All published articles of this journal are available on ScienceDirect.
Comparative Analysis of Three Surgical Approaches for Managing Convergence Insufficiency Intermittent Exotropia in Pediatric Patients
Abstract
Introduction
This study compared three surgical approaches for convergence insufficiency intermittent exotropia (CI-X[T]) in children to identify the most effective method.
Methods
Fifty-eight children aged 4–13 years with CI-X(T) and near-distance disparity ≥10 prism diopters (PD) were prospectively randomized to: (1) Bilateral Lateral Rectus Recession (BLR), (2) Unilateral Recession–Resection (RR), or (3) Medial Rectus Resection (MRR). Surgical outcomes were defined as postoperative deviation within 5 PD of esophoria/tropia and 10 PD of exophoria/tropia. Patients were followed for 24 months.
Results
At the final follow-up, cumulative success rates were similar among BLR (52.4% near, 81.0% at distance), RR (30.4% near, 43.5% at distance), and MRR (27.3% near, 50.0% at distance). Near exodeviation decreased significantly in all groups (p < 0.001). NDD correction was achieved in 59.1% of MRR, 50.0% of BLR, and 30.4% of RR patients (p = 0.142). Stereopsis improved comparably across groups. Complications included overcorrection and A/V patterns in BLR, undercorrection in RR, and persistent consecutive esotropia in MRR.
Discussion
All three surgical approaches were effective, with BLR favoring distance correction, RR showing short-term near benefits, and MRR demonstrating balanced long-term outcomes, including improvement in the AC/A ratio.
Conclusion
MRR appears to be the most reliable overall, although individual patient characteristics should guide surgical choice. Larger, long-term studies are needed.
1. INTRODUCTION
Convergence Insufficiency Intermittent Exotropia (CI-X(T)) is characterized by an exodeviation of at least 10 prism diopters (PD) that is greater at near fixation than at distance, a condition increasingly diagnosed in children due to the rise in electronic device usage [1]. This condition is often accompanied by symptoms such as eye strain, fatigue, and blurred vision, which significantly impact daily activities. The success rate of surgical interventions for CI-X(T) varies considerably, ranging from 18% to 92%, prompting ongoing exploration of more effective surgical strategies [2].
Many surgical treatments may be used to manage CI-X(T). These include slanting operations, adjustable sutures, bilateral LR recession, unilateral MR resection, conventional unilateral LR recession with MR resection, and unilateral or bilateral MR resection [3]. While some surgeons advocate for bilateral LR recession in CI-X(T) treatment, others prefer a more tailored approach, such as unilateral MR resection based on near deviation and LR recession based on distance deviation [4].
One notable technique, proposed by Kraft et al. (1995), is the improved unilateral recession-resection, which involves adjusting the MR resection and LR recession based on near and distance measurements, respectively. This technique has been suggested to provide a balanced correction of near and distance deviations while minimizing postoperative complications, such as consecutive esotropia [5].
Despite these various surgical approaches, there is no consensus on the optimal procedure for treating CI-X(T). This study aims to prospectively compare the outcomes of three surgical techniques, bilateral LR recession (BLR), unilateral MR resection with LR recession (URR), and MR resection (MRR), to determine the most effective strategy for managing this challenging condition.
2. PATIENTS AND METHODS
Between June 2018 and April 2020, 58 consecutive patients with CI-X(T) participated in this prospective study. Parents or guardians of the pediatric patients gave their informed written consent before surgery, as per the protocol approved by the Hospital's Medical Ethics Committee for the protection of human subjects (Declaration of Helsinki). Participants were included in the study if, following 45 minutes of monocular patching, their CI-X(T) (near XT that exceeds distant XT by ≥ 10 PD) was confirmed at least twice, two weeks apart. The minimum age for inclusion was 4 years, and the maximum was 13 years. The study excluded patients with congenital abnormalities, neurological disorders, A or V pattern, paralytic or restrictive strabismus, amblyopia, oblique muscle overaction, or a history of prior strabismus surgeries. We collected a thorough medical history from each patient, including the age at which the deviation began and the duration of the condition. Exodeviation for 100% of waking hours was referred to as constant deviation. Anterior segment, fundus, motility, cycloplegic refraction, and best corrected visual acuity were among the comprehensive ophthalmic and orthoptic examinations that followed. Glasses that were approximately 1.00 to 1.50 D less than their full cycloplegic hyperopic refraction were given to patients with hyperopia, full astigmatic correction, and overcorrected myopic correction by 0.5 to 1.00 D, respectively.
