RESEARCH ARTICLE
Treatment of Dissociated Vertical Deviation by Combined Recession–Resection of the Superior Rectus Muscle versus Recession with Posterior Fixation Suture
Hala K. Mattout1, *
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187436412204180
Publisher ID: e187436412204180
DOI: 10.2174/18743641-v16-e2204180
Article History:
Received Date: 12/1/2022Revision Received Date: 18/2/2022
Acceptance Date: 10/3/2022
Electronic publication date: 20/06/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background:
Management of dissociated vertical deviation (DVD) is still a matter of controversy in strabismus practice. Different surgical techniques are available, ranging from the weakening of the superior rectus or inferior oblique muscles to strengthening of the inferior rectus muscle, with variable success rates.
Objective:
To report the outcomes of correcting DVD by combined recession-resection of the superior rectus muscle and to compare the results with those of superior rectus muscle (SR) recession with posterior fixation sutures.
Methods:
The medical records of patients who had a surgical correction for DVD were retrospectively reviewed. Two groups of patients were identified; Group I (29 patients) was treated with the combined recession –resection of the SR and group II (37 patients) was treated by SR recession with posterior fixation sutures (Faden). Collected preoperative data included age, best-corrected visual acuity, presence of amblyopia, history of previous surgeries and angle of DVD. Operative data such as amount of SR recession and operative time were also extracted. The outcome measures taken at the final postoperative follow up visit included the surgical success rate which is identified as the percentage of patients with absent manifest DVD and the amount of residual latent deviation measured by prism cover test.
Results:
The mean follow-up period for all patients was 22.6 ±4.6 months. In the last follow-up visit, the surgical success rate was 76% in the combined recession-resection group and 73% in the faden group with no significant difference between both groups (p=0.8). No significant difference was found in the residual latent deviation in both groups as well. The recorded surgical time was significantly shorter in the combined recession- resection group (p<0.001). The reported complications included mild, temporary limitation of elevation without hypotropia in 5 patients (2 in group I (7%) and 3 patients in group II (8%)) with no significant difference between both groups (p=0.8).
Conclusion:
Combined recession-resection of SR is as effective as SR recession with posterior fixation suture in the management of DVD with the advantages of easier technique and less surgical time.
1. INTRODUCTION
Dissociated vertical deviation represents a special type of motility disorder commonly encountered in strabismus practice. The term Dissociated Vertical Deviation (DVD) was first proposed by Bielschowsky in 1930 to describe this unique motility disorder. It is termed dissociated as the non-fixing or covered eye moves upwards and laterally but when the cover is removed, it moves downward without a corresponding downward movement of the fellow eye; so it seems that it does not obey Hering’s law of simultaneous innervation of the yolk muscles and hence the term (dissociated) was used [1-5]. However, when Guyton (16) had recorded the extraocular muscles movements involved in DVD; he realized that the DVD appearing in the non-fixing eye is actually an unavoidable undesired effect of the intorsion and downward movements occurring in the fixing eye to damp the emerging latent nystagmus in that fixing eye. This phenomenon commonly occurs in patients with early-onset dysfunction in binocularity due to unbalanced vestibular input on covering one eye or even with monocular fixation, and it tends to be bilateral and asymmetrical [6-8].
The condition could be latent and appears only on orthoptic examination (compensated), but sometimes it manifests itself and becomes decompensated with social and psychological impacts so surgical correction becomes indicated [9].
As no single muscle was found to be incriminated in DVD, its correction could be achieved using variable surgical strategies with variable success rates; including weakening procedures for the superior rectus (SR) or inferior oblique muscles and strengthening procedures for the inferior rectus muscle. This variety of available surgical choices reflects the absence of an established recommended technique with fully satisfactory results [9-13].
Superior rectus weakening is so far the most widely practiced strategy, and the weakening effect could be achieved by superior rectus recession alone, posterior fixation suture alone or a combination of both. The posterior fixation suture, also termed faden operation, is used to weaken the rotational force of a rectus muscle without affecting the primary position. It acts by fixing the muscle to the sclera by a non-absorbable suture at 12-14 mm from its insertion, thus creating a new posterior insertion; this shortens the moment ar and reduces the muscle action only when the eye rotates towards the fixed muscle [14, 15].
