RESEARCH ARTICLE
Comorbidities in Corneal Refractive Surgery Candidates: A Cross-Sectional Study
Phit Upaphong1, 2, Napaporn Tananuvat1, 2, Somsanguan Ausayakhun1, 2, Winai Chaidaroon1, 2, Chulaluck Tangmonkongvoragul1, 2, Muanploy Niparugs1, 2, *
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187436412204051
Publisher ID: e187436412204051
DOI: 10.2174/18743641-v16-e2204051
Article History:
Received Date: 3/11/2021Revision Received Date: 20/1/2022
Acceptance Date: 31/1/2022
Electronic publication date: 21/06/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Individuals with refractive errors sometimes have other associated ocular and systemic abnormalities.
Objectives:
To explore ocular and systemic comorbidities in Corneal Refractive Surgery (CRS) candidates and to examine any contraindications for CRS.
Methods:
This was a cross-sectional study. Medical records of individuals who underwent a refractive surgery screening at Chiang Mai University LASIK Center, Chiang Mai, Thailand, were reviewed. All clinical data of the initial visit were evaluated. Eyes with a history of CRS and phototherapeutic keratectomy were excluded.
Results:
A total of 1,167 cases (2,334 eyes) were recruited, out of which 643 cases were females (55.09%). Myopia was the most common type of refractive error (2,120 eyes, 90.83%), and 868 (40.94%) eyes had high myopia. Approximately 45% (n=526) of the cases had worn contact lenses. The five most common ocular comorbidities (eyes, proportion) included keratoconus suspect (297, 12.72%), cataract (246, 10.53%), dry eye/probable dry eye (208, 8.91%), glaucoma suspect (184, 7.88%), and amblyopia (149, 6.38%). The most common systemic conditions that affected choices or outcomes of CRS were hypertrophic scar/keloid (169 cases, 14.48%) followed by allergy/asthma (127 cases, 10.88%). A total of 1,028 eyes (44.04%) were excluded from CRS, mainly due to abnormal corneal topography (470/1,028 eyes, 45.72%).
Conclusion:
Most refractive candidates were myopic and contact lens wearers. Serious ocular sequelae from myopia and contact lens use were not uncommon. Additionally, systemic diseases regularly affected the CRS options. The most common contraindication for CRS was abnormal corneal topography. Our study, thus, emphasizes the need for thorough ocular and systemic screenings of refractive candidates.
1. INTRODUCTION
Refractive error is a common ocular condition in which the eye cannot focus the light rays precisely on the retina, resulting in blurred vision. To achieve the best visual acuity without the
use of glasses or contact lenses, refractive surgery is a procedure aiming to correct the abnormal refractive states of the eyes with refractive errors. Myopia is the most common refractive error in a person desiring refractive surgery [1]. However, eyes with myopia, exceptionally high myopia, also contain risks of having other pathological ocular conditions, including glaucoma, retinal breaks, retinal detachment, and myopic retinal degeneration [2-4]. Thus, refractive surgeons should be aware of these coexisted conditions in these specific populations, as those conditions may lead to irreversible blindness, and most importantly, refractive surgery may obscure or worsen some conditions. Moreover, amblyopia is not an uncommon diagnosis in patients with high myopia [5], and dry eyes can be regularly found in refractive candidates [6]. Notably, these conditions should be diagnosed prior to the refractive surgery as they could result in unsatisfactory visual outcomes.
Currently, there has been a limited number of studies on the clinical profiles of individuals having refractive surgery screening, and the results have varied from region to region [1, 7, 8]. Our study, therefore, aimed to explore the comorbidities and clinical characteristics of individuals with refractive errors being screened for refractive surgery in Northern Thailand.