X(T) was classified using Burian's classification system [6], which distinguishes between near and distant deviations after monocular occlusion, and this investigation only included the CI-X(T) type. Using the CI-X(T) classification method developed by Yang and Hwang, eleven patients were further grouped based on their responses to monocular occlusion tests. The research comprised individuals with masked CI-X(T), genuine CI-X(T), or close X(T), distant X(T) by more than 10 PD before and after monocular occlusion. Patients who had pseudo-CI-X(T), close X(T)> distant X(T) by more than 10 PD just before the monocular occlusion test but not thereafter were not included in the research. The gradient approach was used to obtain the AC/A ratio. To begin, we assessed fusion using the standard four-dot test. We then measured near stereoacuity in the present refractive correction using the Titmus fly stereotest; a value of 100 seconds of arc was deemed satisfactory. Following surgery, an improvement in stereopsis was defined as a reduction of at least 2 octaves at the last follow-up session or before reoperation. In contrast, deterioration was defined as an increase of at least two octaves. In cases of close or far postoperative overcorrection, patients were informed before surgery that prism treatment or a temporary alternative patching method would be necessary. A variety of surgical procedures are used to treat each patient.
After 45 minutes of monocular occlusion at distant and close fixation, the most significant preoperative deviation assessed by PACT was the amount of deviation for which surgery was completed. Using a small incision in the conjunctiva, the author (AS) and an assistant performed the procedures on the same operating table while under general anesthesia. The LR recession was measured after disinsertion and direct suturing to the globe from the back of the muscle's insertion. The diameter of the target muscle was measured at its place of insertion before dissection from the insertion. The muscle was reinserted near its initial insertion for LR recession recessed by distant exodeviation (range: 6–11 mm). An orthoptist, disguised as a surgeon, conducted postoperative examinations planned for one week, one month, three months, six months, and twelve months after the procedure. They included the Titmus stereotest and alignment in the primary position, as well as close and far away. Only at the final follow-up visit was the AC/A ratio evaluated postoperatively. A postoperative residual deviation at near and distance between 5 PD of esophoria/esotropia and 10 PD of exophoria/exotropia, with a near-distance difference of 10 PD, was considered a successful outcome. Initial postoperative consecutive esotropia ranged from 10 to 20 PD.
2.1. Statistical Analysis
The sample size (N = 58) was calculated to detect a 20% difference in success rates (80% power, α = 0.05). ANOVA was used to compare success rates and exodeviation changes across groups, with Tukey’s post-hoc tests for pairwise comparisons. p < 0.05 was considered significant. Effect sizes (Cohen’s d) were calculated to determine the magnitude of the observed differences.”
3. RESULTS
A total of 58 children who satisfied the inclusion criteria were split into three groups during the study period: the BLR group, which included 22 patients (37.9 percent), the RR group, which included 23 patients (39.7 percent), and the MRR group, which included 13 patients (22.4 percent). Outward deviation affected all 58 patients in our patient cohort, while photophobia affected 14, and diplopia affected 11. None of the patients wore prism glasses before surgery. The angle of deviation and symptoms remained unaffected by the attempt to increase fusional convergence amplitude in 37 patients through push-up training. The preoperative patient characteristics are displayed in Table 1 and did not differ significantly between the three groups. Tables 2, 3, and 4 display the cumulative odds of success, undercorrections, and overcorrections for each of the three groups. The angle of deviation is shown in Fig. (1) along with the average of near exodeviation, distant exodeviation, and near-distant disparity before surgery and at each postoperative follow-up visit. One year following surgery, there was no statistically significant difference between the groups' cumulative odds of success at near fixation, distant fixation, and NDD (p-value = 0.054, 0.233, and 0.142, respectively).
