewed the results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| AFS | = Argentinian Flag Sign |
| IOL | = Intraocular Lens |
| IOP | = Intraocular Pressure |
ETHICAL STATEMENT
This study was approved by Zhejiang Medical and Health Group Qu Zhou Hospital, Ethics (Approval No. 2024-10).