2. MATERIALS AND METHODS
This was a cross-sectional study. Medical records of individuals who underwent a refractive surgery screening by five refractive surgeons at Chiang Mai University (CMU) LASIK Center, Chiang Mai, Thailand, between January 2013 and March 2020 were reviewed. The CMU LASIK Center is one of the two laser refractive surgery centers in Northern Thailand. Laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) are the refractive surgical options. Eyes with previous corneal refractive surgery (CRS) or phototherapeutic keratectomy were excluded.
At the center, the following clinical data were routinely examined at the first screening for refractive surgery, including demographic data, social history, lifestyle, ocular/systemic comorbidities, and ophthalmic examinations, which were uncorrected distance visual acuity (UCDVA), best-corrected distance visual acuity (BCDVA), intraocular pressure (IOP), manifest and cycloplegic refractions, slit-lamp examination, and dilated fundus examination, corneal topography, and tomography. The assessment of visual acuity (VA) was performed using the Early Treatment Diabetic Retinopathy Study (ETDRS) chart and subsequently converted to the logarithm of the minimum angle of resolution (LogMAR) scale for analysis. The IOP was measured by the Goldmann applanation tonometer. The evaluation of corneal topography and tomography was performed by Allegro Topolyzer Vario (WaveLight GmbH, Erlangen, Germany) for keratometric parameters and Pentacam® (Oculus Optikgeräte GmbH, Wetzlar, Germany) for other parameters. Recorded contraindications for refractive surgery were analyzed.
This study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board/Ethics Committee of the Faculty of Medicine, Chiang Mai University (Study code: OPT-2564-08019).
2.1. Definitions
High myopia was defined as the refractive error of at least -6.00 diopters (D) spherical equivalence. The diagnosis of keratoconus was based on Rabinowitz criteria [9]. The keratoconus suspect (KCS) was stratified into 1) keratoconus (KC) if the eyes had no keratometric, retinoscopic, or biomicroscopic signs of keratoconus but had an inferior-superior asymmetry and/or bowtie pattern with screw radial axis deviation [10], and 2) forme fruste keratoconus (FFKC) if the eyes had back difference elevation and abnormal elevation-based topography parameters on Pentacam® without apparent topographic abnormality. Dry eyes and probable dry eyes were diagnosed based on the 2006 Japanese diagnostic criteria for dry eyes [11]. Amblyopia was defined as having a BCDVA of less than 20/32 in the absence of ocular pathology [5]. Glaucoma suspects were diagnosed through the following ophthalmic findings: suspicion of glaucomatous damage on the optic disc or retinal nerve fiber layer, suspicion of visual field damage with no other identified pathologies, and persistently elevated IOP [12].
2.2. Statistical Analysis
Data were analyzed using the SPSS version 22 (IBM Corp., Armonk, NY, USA). For descriptive statistics of continuous variables, the mean was used for normally distributed data, while the median was for non-normally distributed data. Parameters from patients aged ≤40 and >40 years were compared. Listwise deletion was used to handle missing data. A comparison of categorical data between the two groups was made by Fisher’s exact test. The comparison of median or mean between two independent groups was made by the Mann-Whitney U test or Student t-test. To correct the repeated measurements of CCT and age groups, multilevel analysis adjusted by the degree of refractive error was performed using the robust method. Likewise, to correct the repeated measurements of CCT and refractive status, multilevel analysis adjusted by age and degree of refractive error was performed.
3. RESULTS
A total of 1,167 cases (2,334 eyes) with 643 females (55.09%) were recruited. Thirty-three eyes with the previous CRS, including LASIK (18 eyes), PRK (4 eyes), radial keratotomy (RK; 6 eyes), and arcuate keratotomy (AK; 5 eyes), were excluded. The demographic data of the studied cases are shown in Table 1. Of the 1,167 cases, 526 (45.07%) were contact lens wearers. Among 2,334 eyes, 1,013 (43.40%) eyes had a history of contact lens wear, of which 876 eyes were soft lenses, 66 were soft toric lenses, 13 were rigid gas permeable lenses, and 58 were unknown types. The median (IQR, interquartile range) duration of contact lens wear was 8 (3.5,10) years. In the high myopia group, the proportion of eyes using previous contact lenses was higher than that of non-contact lenses, 510/868 versus 503/1,466 (P = 0.00).
