RESEARCH ARTICLE
Transcutaneous Blepharoptosis Surgery: Simultaneous Advancement of the Levator Aponeurosis and Müller’s Muscle (Levator Resection)
Kazunami Noma1, Yasuhiro Takahashi2, Igal Leibovitch3, Hirohiko Kakizaki*, 2
Article Information
Identifiers and Pagination:
Year: 2010Volume: 4
First Page: 71
Last Page: 75
Publisher ID: TOOPHTJ-4-71
DOI: 10.2174/1874364101004010071
Article History:
Received Date: 15/4/2010Revision Received Date: 25/6/2010
Acceptance Date: 19/7/2010
Electronic publication date: 14/12/2010
Collection year: 2010

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
Transcutaneous blepharoptosis surgery with simultaneous advancement of the levator aponeurosis and Müller’s muscle (levator resection) is a popular surgery which is considered effective for all types of blepharoptosis except for the myogenic type. Repair of ptosis cases with good levator function yields excellent results. A good outcome can be also obtained in cases with poor levator function, however, in such cases; a large degree of levator advancement may be required, which may result in postoperative dry eyes, unnatural eyelid curvature and astigmatism. These cases are therefore better treated with sling surgery. With the right patient selection, the levator resection technique is an effective method for ptosis repair.
INTRODUCTION
Blepharoptosis surgery is one of the most popular operations in the field of ophthalmic plastic and reconstructive surgery. The specific surgical method for repairing blepharoptosis is selected according to the degree of eyelid droopiness and the preoperative levator function [1]. There are 3 categories of surgical approaches to blepharoptosis surgery; transcutaneous [2], transconjunctival [3] and sling surgery [4]. The transconjunctival approach is mainly used in cases of mild to moderate ptosis with a good response to the phenylephrine test [5]. The transcutaneous approach can be applied to all types of ptosis except for the myogenic type, in which sling surgery may be best suitable [6]. Ptosis cases with levator function of 4 mm or more are usually repaired by levator resection [1], whereas sling surgery is used in cases of levator function under 4 mm [7].
There are several techniques for blepharoptosis repair which are done through a transcutaneous incision; simultaneous advancement of the levator aponeurosis and Müller’s muscle (levator resection) [8], advancement of the aponeurosis only (lavatory advancement) [2] etc. The 2 transcutaneous techniques are widely performed, however, they are selected based on surgeons’ preferences and not based on the pathophysiology of ptosis or factors like levator function, degree of ptosis, or type of ptosis.
Müller’s muscle is believed to originate from the posterior surface of the levator palpebrae superioris (LPS) muscle [9]. More recently, modified anatomical findings regarding the origin of the levator aponeurosis and Müller’s muscle have been reported [10]. It was shown that the LPS muscle is divided into 2 branches in the periphery: the superior branch which continues to the levator aponeurosis, and the inferior branch from which Müller’s muscle originates. Although the thickness of each branch is almost identical, the superior branch tends to be thicker than the inferior branch.
Based on these new anatomical findings, the indications for ptosis surgery can theoretically be divided into the following categories:
- Aponeurotic ptosis- requires aponeurosis advancement.
- Cases of pathology in the Müller’s muscle (such as Horner’s syndrome) [9] - require Müller’s muscle advancement. However, as Müller’s muscle is structurally weak [11], simultaneous advancement of the levator aponeurosis is recommended.
- Ptosis in hard contact lens user [12] (and in rare cases in soft contact lens user [13]) - as the pathology is not purely in the aponeurosis but rather in both the aponeurosis and Müller’s muscle [14], levator resection is recommended.
- In cases of severe ptosis - levator resection or sling surgery should be performed. Although each procedure is effective irrespective of the associated pathology, comparative long term results have not been reported so far.
In this review, we present the levator resection technique and discuss the advantage and disadvantage.
THE SURGICAL TECHNIQUE
After marking a horizontal line along the upper skin crease extending to the lateral canthal commissure and about 6 to 7 mm from the upper eyelid margin, a local anesthetic solution (2 ml of 1% lidocaine with 1/100,000 epinephrine) is administered.
The skin is then incised with a number 15 blade. The subcutaneous tissue and the orbicularis oculi muscle are dissected with scissors, and the levator aponeurosis can then be visualized.