| Characteristics, mean ± SD. | BLR (n=22) | RR (n=23) | MRR (n=13) | p-value |
|---|---|---|---|---|
|
Age at time of surgery (in years, mean±SD) |
13.9 ± 12.56 | 17.0 ± 12.1 | 15.8 ± 7.1 | 0.865a |
| Gender: Male, n (%) Female, n(%) |
12 (70.0%) 5(31.8%) |
11 (50.0%) 10(47.8%) |
15 (77.1%) 5(23.1%) |
0.08b |
| Refractive error in the right eye (OD), spherical equivalent (S.E.; diopters, D) mean±SD | − 0.38 ± 1.1 | - 1.1 ± 2.0 | − -0.7 ± 1.8 | 0.186a |
| Refractive error in the left eye (OS), spherical equivalent (S.E.; diopters, D) mean±SD | 0.25 ± 1.3 | -1.0 ± 2.0 | 0.4 ± 1.8 | 0.168a |
| Best corrected visual acuity (BCVA) in the right eye (OD), logMAR, mean±SD | 1.10 ± 0.29 | 0.92 ± 0.12 | 1.02 ± 0.28 | 0.122a |
| Best corrected visual acuity (BCVA) in the right eye (OD), logMAR) mean±SD | 1.05 ± 0.35 | 0.99 ± 0.27 | 1.00 ± 0.33 | 0.878a |
| Distance exotropia (in prism diopters, ∆) mean±SD | 29.1 ± 11.3 | 34.2 ± 16.5 | 24.1 ± 10.6 | 0.052a |
| Near exotropia (in prism diopters, ∆) mean±SD | 47.0 ± 14.0 | 46.2 ± 16.2 | 37.8 ± 10.3 | 0.053a |
| Difference in close-distance measurements (in prism diopters, ∆) mean±SD | 17.0 ± 8.2 | 12.5 ± 7.6 | 13.3 ± 7.1 | 0.056a |
| functional stereopsis preoperatively n(%) | 10/22 (45.5%) | 14/24 (58.3%) | 13/22 (59.1%) | 0.527b |
| functional stereopsis postoperatively n(%) | 15/23 (65.2%) | 19/25 (76.0%) | 17/22 (77.3%) | 0.470b |
| Progression in stereopsis after surgery (%) | 9/22 (40.9%) | 12/23 (52.2%) | 13/22 (59.1%) | 0.302b |
| Stability in stereopsis after surgery (%) | 8/22 (36.4%) | 9/23 (39.1%) | 6/22 (27.3%) | 0.693b |
| Degradation in stereopsis after surgery (%) | 7/23 (30.4%) | 2/23 (8.7%) | 3/22 (13.6%) | 0.105b |
| Persistence of ocular deviation postoperatively n(%) | 9/22 (40.9%) | 11/13 (84.6%) | 5/12 (41.7%) | 0.000b,c |
| Preoperative accommodative convergence/accommodation (AC/A) ratio mean±SD | 1.80 ± 0.88 | 1.90 ± 0.52 | 2.10 ± 0.39 | 0.189a |
| postoperative accommodative convergence/accommodation (AC/A) ratio mean±SD | 2.05 ± 1.80 | 2.65 ± 0.82 | 2.07 ± 0.53 | 0.214a |
| Primary undercorrection in distant vision (%) | 7/21 (33.3%) | 14/23 (60.9%) | 0/21 | 0.000b,c |
| Primary undercorrection in near vision (%) | 12/21 (57.1%) | 12/13 (61.5%) | 4/11 (36.4%) | 0.009b,c |
| Final undercorrection in distant vision (%) | 6/21 (28.6%) | 13/23 (56.5%) | 5/21 (23.8%) | 0.021b,c |
