All published articles of this journal are available on ScienceDirect.
LETTER TO THE EDITOR Excision of Congenital Bilateral Persistent Pupillary Membrane in a Child with Exotropia
Abstract
Purpose :
To report the clinical and histopathological findings of a patient who had bilateral persistent pupillary membrane with exotropia and high hyperopia.
Methods :
Case Report: A 7-year-old boy presented with a persistent pupillary membrane in both eyes. His best corrected visual acuity (BCVA) was 20/20 in the right eye and 20/32 in the left eye with exotropia of 18 prism diopters. He underwent surgical resection of both membranes. At 5 months postoperatively, BCVA was 20/20 with final bilateral refraction of +6.5 D in both eyes. Exotropia and photophobia showed improvement immediately after surgery. Histopathological examination revealed typical features of normal iris tissue in the excised membranes.
Conclusion :
Bilateral persistent pupillary membranes were excised successfully without injury to other ocular tissues, including the crystalline lens. Surgical treatment may be required for the management of persistent pupillary membrane associated with visual impairment such as exotropia or photophobia.
INTRODUCTION
Persistent pupillary membrane (PPM) is a common congenital anomaly of the eye, in which remnants of a fetal membrane persist as strands of tissue crossing the pupil. Although the exact pathophysiology is not well understood, it is thought that PPM represents a congenital remnant of the anterior portion of the tunica vasculosa lentis [1, 2]. The anterior portion of the tunica vasculosa lentis is usually fully developed by 9 weeks of gestation and normally disappears by 34 weeks [3]. PPM probably arises due to incomplete resorption of this tunica over the anterior lens capsule [2]. Because histological examination showed that the membrane was composed of normal iris tissue, this supports an origin from congenital iris hyperplasia.
PPM is most common in premature infants and becomes rare over time because the membrane is absorbed with age. PPM is usually asymptomatic, rarely affects vision, and does not appear to be linked to cataract formation. Additionally, bilateral sever PPV with exotropia and high hyperopia are relatively uncommon [4]. Here we report a patient with exotropia and photophobia, in whom bilateral PPM required surgical excision.
CASE REPORT
A 7-year-old boy complained of poor vision and photophobia in both eyes. At the first visit, his uncorrected visual acuity (UCVA) was 20/20 in the right eye and 20/40 in the left eye. The preoperative best-corrected visual acuity (BCVA) was 20/20 with refraction of + 5.50 –1.75 ×170 in the right eye and 20/32 with refraction of + 5.00 –4.00 ×180 in the left eye. He was not wearing glasses or contact lenses for correction of hyperopia. Eye movements were normal. Alternate prism and cover measurements revealed exotropia of 18 prism diopters in the left eye. Slit-lamp examination revealed a persistent pupillary membrane (PPM) in both eyes, but otherwise was essentially normal (Fig. 1). Each PPM consisted of many strands inserting into the collarette of the iris with several free floating edges. The membrane covered half of the pupil area in the right eye and two thirds in the left eye, and its root was fully extended after mydriasis with phenylephrine eyedrops. The central portion of each membrane was attached to the anterior lens capsule, but there was no posterior synechiae in either eye. Because of their large size, the membranes seemed to cause blurred vision and visual impairment by occluding the visual axis. Findings on funduscopy were normal. The patient had no family history of ocular disease.
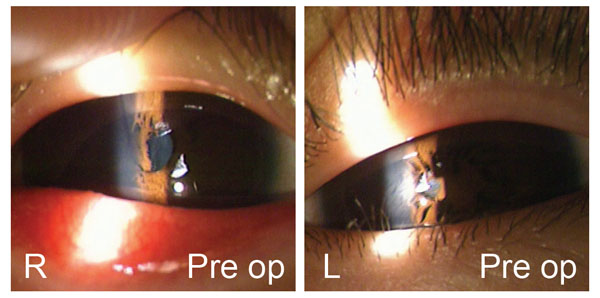
Anterior segment photographs obtained before surgical treatment of bilateral persistent pupillary membrane (PPM).
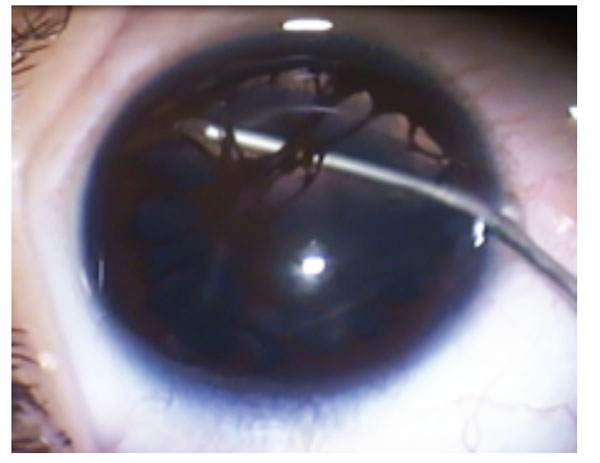
Surgical membranectomy and pupilloplasty in the left eye. The PPM was separated by using high-viscosity viscoelastic material, excised from the anterior lens capsule with curved iris scissors, and removed by irrigation and aspiration.
