RESEARCH ARTICLE
Management of Post Laser In Situ Keratomileusis Ectasia with Simultaneous Topography Guided Photorefractive Keratectomy and Collagen Cross-Linking
George D Kymionis1, Dimitra M Portaliou*, 1, Vasilios F Diakonis1, Alexandra E Karavitaki1, Sophia I Panagopoulou 1, Mirko R Jankov II 2, Efekan Coskunseven 3
Article Information
Identifiers and Pagination:
Year: 2011Volume: 5
First Page: 11
Last Page: 13
Publisher ID: TOOPHTJ-5-11
DOI: 10.2174/1874364101105010011
Article History:
Received Date: 11/8/2010Revision Received Date: 15/10/2010
Acceptance Date: 3/11/2010
Electronic publication date: 11/02/2011
Collection year: 2011

open-access license: This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
Abstract
A thirty-nine year old man was referred to our institute due to progressive decreased visual acuity five years after bilateral Laser in situ Keratomileusis (LASIK). Topography revealed signs of post – LASIK ectasia. Patients’ left eye was treated with simultaneous Topography Guided Photorefractive Keratectomy (PRK) followed by Corneal Collagen Cross Linking (CXL). Twelve months after the combined procedure both uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) showed significant improvement while topographic findings revealed an improvement of the astigmatic pattern. All higher order aberrations showed a significant decrease twelve months postoperatively. Combined topography guided PRK and corneal cross linking could represent an alternative treatment for post – LASIK ectasia.
INTRODUCTION
Keratectasia is the condition in which the cornea progressively thins and steepens resulting in the production of myopia, irregular astigmatism and loss of corrected distance visual acuity (CDVA) lines. This corneal entity has been reported extensively, mainly after Laser in Situ Keratomileusis (LASIK) [1]. There are several parameters such as high myopic corrections, thin corneas and residual corneal bed thickness less than 250 μm, which represent major risk factors for this condition [2].
Therapeutic solutions include spectacle correction, rigid gas permeable contact lenses and intrastromal corneal ring segments [3] in order to achieve adequate visual rehabilitation. Lamellar or penetrating keratoplasty [4] are considered the ultimate solution when all other choices have failed to provide a functional visual acuity.
Corneal Collagen Cross linking (CXL) is a relatively new technique used for the stabilization of ectatic disorders [5,6]. The objective of this technique is the increase of corneal strength and stability by inducing cross links at the corneal stroma [7].
In this case report, we present a patient with post – LASIK ectasia that underwent simultaneous Topography Guided PRK and CXL in the left eye.
CASE REPORT
A thirty-nine year old man was referred to our institute complaining about progressive decreased visual acuity five years after bilateral LASIK. Attempted correction was -1.00 / -2.00 x 20 and -1.25 / -2.50 x 160 in the right and left eye respectively. Pre-LASIK corneal thickness was 543μm and 550μm while flap thickness was 193μm and 180μm in the right and left eye respectively. At the time of the examination, uncorrected distance visual acuity (UDVA) was 20/40 (Snellen) in the right and 20/100 in the left eye and corrected distance visual acuity (CDVA) was 20/32 (manifest refraction -1.00 -1.50 x 45) for the right eye and 20/40 (manifest refraction +0.50 -4.00 x 125) for the left eye. Topographic findings (Topolyzer, Wavelight, Erlangen, Germany) were consistent with post – LASIK ectasia in both eyes. Keratometry readings were 39.30 x 38 / 40.75 x 128 in the right eye and 37.76 x 139 / 42.29 x 49 in the left eye.
The patient could not achieve functional visual acuity with spectacle correction due to the irregular shape of the cornea. Additionally, the patient had contact lens intolerance.
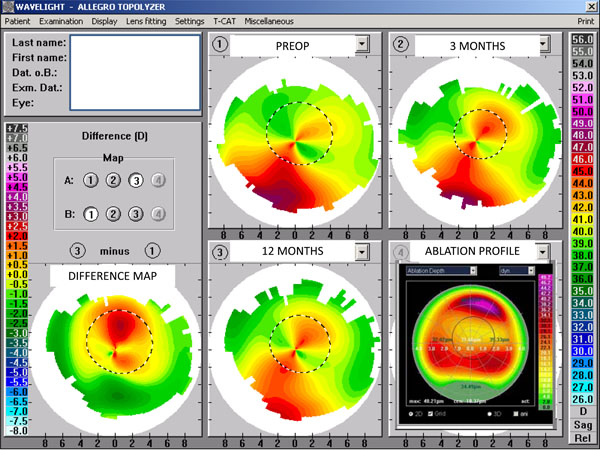
Patient was advised to undergo simultaneous Topography Guided PRK and CXL treatment in the left eye first (Fig. 1).