| Final undercorrection in near vision (%) | 11/21 (52.4%) | 16/23 (69.6%) | 15/21 (71.4%) | 0.233b |
| Primary overcorrection in distant vision (%) | 4/21 (19.0%) | 0/23 (0%) | 8/21 (38.1%) | 0.007b,c |
| Primary overcorrection in near vision | 0/21 | 0/23 | 0/21 | N/A |
| Final overcorrection in distant vision | 0/22 | 0/23 | 6/21 (28.6%) | 0.001b,c |
| Final overcorrection in near vision | 0/21 | 0/23 | 0/21 | N/A |
| Group | Surgical Outcome | 1 Day | 1 Month | 3 Months | 6 Months | 12 Months |
|---|---|---|---|---|---|---|
| BLR (n = 22) | Successful Outcome | 9/21 (42.9%) | 9/21 (42.9%) | 9/21 (42.9%) | 14/21 (66.7%) | 17/21 (81.0%) |
| - | Incomplete Correction | 8/21 (38.1%) | 5/21 (23.8%) | 4/21 (19.0%) | 4/21 (19.0%) | 5/21 (23.8%) |
| - | Excessive Correction | 4/21 (19.0%) | 7/21 (33.3%) | 8/21 (38.1%) | 3/21 (14.3%) | 0/21 (0%) |
| RR (n = 23) | Successful Outcome | 9/23 (39.1%) | 8/23 (34.8%) | 9/23 (39.1%) | 8/23 (34.8%) | 10/23 (43.5%) |
| - | Incomplete Correction | 14/23 (60.9%) | 14/23 (60.9%) | 14/23 (60.9%) | 15/23 (65.2%) | 13/23 (56.5%) |
| - | Excessive Correction | 0/23 | 1/23 (4.3%) | 0/23 | 0/23 | 0/23 |
| MRR (n = 22) | Successful Outcome | 13/22 (59.1%) | 17/22 (77.3%) | 16/22 (72.7%) | 11/22 (50.0%) | 11/22 (50.0%) |
| - | Incomplete Correction | 0/22 | 0/22 | 0/22 | 5/22 (22.7%) | 5/22 (22.7%) |
| - | Excessive Correction | 9/22 (40.9%) | 5/22 (22.7%) | 6/22 (27.3%) | 6/22 (27.3%) | 6/22 (27.3%) |
| p-value of Successful Outcome Rate | BLR vs RR | 0.903 | 0.671 | 0.903 | 0.055 | 0.021a |
| - | BLR vs A-BLR | 0.136 | 0.005a | 0.035a | 0.368 | 0.063 |
| - | RR vs MRR | 0.104 | 0.001a | 0.025a | 0.304 | 0.66 |
| Group | Surgical Outcome | 1 Day | 1 Month | 3 Months | 6 Months | 12 Months |
|---|---|---|---|---|---|---|
| BLR (n = 22) | Successful Outcome | 9/21 (42.9%) | 9/21 (42.9%) | 12/22 (54.5%) | 9/21 (42.9%) | 11/21 (52.4%) |
| - | Incomplete Correction | 13/22 (59.1%) | 13/22 (59.1%) | 10/22 (45.5%) | 13/22 (59.1%) | 11/22 (52.4%) |
| - | Excessive Correction | 0/22 | 0/22 | 0/22 | 0/22 | 0/22 |
| RR (n = 23) | Successful Outcome | 10/23 (43.5%) | 8/23 (34.8%) | 16/23 (69.6%) | 6/23 (26.1%) | 7/23 (30.4%) |
| - | Incomplete Correction | 13/23 (56.5%) | 15/23 (65.2%) | 7/23 (30.4%) | 17/23 (73.9%) | 16/23 (69.6%) |