A history of ocular trauma was present in 15/2,334 eyes (0.64%). Regarding previous ocular procedures, 10/2,334 (0.43%) eyes had blepharoplasty, 12/2,334 (0.51%) had surgery due to previous retinal detachment, and 5/2,334 (0.21%) had laser photocoagulation for retinal breaks. Cataract surgery was performed in only 3/2,334 (0.13%) eyes.
Of the 2,334 eyes, the median (interquartile range, IQR) of the uncorrected distance LogMAR VA was 1.0 (0.7, 1.3), with the Snellen equivalence of 20/200. The median (IQR) of the best-corrected distance LogMAR VA was 0 (-0.1, 0), with the Snellen equivalence of 20/20. Ophthalmic parameters by age group and refractive state are presented in Table 2. Overall, the mean IOP (IQR) was 15.19 (4.02) mmHg. UCDVA, MRSE (Manifest Refraction Spherical Equivalence), cylindrical refractive errors, central corneal thickness (CCT), and IOP between eyes of individuals aged ≤40 years and >40 years were significantly different. Additionally, comparing myopic and hyperopic eyes, the differences in BCDVA, MRSE, and CCT were also statistically significant.
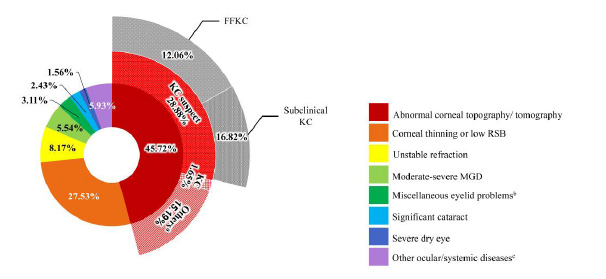
The ocular abnormalities from the self-report and ophthalmic examinations are shown in Table 3. The most common self-reported ophthalmic problem was dry eye symptoms (116/2,334 eyes, 4.97%). The five most common ophthalmic conditions detected were keratoconus suspect (297/2,334 eyes, 12.72%), cataract (246/2,334 eyes, 10.53%), dry eyes/probable dry eyes (208/2,334 eyes, 8.91%), glaucoma suspect (184/2,334 eyes, 7.88%) and amblyopia (149/2,334 eyes, 6.38%). The underlying systemic conditions affecting surgeons’ decisions on refractive surgeries are listed in Fig. (1), from which the most frequent one was hypertrophic scar (HTS)/keloid (169/1,167 cases, 14.48%) followed by allergy/asthma (127/1,167 cases, 10.88%). However, other less frequent systemic diseases included hypertension (119/1,167 (10.20%) cases), dyslipidemia (24/1,167 (2.06%) cases), and gout (8/1,167 (0.69%) cases). The contraindications for CRS are illustrated in Fig. (2), in which 1,028 eyes (44.04%) were considered unsuitable for CRS. The most frequent etiology was abnormal corneal topography/tomography. In cases of having active conjunctivitis or anterior blepharitis, the conditions can be resolved after treatment.