TOPOGRAPHY CUSTOMIZED PRK PROCEDURE
PRK was performed before the CXL treatment. The surgical procedure was conducted under sterile conditions. The patient’s eye was anesthetized with proparacaine 0.5% (Alcaine). We applied a customized ablation on top of the LASIK flap (T-CAT software, Wavelight, Erlangen, Germany). The epithelium was removed by Transepithelial Phototherapeutic Keratectomy (t-PTK). The t-PTK ablation was performed in an 8.0 mm zone in an intended depth of 50μm (Fig. 1). A maximum ablation depth of 48.21μm has been chosen in order to aim for a decrement in astigmatism but not to remove a significant amount of tissue that would jeopardize the biomechanical integrity of the cornea. No adjuvant Mitomycin-C was used.
CXL PROCEDURE
Immediately after PRK, riboflavin 0.1% solution was instilled repeatedly for approximately 30 minutes. Penetration of the cornea and presence of riboflavin in the anterior chamber (riboflavin shielding) was monitored by slit-lamp examination. The Ultraviolet - A irradiation was performed using an optical system (UV-X illumination system version 1000). Irradiance was performed for 30 minutes. During treatment the riboflavin solution was applied every 5 minutes to saturate the cornea. At the end of the procedure, a bandage contact lens was applied until full re – epithelization. Postoperative medication included diclofenac sodium 0, 1% (Denaclof, Novartis) for two days as well as antibiotic/corticosteroid (tobramycin/dexamethasone) drops (Tobradex, Alcon Laboratories, Inc.) until the removal of the bandage contact lens. Patient was encouraged to use artificial tears at least six times per day for six months postoperatively.
Patient was examined daily until the epithelium healed completely and at one, three and twelve months postoperatively.
One month after the combined procedure, UDVA was 20/63 and CDVA was 20/30 with a manifest refraction of -1.25 -4.25 x 180 (left eye). The slit-lamp biomicroscopy revealed the presence of trace haze.
Three months postoperatively, UDVA was 20/40 and CDVA was 20/25 with a refractive error of -0.50 -3.00 x 145. There were no signs of trace on slit-lamp examination. Topography revealed a symmetric astigmatism pattern.
Twelve months after the combined procedure, both UDVA and CDVA remained stable while there was further topographic improvement (Fig. 1).
Patient perceived an improvement in his night vision and glare problems that originally appeared a few months after the LASIK procedure.
Wavefront analysis was performed with the Wasca Wavefront Analyzer (Carl Zeiss Meditec, Jena Germany), and the eye was under cycloplegia. All higher order aberrations showed a decrease twelve months postoperatively. Total higher order Root Mean Square (RMS) (3rd and 4th order) for a 5mm pupil diameter, decreased from 0.74 microns preoperatively to 0.25 microns twelve months postoperatively. In particular coma like RMS decreased from 0.26 microns to 0.01 microns twelve months postoperatively.
DISCUSSION
The progressive thinning of the cornea, identified as ectasia, is a possible post refractive surgery complication with severe impact on patients’ vision. The incidence of iatrogenic ectasia is mainly attributed to LASIK [8].
Until recently the ‘’gold standard’’ treatment in cases of progressive ectatic disorders was penetrating keratoplasty. An alternative and less invasive treatment introduced recently is CXL with riboflavin and Ultraviolet - A irradiation that arrests the progression of ectasia producing a stiffening effect and stabilizing the cornea [6].
In this case report, patient underwent simultaneous topography guided PRK and CXL for the management of post – LASIK corneal ectasia. During the pre-operative examination the patient complained of deterioration of the visual acuity that could not been resolved with spectacles or contact lenses.
Kanellopoulos et al. [9] in a previous study proposed a two step procedure of corneal cross-linking followed by PRK with a one year interval. According to this study, documentation of the stability for at least one year is essential before proceeding with the laser treatment. This approach has several limitations. The stiffened cross linked corneal tissue is partly removed by the consequential PRK procedure. There is no control over the efficacy of this approach, since the corneal ablation rate could be different in cross linked corneas as compared to virgin corneas and this could lead to unpredictable refractive results. Lastly, there is an increased possibility of post-PRK haze formation since it is known that after CXL the anterior stromal is repopulated by new keratocytes after six months [10, 11].
The desirable effect of the topography guided PRK was to produce a more regular appearance in the central cornea by smoothening the anterior surface. In accordance with previous studies [12] performed on keratoconic patients that underwent PRK – CXL, we adopt a Topo – guided photorefractive keratectomy in order to remodel the asymmetric cornea in the most possible customized way. Topographically, the central cornea appears with a symmetric astigmatic pattern.
Twelve months after the procedure all higher order aberrations showed decrease. Especially coma like RMS was almost eliminated completely. Postoperatively the objective findings from corneal topography and Wavefront analysis agree with the improvement of the subjective symptoms of the patient.
A possible limitation of this combined approach is the fact that the removal of corneal tissue by laser ablation could jeopardize the integrity of the cornea and increase the risk of endothelial cell damage during irradiation.
The significant clinical improvement and the apparent stability of the ectasia during the post-operative follow-up lead us to believe that the simultaneous approach of topography guided PRK and CXL may offer an alternative solution to post refractive surgery ectasia. Longer follow-up and larger patient sample is necessary in order to validate the safety and the stability of this combined procedure.