| - | Excessive Correction | 0/23 | 0/23 | 0/23 | 0/23 | 0/23 |
| MRR (n = 22) | Successful Outcome | 17/22 (77.3%) | 12/21 (57.1%) | 10/22 (45.5%) | 9/21 (42.9%) | 5/22 (22.7%) |
| - | Incomplete Correction | 4/21 (19.0%) | 8/22 (36.4%) | 11/22 (50.0%) | 12/23 (52.2%) | 15/22 (68.2%) |
| - | Excessive Correction | 0/22 | 0/22 | 0/22 | 0/22 | 0/22 |
| p-value of Success Rate | BLR vs RR | 0.857 | 0.674 | 0.906 | 0.298 | 0.183 |
| - | BLR vs A-BLR | 0.004a | 0.004a | 0.034a | 0.374 | 0.123 |
| - | RR vs MRR | 0.009a | 0.003a | 0.026a | 0.064 | 0.812 |
| Group | Surgical Outcome | 1 Day | 1 Month | 3 Months | 6 Months | 12 Months |
|---|---|---|---|---|---|---|
| BLR (n = 22) | Successful outcome | 14/22 (63.6%) | 9/22 (40.9%) | 9/22 (40.9%) | 9/22 (40.9%) | 13/22 (59.1%) |
| RR (n = 23) | Successful outcome | 23/23 (100%) | 16/23 (69.6%) | 8/23 (34.8%) | 8/23 (34.8%) | 7/23 (30.4%) |
| MRR (n = 22) | Successful outcome | 18/22 (81.8%) | 13/22 (59.1%) | 17/22 (77.3%) | 15/22 (68.2%) | 11/22 (50.0%) |
| p-value of the Successful Outcome Rate | BLR vs RR | 0.001a | 0.056 | 0.671 | 0.671 | 0.055 |
| - | BLR vs MRR | 0.18 | 0.232 | 0.015a | 0.015a | 0.549 |
| - | RR vs MRR | 0.034a | 0.47 | 0.004a | 0.004a | 0.184 |
3.1. Near Exodeviation and Near-distant Disparity
Following surgery, all three groups showed a significant decrease in the mean near exodeviation (p<0.001, paired t-test). The cumulative probability of exodeviation success at near fixation at the last visit was 52.4% for the BLR, 30.4% for the RR, and 27.3% for the MRR groups. This difference was not statistically significant (p=0.233; Fig. 1A). Notably, none of the three groups experienced postoperative overcorrection at near fixation.
Following surgery, the mean near-distant disparity was not significant in the RR group (p=0.148), but it was significantly reduced in the BLR and MRR groups (p=0.002, 0.007, respectively) (Fig. 1B). The MRR, RR, and BLR groups had cumulative probabilities of success in correcting NDD at the last postoperative visit of 59.1%, 30.4%, and 50%, respectively. This difference was deemed statistically insignificant (p=0.142; Fig. 1C).
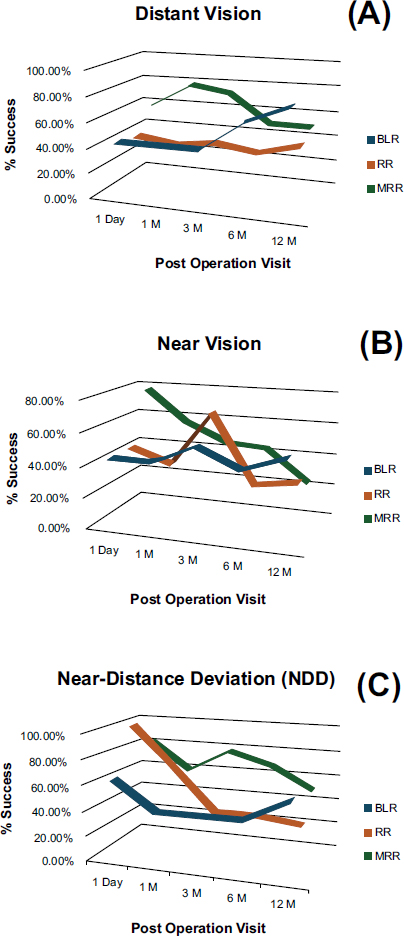
Comparison of the postoperative success rates of three distinct surgical approaches for treating convergence insufficiency intermittent exotropia.