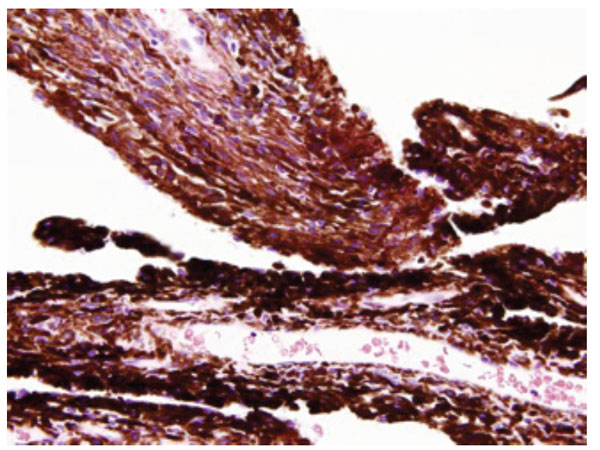
Histological features of the excised PPM. The PPM is composed of fibrovascular tissue containing stromal melanocytes, vascular tubes (arrows), and melanin-rich pigment epithelial cells (hematoxylin and eosin, 40X).
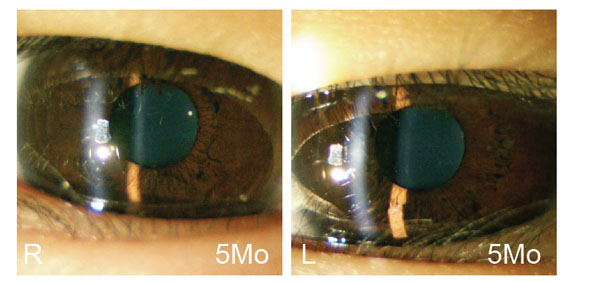
Anterior segment photographs obtained 5 months after surgical treatment of bilateral persistent pupillary membrane (PPM).
The PPM was surgically resected from both eyes under general anesthesia. A superior clear corneal incision was made using a 2.4 mm keratome. Then a high-viscosity viscoelastic material (Opegan-Hi™, Santen, Osaka, Japan) was injected into the anterior chamber and behind the iris to separate the PPM from the anterior lens capsule (Fig. 2), after which the strands were excised with a curved iris scissors. Next, residual strands were removed completely by irrigation and aspiration, after which hydration of the superior corneal wound was done with sterile balanced salt solution (OpeGuard Neo Kit®; Senju, Osaka, Japan). Histopathological examination revealed typical features of normal iris tissue in the excised membranes (Fig. 3). Each specimen consisted of a thin fibrovascular membrane containing small vessels, fibrocytes, and stromal melanocytes. Melanin-rich pigment epithelial cells covered the surface of the membrane that was closest to the pupillary margin.
Postoperatively, the pupils were round and central in both eyes (Fig. 4). There were no surgical complications, including endophthalmitis, lens damage, or corneal opacity. UCVA was 20/40 in the right eye and 20/50 in the left eye. BCVA was 20/20 with refraction of + 7.50 –1.75 ×170 in the right eye and 20/20 with a refraction of + 9.00 –5.75 ×5 in the left eye at 5 months postoperatively. Exotropia resolved and orthophoria was achieved immediately after surgery.
DISCUSSION
In this patient, bilateral PPMs were successfully removed with microscissors. Surgical treatment is recommended as the first choice for PPM that totally covers the pupil in children because congenital PPM may cause amblyopia.
Surprisingly, the present patient did not develop amblyopia, although he had bilateral severe PPM and hyperopia. In fact, he had good preoperative UCVA despite very hyperopic refraction. We speculate that an aperture in the PPM and iris created a pinhole effect that allowed the development of his vision. Central obstruction of the pupil by the PPM was undoubtedly responsible for the altered visual axis and maintaining the visual axis by compensating exotropia may have effectively prevented amblyopia.
Patients with PPM can usually be managed conservatively because small to medium membranes do not cause visual impairment. Attachment of PPM to the cornea may cause corneal opacity and stromal edema, while attachment to the lens capsule or synechia might lead to cataract formation. Various methods have been reported for the management of PPM, including the use of mydriatic agents, argon laser [5] or Nd:YAG laser pupilotomy [6], and surgical resection [7-11]. Among them, topical mydriatic agents are generally used to prevent adhesions and posterior synechiae in patients with a small PPM. Nd:YAG laser pupilotomy can also be recommended as a simple treatment for a PPM in adults because there is no risk of postoperative infection. However, laser pupilotomy may cause irreversible lens damage, cataract, uveitis, and increased intraocular pressure [6]. Additionally, laser pupilotomy cannot be performed safely without general anesthesia in young children.
In our patient, the PPMs partly blocked the visual axis, which could be associated with a risk of amblyopia. Therefore, surgical treatment was selected for this case and the visual problems were cured without intraoperative or postoperative complications. Further treatment of amblyopia with glasses would be effective in this patient because an age of 6 to 8 years is thought to repeat the end of the "critical period" for visual development.
CONCLUSION
In summary, we encountered a rare case of bilateral PPM associated with exotropia. Surgical excision of both membranes was performed successfully without complications and improvement of vision was achieved. In particular, control of photophobia gave the patient confidence and increased his motivation to continue orthoptic training.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
ACKNOWLEDGEMENTS
This work was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science.