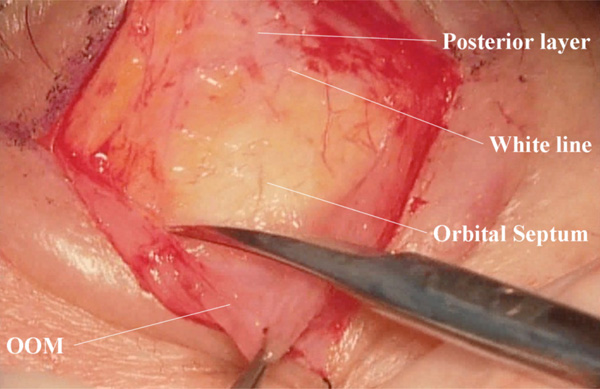
The levator aponeurosis is detached from the tarsal plate (Fig. 1), and the levator complex, including Müller’s muscle and the levator aponeurosis, are continuously detached from the conjunctiva (Fig. 2). Involutional change of the Müller’s muscle (thin appearance and/or fat infiltration, etc.) may be seen in some cases [15]. A negative phenylephrine test can be seen in patients with marked fatty infiltration [16].
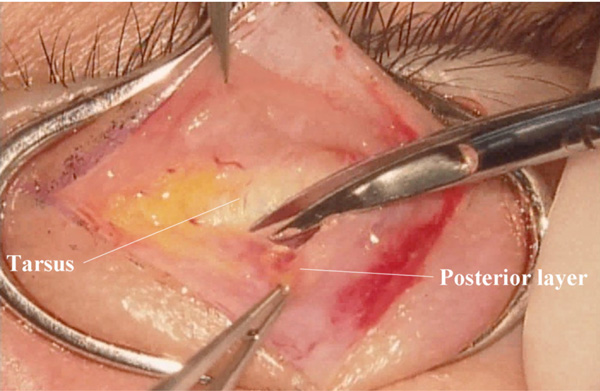 |
Fig. (1). (Upside down view: surgeon’s view) Detachment of the posterior layer of the levator aponeurosis from the tarsal plate. |
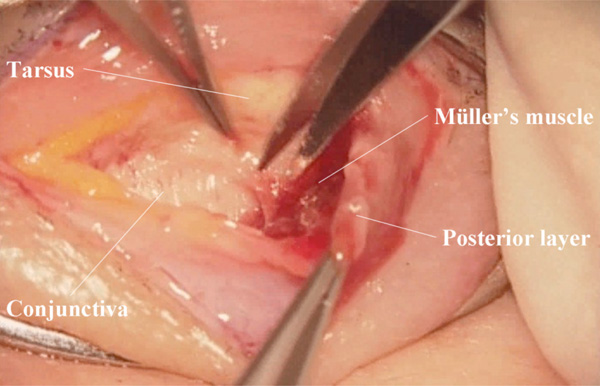 |
Fig. (2). (Surgeon’s view) Detachment of Müller’s muscle from the conjunctiva. |
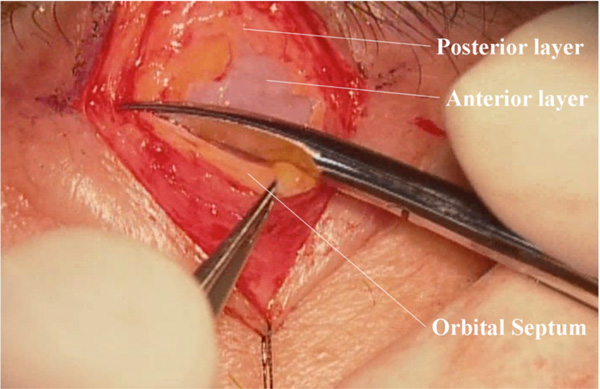 |
Fig. (4). (Surgeon’s view) Transverse incision of the orbital septum. The anterior layer of the levator aponeurosis is visualized. |
 |
Fig. (5A). Intraoperative quantification in the sitting position. Overcorrection is shown in the right side. |
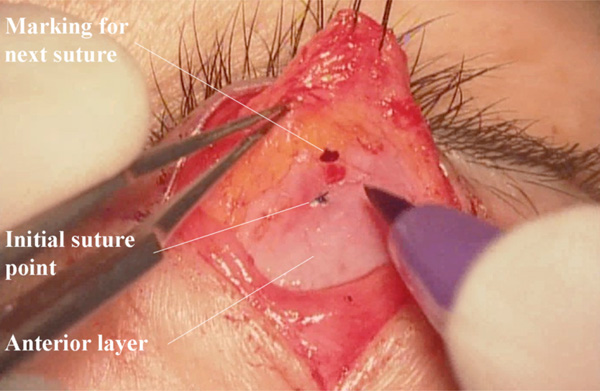 |
Fig. (5B). (Surgeon’s view) Re-fixation of the levator complex. The levator complex is re-sutured at a more distal point. |
 |
Fig. (5C). Re-examination of the upper eyelid height and curvature in the sitting position. |
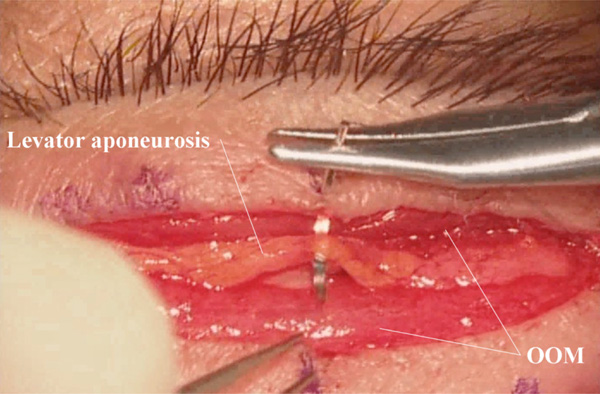 |
Fig. (6). (Surgeon’s view) Creation of the upper eyelid crease. OOM: orbicularis oculi muscle. |
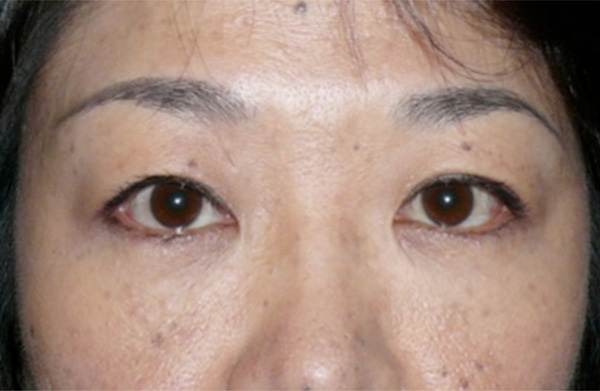 |
Fig. (7). Postoperative outcome at 6 weeks post-operatively. The patient is in a sitting position. |