The mean near stereoacuity and AC/A ratio increased from 60.9±13.3 to 82.7±17.7 and 67.5±27.5 arc sec, respectively, in the BLR, RR, and MRR groups before and after surgery, with values of 59.9±14.6, 46.6±11.5 arc sec, and 36.2±12.1 arc sec. A comparison of the three groups' rates of enhanced stereopsis (p=0.302), stationary stereopsis (p=0.693), and reduced stereopsis (p=0.105) revealed no statistically significant difference (Table 1).
The average AC/A ratio was 3.4±2.7, and 34 out of the 58 individuals included in this research had a normal ratio.
3.2. Complications
Four patients (18.1% of the BLR group) exhibited downgaze “V-pattern” overcorrection at the last postoperative appointment. On average, the deviations after the operation were 3.5±5.2 PD XT in downgaze, 8.7±4.2 PD XT in upgaze, and 8.3±6.1 PD ET in the leading position. A different example (4.5 percent) in the same group also showed a notable postoperative A-pattern, with downgaze measuring 16.2±5.2 PD XT, upgaze measuring 4.2±2.8 PD XT, and leading position measuring 4.4±4.1 PD XT, respectively. Since no diplopia was seen in any of those individuals with an asymptomatic A-V pattern, further therapy was unnecessary. Patients whose cases included distant early postoperative overcorrection received appropriate treatment and therapy (Tables 2, 3, and 4).
Until the diplopia subsided, complete cycloplegic hypermetropic correction and alternating full-time patching were administered to those patients. Temporary Fresnel press-on prisms were used to treat cases of non-revolving consecutive esotropia (46 PD) and diplopia in the BLR group on 8/21 (36.3 percent), RR on 1/23 (4.3 percent), and MRR on 4/21 (18.1 percent) after a month. At six months after surgery, the base-out prisms were weaned off in all cases of persistent consecutive esotropia, with 5/22 (22.7 percent) in the BLR group and 7/22 (31.8 percent) in the MRR group having PD values less than 15 (mean 6.0±2.5 PD). All instances of successive esotropia in the BLR and RR groups showed complete resolution, unlike 7/22 cases (31.8%) in the MRR group, who still had it at the most recent follow-up visit.
4. DISCUSSION
Deficit in Convergence. As screen time continues to rise, more children suffer from intermittent glare, also known as intermittent exotropia (CI-X(T)). The management of CI-X(T) remains controversial, with various surgical techniques proposed to address the different characteristics of this condition. This study aimed to compare the efficacy of three common surgical approaches: Bilateral Lateral Rectus (BLR) recession, Unilateral Recession–Resection (RR), and Modified Recession–Resection (MRR) in terms of correcting both near and distant exodeviations and near-distant disparity (NDD).
Our findings provide important insights into the efficacy of these techniques. The BLR group showed a significant improvement in distant exodeviation correction, with a success rate of 77.1% at 12 months. However, this technique was associated with a higher incidence of postoperative overcorrection and the development of A-V patterns, which persisted throughout the follow-up period. These results align with previous studies by Tu Y et al. that noted the tendency for BLR recession to result in overcorrection, especially in patients with larger preoperative deviations [7]. Furthermore, while BLR may effectively address distant exodeviations, its associated complications often necessitate careful postoperative management [8].