| Gender: cases (%) | |
|---|---|
| Male | 524 (44.90%) |
| Female | 643 (55.09%) |
| Nationality: cases (%) | |
| Thai | 1,157 (99.14%) |
| Age: years | |
| Mean (SD) | 33.27 (12.58) |
| Age group | |
| ≤ 40 years (cases, %) | 851 (72.92) |
| >40 years (cases, %) | 316 (27.08) |
| Median age (IQR) of the initial recognition of refractive error: years | 10 (14, 18) |
| Parameters |
Age ≤40 years (n = 851 cases, 1,702 eyes) |
Age >40 years (n = 851 cases, 632 eyes) |
P-value |
Myopia (n = 2,120 eyes) |
Hyperopia (n = 214 eyes) |
P-value | |
|---|---|---|---|---|---|---|---|
| Distant visual acuity (LogMAR) | |||||||
| Uncorrected | Median (IQR), SE | 1.3 (0.8, 1.1), 20/400 | 1.1 (0.4, 0.9), 20/250 | 0.00 | 1.0 (0.8, 1.3), 20/200 | 0.3 (0.1, 0.7), 20/40 | 0.00 |
| Best-corrected | Median (IQR), SE | 0 (-0.1, 0), 20/20 | 0 (-0.1, 0), 20/20 | 0.07 | 0 (-0.1, 0), 20/20 | 0 (-0.1, 0.1), 20/20 | 0.08 |
| Refraction | |||||||
| MRSE (D) | Median (IQR) | -5.00 (-7.87, -2.50) | -3.00 (-6.38, -4.06) | 0.00 | -5.00 (-7.75, -2.62) | +0.75 (0, +2) | 0.00 |
| Cylinder (D) | Median (IQR) | -2.25 (-3.50, -1.50) | -0.75 (-1.25, -0.50) | 0.00 | -1.00 (-2.00, -0.50) | -0.75 (-1.25, -0.50) | 0.95 |
| High myopia | Eyes (%) | 693 (40.72) | 175 (27.69) | ||||
| Keratometry | |||||||
| K1 (D) | Mean (SD) | 43.62 (11.54) | 44.63 (22.16) | 0.42 | 43.76 (13.72) | 43.74 (4.39) | 0.63 |
| K2 (D) | Mean (SD) | 46.70 (25.10) | 45.60 (18.43) | 0.29 | 45.86 (19.75) | 45.10 (5.00) | 0.94 |
| Average K (D) | Mean (SD) | 45.19 (13.86) | 45.12 (14.42) | 0.90 | 44.61 (12.47) | 44.42 (4.64) | 0.95 |
| Thinnest CCT (μm) | Mean (SD) | 531.41 (37.99) | 537.96 (32.68) | 0.01 | 532.76 (34.98) | 537.45 (52.31) | 0.00 |
| IOP (mmHg) | Mean (SD) | 14.94 (2.81) | 15.21 (2.89) | 0.02 | 15.19 (4.02) | 15.11 (3.17) | 0.34 |
| Self-report of Ocular Abnormalities | Eyes (%) (n = 2,334) |
|---|---|
| Ocular surface diseases | |
| Dry eyes | 116 (4.97) |
| Pinguecula | 16 (0.69) |
| Keratoconus | 9 (0.39) |
| Previous corneal ulcer | 8 (0.34) |
| Contact lens-related | 2 (0.09) |
| Corneal scar | 2 (0.09) |
| Pterygium | 2 (0.09) |
| History of herpes zoster ophthalmicus | 1 (0.04) |
| Vitreoretinal diseases | |
| Posterior vitreous detachment | 30 (1.29) |
| History of retinal detachment | 12 (0.51) |
| Previous retinal break | 5 (0.21) |
| Neovascular aged related macular degeneration | 3 (0.13) |
| Others | |
| Amblyopia | 27 (1.16) |
| Color blindness | 12 (0.51) |
| Strabismus | 9 (0.39) |
| Glaucoma | 7 (0.30) |
| Ocular myasthenia gravis | 6 (0.26) |
| Nystagmus | 2 (0.09) |
| Ocular abnormalities from eye screening | Eyes (%) (n = 2,334) |
| Ocular surface diseases | |
| Dry eyes and probable dry eyes | 208 (8.91) |
| Eyelid | |
| Moderate to severe meibomian gland dysfunction | 65 (2.78) |
| Trichiasis | 12 (0.51) |
| Epiblepharon | 8 (0.34) |
| Ptosis | 6 (0.26) |
| Lagophthalmos | 6 (0.26) |