The anterior aspect of the levator aponeurosis is also detached from the orbicularis oculi muscle, and the white line [17-19], which is the confluent part between the levator aponeurosis and the orbital septum, is confirmed (Fig. 3). Of notice here is the 3-dimentional structure of the merging point between the levator aponeurosis and the orbital septum. When the orbital septum above the white line is incised transversely, the white glistening anterior layer of the levator aponeurosis can be seen (Fig. 4). Old patients with fair to poor levator function may have a misleading fatty degeneration in the aponeurosis [15].
The centre of the eyelid fissure is then determined [17]. First, the eyelid margin above the centre of the pupil is pulled superiorly and an isoscele triangle is created, the part of which corresponds to the centre of the eyelid fissure. Then, the centre of the levator aponeurosis is determined by making an isosceles triangle of the levator aponeurosis with inferior traction, the tip of which corresponds to the centre of the levator aponeurosis [18]. These steps are essential to avoid a postoperative temporal flare [19].
A 6-0 nylon or vicryl® suture is passed from the centre of the levator aponeurosis, just a few millimeters above the white line, and fixated to central part of the tarsal plate, by taking a partial thickness bite at around the middle height of the tarsus. The suture is tightly knotted four times to prevent loosening.
As the medial horn of the levator aponeurosis is structurally weaker than the lateral horn [19], therefore the medial part should be advanced about 2 mm more than the central part. In addition, as the levator aponeurosis is narrow proximally and wider distally, the narrow part of the aponeurosis should be sutured in cases that require a significant advancement. The medial horn supporting ligament can be used as a marking point to the medial margin of the levator aponeurosis [20].