The RR group showed more moderate results, with a success rate of 43.4% for distant exodeviation correction at 12 months. The RR technique exhibited a higher rate of undercorrection, with 56.5% of patients still experiencing undercorrection at 12 months. These results are consistent with previous reports that have indicated a tendency for undercorrection when unilateral techniques such as MR resection combined with LR recession are employed [8]. Despite this, the RR group demonstrated a significant improvement in near exodeviation correction at 3 months (69.5%), although this improvement diminished over time (30.4% at 12 months). This suggests that RR may offer more short-term benefits in correcting near deviation, though its long-term effectiveness in correcting both near and distant exodeviations may be less robust.
These findings are consistent with Farid and Abdelbaset (2018), who reported similar success rates for the RR technique in CI-X(T) [4].
The MRR group showed the most favorable outcomes, achieving an 81.8% success rate at 1 month for distant exodeviation correction, which gradually decreased to 50% by 12 months. Although this decline in success rates over time was observed, the MRR group maintained the most consistent and stable results compared to BLR and RR. Notably, the MRR technique demonstrated the only significant improvement in the AC/A ratio, a critical factor in managing associated convergence insufficiency. These results align with those reported by Kraft et al. (1995), who introduced an improved version of the unilateral recession–resection procedure tailored to treat CI-X(T) and reported similar successes in near and distant exodeviation corrections [5].
Regarding NDD, the MRR group had the highest cumulative probability of success in reducing NDD at 12 months (59.09%), followed by the BLR group (50%) and the RR group (30.4%). However, the difference between the groups was not statistically significant (p = 0.142), suggesting that all three surgical techniques have comparable efficacy in addressing NDD. These findings are consistent with studies by [9], which showed similar success rates among different surgical approaches for correcting NDD. Although MRR showed a trend toward greater success in achieving this outcome, it should be noted that the differences were not clinically significant.
In terms of postoperative complications, none of the three surgical approaches resulted in permanent postoperative diplopia at near fixation, and there was no persistent overcorrection at near fixation, a common complication in traditional surgical treatments for intermittent exotropia [9]. These results highlight the potential benefits of these surgical approaches in reducing postoperative complications, which could otherwise affect patients' quality of life. Cycloplegic correction and alternate full-time patching effectively addressed early postoperative overcorrection and consecutive esotropia. Additionally, Fresnel press-on prisms helped manage cases of non-revolving consecutive esotropia, particularly in the BLR and MRR groups. These findings are consistent with what was noted by Liang et al., who found that adjunctive measures are critical for managing postoperative overcorrection [10].
5. STUDY LIMITATIONS
Although randomization was mentioned, the details of the method and whether it was effectively blinded were not fully explained. Only 58 patients were included, which limits the generalizability of the findings and makes it difficult to detect minor differences between groups. Notably, despite its valuable insights, this research has a few shortcomings. The short 2-year follow-up period and small sample size make it difficult to determine how well these surgical techniques performed over the long term. Larger-scale studies with more extended follow-up periods are necessary to evaluate the sustained effectiveness of these interventions. Additionally, the absence of subjective visual function assessments and a control group limits our ability to draw definitive conclusions regarding the functional benefits of these surgical techniques.
CONCLUSION
This study suggests that MRR is the most effective surgical technique for managing CI-X(T), providing favorable outcomes in both near and distant exodeviation correction. The method also offers advantages in improving the AC/A ratio, which is particularly beneficial for patients with associated convergence insufficiency. Although all three surgical approaches showed comparable efficacy in reducing NDD, MRR exhibited the highest success rates. Given the relatively low incidence of postoperative complications such as overcorrection and A-V patterns, the MRR technique offers a reliable and practical option for the surgical treatment of CI-X(T). Further studies with larger sample sizes and longer follow-up are needed to confirm these findings and refine the management strategies for CI-X(T).