| Anterior blepharitis | 4 (0.17) |
| Lid retraction | 4 (0.17) |
| Benign lid mass | 1 (0.04) |
| Conjunctiva | |
| Pinguecula | 54 (2.31) |
| Allergic conjunctivitis | 40 (1.71) |
| Cornea | |
| Keratoconus | 17 (0.73) |
| Keratoconus suspect | 297 (12.72) |
| Forme fruste keratoconus | 124 (5.31) |
| Subclinical keratoconus | 173 (7.41) |
| Corneal scar | 30 (1.29) |
| Pterygium | 14 (0.60) |
| Significant corneal arcus | 8 (0.34) |
| Corneal dystrophy | 2 (0.09) |
| Recurrent corneal erosion | 1 (0.04) |
| Lens abnormalities | |
| Cataract | 246 (10.53) |
| Lens subluxation | 1 (0.04) |
| Retinal diseases | |
| Lattice degeneration | 50 (2.14) |
| Retinal break/retinal hole | 26 (1.11) |
| Significant posterior staphyloma | 4 (0.17) |
| Macular scar | 2 (0.09) |
| Others | |
| Amblyopia | 149 (6.38) |
| Glaucoma | 36 (1.54) |
| Glaucoma suspect | 184 (7.88) |
| Iris defect | 2 (0.09) |
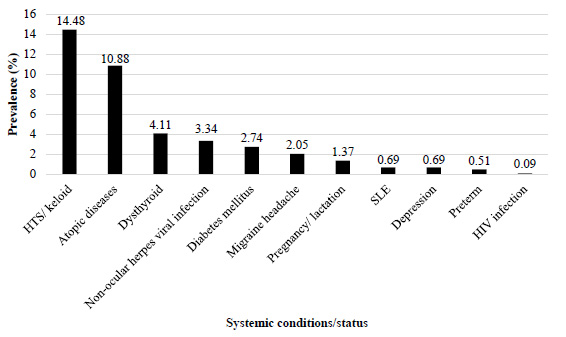 |
Fig. (1).
Underlying systemic conditions/status in candidates for refractive surgery. Abbreviations: HIV: human immunodeficiency virus, HTS: Hypertrophic scar, and SLE: Systemic lupus erythematosus. |
4. DISCUSSION
In this study, 55.1% were females, similar to previous studies (51.4 - 60%) [1, 8, 13]. The mean (standard deviation, SD) age in our cohort was 33.27 (12.58) years, which was not different from previous studies (range 26 - 39 years) [1, 8, 13]. The candidates in this age range have financial capabilities. Moreover, the individual aged < 40 years old could achieve the most benefit from CRS because presbyopia is not prevalent at this age.
In comparing ophthalmic parameters between age groups, candidates aged <40 years old tended to have poorer initial UCVA and a higher degree of refractive errors. Interestingly, candidates older than 40 years are likely to have a hyperopic shift. The Beaver Dam Eye Study [14] also reported similar trends. In this study, the eyes of candidates aged >40 years old had slightly higher CCT compared with those aged ≤40 years old. Adjusting the degree of refractive error, the CCT tended to be higher in those with high refractive error (P <0.01). Though most studies could not elucidate this association [15-17], our study revealed that increasing age was correlated with thinner CCT [18]. Moreover, IOP seems to be slightly higher in those aged >40 years old but not statistically significant (P = 0.32) when corrected for the degree of refractive error.
In this study, hyperopic eyes had better initial UCDVA, likely due to the higher degree of refractive error in myopes. Our data also showed that myopic eyes seemed to have thinner CCT than hyperopic eyes. Nonetheless, in the regression analysis, with adjustment for age and degree of refractive errors, the refractive error types did not influence CCT (P = 0.36). Similarly, previous studies [16, 17, 19] found no association between refractive error types and CCT.