At this stage, intraoperative quantification is performed while the patient is in a sitting position [21]. If overcorrection is noted (Fig. 5A), the levator complex is re-sutured more distally (Fig. 5B). This procedure is continued untill the desired height and contour of the upper eyelid are achieved (Fig. 5C). Two additional 6-0 nylon or vicryl® sutures are added medialy and laterally to form a more naturally-looking upper eyelid curvature. When there is no lagophthalmos, the redundant aponeurosis can be resected. When lagophthalmos exists, a forced eyelid closure test (downward eyelid push with a finger) is performed [22], and if the residual lagophthalmols is less than 2 mm, the chance of postoperative lagophtahlmos is very low. Any redundant eyelid skin, can now be also removed.
The double eyelid is formed by 3 separate sutures, taking care not to cause inappropriate outward rolling of the eyelid margin (Fig. 6). This step is known as the “Asian blepharoplasty technique” [23]. In Caucasians and higher eyelid crease patients, this step is not required, and when the skin is closed with 6-0 nylon or vicryl® sutures they are also passed through the aponeurosis. The intraoperative quantification in the sitting position is shown to match the final posoperative outcome after 6 weeks (Fig. 7) [21].
DISCUSSIONS
Patients with aponeurotic ptosis frequently show involutional or post-inflammatory changes in Müller’s muscle in addition to the aponeurotic changes [14, 15, 24]. Transcutaneous ptosis surgery with advancement of both the levator aponeurosis and Müller’s muscle (levator resection) is anatomically and pathophysiologically more appropriate than the other techniques for ptosis surgery, and results in a more naturally-looking upper eyelid contour.
The levator resection advances the levator aponeurosis as well as Müller’s muscle. Cases with levator function of 10 mm or more usually require a small degree of advancement of the levator complex [25]. In addition, cases with a poor response to the phenylephrine test, which mostly result from involutional changes in Müller’s muscle [16], may require a smaller degree of advancement of the levator tissue if levator resection is chosen over the other types of ptosis repair techniques. This is because the levator resection advances both layers of the levator complex.
Cases with poor levator function may require a very significant advancement of the levator complex, which may cause dry eyes [26] because of a poorer fitting between the lower part of the upper eyelid and the underlying cornea. In addition, as the levator aponeurosis is narrower in its proximal part [19], a larger degree of advancement may cause difficulties in appropriate fixation of the levator aponeurosis to the tarsal plate, and result in an unnatural upper eyelid curvature. Furthermore, postoperative astigmatism may occur in such cases of advancement [27], which may be of significant importance in children undergoing this surgery, and who may develop amblyopia. Levator resection was shown to cause more postoperative astigmatism than the sling operation [28]. A possible reason is that the advanced aponeurosis presses the globe and changes the corneal shape [27]. A patient with ptosis who intends to undergo cataract or refractive surgery in the future should consider having his or her ptosis surgery done first to avoid any additional refractive changes [27].
Some surgeons believe that Müller’s muscle should not be manipulated during ptosis surgery because it acts as a muscle spindle to the LPS muscle [29]. However, with a positive phenylephrine test, the levator complex is not advanced much in the levator resection, and a certain amount of Müller’s muscle is spared, and its function is partially preserved. That theory has several drawbacks. First, cases with no response to the phenylephrine test will not react to the sympathetic stimulation. Second, in cases where only the levator aponeurosis is advanced, Müller’s muscle is loosened and cannot react to the sympathetic stimulation, possibly resulting in denervation atrophy. Third, the sympathetic reflex from Müller’s muscle cannot be explained only by the Müller’s muscle itself, and the smooth muscle fibers in the orbit should also be taken into consideration [30]. Forth, studies on fetuses have shown that the LPS muscle has its own muscle spindles, although their number is smaller than that of the other extraocular muscles [31].
In conclusion, the levator resection is a commonly used procedure that addresses the pathophysiology of most types of ptosis except for the myogenic type. Cases with good levator function, irrespective of the response in the phenylephrine test, are best suitable for this technique. In cases with poor levator function where a large degree of levator complex advancement is required, it may result in undesired ocular side effects. We believe that with the right patient selection, the levator resection technique is an effective method for ptosis repair.