SUMMARY
Convergence Insufficiency Intermittent Exotropia (CI-X(T)) is increasingly recognized as a prevalent form of intermittent exodeviation, particularly in children, likely exacerbated by the increased usage of electronic devices in this demographic. The surgical management of CI-X(T) remains contentious, with varying opinions on the optimal approach. Unilateral recession-resection, specifically biased towards near and distant deviations, has shown moderate success among the options considered. Bilateral lateral rectus (LR) recession, although yielding favorable outcomes in cases with significant deviation at distance, is associated with a higher incidence of postoperative V and A patterns. Additionally, bilateral LR recession is linked to a substantial occurrence of consecutive postoperative diplopia and esotropia, which complicates the management of these patients. This study suggests that MRR is the most effective surgical technique for managing CI-X(T), providing favorable outcomes in both near and distant exodeviation correction. In contrast, while demonstrating moderate success in correcting distant exodeviation, the unilateral recession-resection technique has been linked to postoperative undercorrection in some cases. Despite this, the method has shown stability in treating distant exodeviation and moderate success in correcting near exodeviation, particularly when compared to bilateral LR recession. Moreover, this technique yielded significantly lower rates of postoperative overcorrection and offered improvements in the AC/A ratio, indicating its potential benefit in managing CI-X(T). Several factors, including the degree of preoperative deviation, binocular potential, and individual patient characteristics, influence the CI-X(T) treatment outcomes. Notably, patients with uniocular dominance, as well as those presenting with large preoperative angles of deviation, may experience distinct outcomes. These findings align with previous studies by Yang et al. 2024 which highlighted the multifactorial nature of treatment success in CI-X(T) management [11]. This study suggests that the improved unilateral recession-resection technique, with its moderate success rate, lower incidence of postoperative complications, and favorable impact on the AC/A ratio, represents a promising surgical option for managing CI-X(T) in pediatric populations. Further studies with larger cohorts and longer follow-up are necessary to confirm these findings and refine the CI-X(T) surgery approach.
FUTURE RESEARCH
Future studies should concentrate on long-term outcomes through extended follow-up periods (5–10 years) to evaluate alignment stability, recurrence rates, and sensory outcomes like stereopsis; optimize preoperative planning by integrating diagnostic monocular occlusion protocols. Assess combined approaches with non-surgical adjuncts like orthoptic exercises or prisms; examine the effect on myopic progression; and include patient-reported quality-of-life measures to capture subjective benefits.
AUTHORS’ CONTRIBUTIONS
The authors confirm contribution to the paper as follows: A.S.: The principal investigator and main author, was responsible for study conception and design, surgical procedures, data collection, statistical analysis, manuscript drafting, and overall supervision; K.G.: Contributed to patient recruitment, surgical assistance, and follow-up evaluations and participated in data interpretation and manuscript editing; A.E.: Assisted in the literature review, data organization, and contributed to the initial manuscript writing; M.H.: Assisted with data accuracy verification and figure preparation; A.A.K.: Provided statistical consultation and contributed to analysis validation; M.D.: Supported patient clinical assessments, documentation, and contributed to revisions of the manuscript; S.G.: Involved in ethics approval coordination, reference formatting, and manuscript proofreading; A.I.: Reviewed the final manuscript for intellectual content, provided critical revisions, and contributed to submission preparation. All authors have read and approved the final version of the manuscript and agree to be accountable for all aspects of the work.
LIST OF ABBREVIATIONS
| BLR | = Bilateral Lateral Rectus Recession |
| PD | = Prism Diopters |
| MRR | = Medial Rectus Resection |
| RR | = Unilateral Recession–Resection |
| NDD | = Near-distant Disparity |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was approved by the Ethics Committee of Magrabi Eye Hospital (Approval No: IRB approval from the Institutional Review Board (IRB), Faculty of Medicine, Al-Baha University, Saudi Arabia No.: IRB/SUR/BU-FM/2024/181.
HUMAN AND ANIMAL RIGHTS
All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
AVAILABILITY OF DATA AND MATERIALS
All the data and supporting information are provided within the article https://doi.org/10.5281/zenodo.17193742.
ACKNOWLEDGEMENTS
Declared none.