Myopia was the major refractive problem in this study (2,120/2,334 eyes, 90.83%), and among myopic eyes, 868/2,120 eyes (40.94%) had high myopia, corresponding to the findings of Ang et al. [1]. A systematic review in 2000 [20], including 145 studies, indicated that myopia was the most common type of refractive error and was highly prevalent globally. This systematic review estimated that, in 2000, 1,406 million people worldwide were myopic (22.9% of the population), and as high as 163 million were highly myopic people (2.7% of the population).
Our study showed that 45.07% of the refractive candidates were contact lens wearers, comparable to 45.50% of those from a study in the Philippines [4]. This study found that the proportion of contact lens wearers significantly increased in the high myopia group compared with those with low to moderate myopia. This could be explained by the disturbance from more distorted images while using glasses and heavier lenses of a higher power.
Compared with the general population, individuals with high myopia carried a higher risk of glaucoma, retinal break, retinal detachment, myopic retinal degeneration, and amblyopia [2-5, 21]. For example, the prevalence of retinal detachment was reported to be 3.2% in high myopic eyes versus 0.7% in emmetropic eyes [22], and the prevalence of glaucoma was 2.9% in myopic eyes versus 2.1% in emmetropic eyes [21]. Moderate or high myopic eyes had three times greater risk of primary open-angle glaucoma than emmetropic eyes [21]. Regarding glaucoma, 1.61% of our studied eyes had been diagnosed with glaucoma. Xu L et al. [4] summarized that more than -6.00 D of myopia was a glaucoma risk factor. In our study, 8/2,334 (3.51%) had newly detected retinal abnormalities. Of these, lattice degeneration was the most common finding (50/2,334 eyes, 2.14%), followed by a retinal break or retinal hole (26/2,334 eyes, 1.11%). Notably, only a small number of eyes (17/2,334, 0.73%) previously had laser treatments for retinal breaks or surgeries for retinal detachment. Likewise, Ang et al. [1] reported 3.6% of retinal abnormalities in refractive surgery candidates, and lattice degeneration was the most frequent.
Dry eyes were one of the most common problems in refractive surgery candidates, and the prevalence based on the symptoms was up to 40 - 55% of LASIK candidates in one study [6]. Mild to moderate dry eyes, while not an absolute contraindication for refractive surgery, may lead to unsatisfactory visual outcomes [23]. Contact lens wear was another significant cause of dry eyes in myopia [24]. In the present study, 116/2,334 (4.97%) cases had dry eye symptoms using the self-reported problems. However, when the diagnosis was based on signs and/or symptoms, the prevalence increased to be 208/2,334 (8.91%). The finding may imply that some of our refractive candidates were diagnosed with dry eyes based on clinical signs rather than symptoms. A possible explanation might be the decreased corneal sensation from chronic long-worn contact lenses, as a large proportion of the candidates frequently wore the contact lens for eight years on average.
In the current study, corneal ectatic diseases (keratoconus, forme fruste keratoconus, and subclinical keratoconus) were among the common ophthalmic conditions in refractive candidates or 314/2,334 (13.45%) eyes. Similarly, a high prevalence of these corneal ectatic diseases among the refractive candidates was reported by Bamashmus et al. (28.3%), including 17.90% of keratoconus and 10.4% of subclinical keratoconus or forme fruste keratoconus [13].
Due to a large number of corneal ectatic diseases in our study, the most common contraindicated condition of eyes for laser-refractive surgery was abnormal corneal topography/tomography, 470/2,334 (20.14%), followed by thin cornea/low residual stromal bed (283/2,334 (12.13%) eyes). This is similar to the study of Torricelli et al. [8], which reported that up to 34.3% of the candidates had abnormal corneal topography, and 23.1% had insufficient corneal thickness. In other studies, although the causes varied among regions and diagnostic criteria, the three leading contraindications were a greater degree of myopia, thin cornea, and abnormal topographic patterns [1, 13].
Several systemic conditions such as autoimmune/connective tissue diseases, diabetes mellitus, and keloid formation should be taken into consideration before refractive surgery [25] as they might interfere with the preferred refractive surgical options, the procedure difficulty, and visual outcomes. As these conditions were not uncommon in our study population, the surgeons should be concerned regarding the underlying systemic conditions of the candidates. Moreover, despite being well-controlled, the effects of these systemic conditions on refractive surgery remained inconclusive [26-29]. In our study, the most commonly related systemic condition was HTS or keloid (169/1,167 cases, 14.48%), in which LASIK was more preferred over PRK at our center. The second leading condition was a group of atopic diseases (127/1,167 cases, 10.88%). Atopic diseases were associated with keratoconus and abnormal corneal topography indirectly via the increasing tendency of eye rubbing [30].
4.1. Limitations
First, as this was a retrospective study, some information may be incomplete. Second, this was a hospital-based study, so there were only cases with refractive errors with no matched emmetropic eyes controls. Therefore, the prevalence of ophthalmic abnormalities in this study may not represent the general population.
CONCLUSION
The epidemiological data of refractive candidates regarding ophthalmic and systemic abnormalities related to refractive errors were limited. Most of the refractive candidates were myopic and contact lens wearers, who were more prone to develop ophthalmic pathologies than the general population. If these pathologies were overlooked, post-operative visual outcomes might be unsatisfactory with possible future serious complications. As these conditions are regularly found, our study suggests that all refractive surgeons should be aware of the conditions, even in the individuals with no reported symptoms. Likewise, several systemic diseases that might affect refractive surgical options were not uncommon and were usually underreported by the patients due to unawareness. Our study was conducted in the Thai population, where the prevalence of myopia was high; however, the findings are likely to be beneficial in screening for candidates of CRS, who are usually myopic.
LIST OF ABBREVIATIONS
| AK | = Arcuate Keratotomy |
| BCDVA | = Best-Corrected Distance Visual Acuity |
| CCT | = Central Corneal Thickness |
| CI | = Confidence Interval |
| CRS | = Corneal Refractive Surgery |
| D | = Diopter |
| ETDRS | = Early Treatment Diabetic Retinopathy Study |
| FFKC | = Forme Fruste Keratoconus |
| HIV | = Human Immunodeficiency VirusHTS = Hypertrophic Scar |
| IOP | = Intraocular Pressure |
| IQR | = Interquartile Range |
| K | = Keratometry |
| KC | = Keratoconus |
| KCS | = Keratoconus Suspect |
| LASIK | = Laser in Situ Keratomileusis |
| LogMAR | = Logarithm of the Minimum Angle of Resolution |
| MGD | = Meibomian Gland Dysfunction |
| MRSE | = Manifest Refraction Spherical Equivalence |
| OR | = Odds Ratio |
| PRK | = Photorefractive Keratectomy |
| RK | = Radial Keratotomy |
| RSB | = Residual Stromal Bed |
| SD | = Standard Deviation |
| SE | = Spherical EquivalenceSLE = Systemic Lupus Erythematosus |
| UCDVA | = Uncorrected Distance Visual Acuity |
| VA | = Visual Acuity |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval from the Institutional Review Board/Ethics Committee of the Faculty of Medicine, Chiang Mai University, was obtained (Study code: OPT-2564-08019).
HUMAN AND ANIMAL RIGHTS
No animals were used that are the basis of this study. All the human procedures were followed in accordance with the tenets of the Declaration of Helsinki.
CONSENT FOR PUBLICATION
According to the ethical committee, informed consent was exempted due to the policy of the type of study, which was retrospective in nature, and all of the data was anonymised.
STANDARDS OF REPORTING
STROBE guidelines were followed for this cross-sectional study.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available from the corresponding author, [M.N], on special request.
FUNDING
Declared none.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.