Combined recession-resection is a technique that aims to simulate the effect of faden operation by resecting part of the rectus muscle followed by its recession by an amount exceeding the amount of resection. It was used with or without adjustable sutures to treat various disorders with gaze incomitance, including near-distance disparity esotropia, divergence excess exotropia and vertical incomitance secondary to paralytic or restrictive causes [16, 17]
This study aims to report the outcomes of correcting DVD by combined recession-resection of the SR muscle and compare the results with those of SR muscle recession with faden.
2. PATIENTS AND METHODS
The medical records of patients diagnosed with DVD in the period between February 2016 and May 2020 were retrospectively reviewed. The inclusion criteria for patients involved in the analysis were those who had no simultaneous surgery on other muscles, no previous surgeries on the SR muscle, no dysfunction in any of the oblique muscles and those who completed their follow up. This study adhered to the tenets of the Declaration of Helsinki of 1964, as revised in 2013. Patients were operated at El-Fat’h eye hospital (Zagazig, Egypt) and the Delta Medical centre (Dakahleya, Egypt) .The study was approved by the research ethics committee of El-Fat’h Eye Hospital. Written informed consent was provided by all patients or their parents prior to the procedure.
2.1. Two Groups of Patients were Identified
The first group (Group I) included patients who underwent combined recession-resection of the SR, and the second group (Group II) included patients who had received SR recession with posterior fixation suture (faden).
2.2. Preoperative Data
Preoperative data collected from patient's records included: age, gender, history of previous surgeries, best-corrected visual acuity (BCVA), and the results of ocular motility examinations. Extracted data also included the angle of deviation measured at a distance only for the reason of data analysis. The DVD was measured using a base-down prism bar held in front of the non-fixing eye covered by an occluder while the patient was looking at the 6 m distance. The downward refixation movement of the eye was noticed on removal of the occluder; the angle of deviation was determined by the prism power that neutralized that downward re-fixation movement. Asymmetrical DVD was considered when the inter-ocular difference in the measured angle was more than 10 PD. All measurements were taken with the patient putting his best optical correction.
2.3. Surgery
All surgeries were performed by the same surgeon (Mattout HK) under general anaesthesia, the recorded duration of the surgery was included in the analysis.
In patients where combined recession-resection was performed (group I), a standard limbal incision was made, the SR muscle was hooked and meticulously dissected to avoid inadvertent injury of the underlying superior oblique muscle. A part measuring 2.5 mm from the insertion end of the SR muscle was resected using the standard resection method then SR recession was performed using fixed scleral sutures by an amount exceeding the resection. The amount of recession was determined based on the nomogram suggested by Tibrewal et al. [18] as follows; 6 mm SR recession for deviation less than 10 PD, 8 mm for DVD of 11-15 PD, 9 mm recession for DVD of 16-20 PD and 10 mm recession for DVD angle more than 20 PD. Bilateral symmetrical or asymmetrical recession was performed in cases of bilateral DVD while in cases of unilateral DVD with amblyopia more than 2 lines had received unilateral surgery.
For cases who received SR recession with posterior fixation sutures (group II), a limbal conjunctival incision was done with long perpendicular release incisions to maximize posterior exposure. Scleral sutures were taken on either side of the SR at a point 14 mm from the muscle insertion perpendicular to the muscle fibres using 5-0 polyester suture on a spatula needle and each suture had its exit from the lateral one third of the muscle at a point anterior to the scleral inlet by a distance equal to the planned recession but left untied.. The muscle was then recessed by the conventional fixed scleral sutures technique using double armed 6-0 vicryl sutures. The posterior fixation sutures were lastly tied on either sides of the recessed muscle leaving the middle one third of the muscle free from sutures to maintain its blood supply. The amount of recession ranged from 5 mm to 8 mm based on the measured preoperative DVD angle.
2.4. Outcome Measures
Follow up data were collected after 1 week, 1 month, 6 months,1 year then every 6 months thereafter .The minimum required follow-up was 18 months following the procedure.
The outcome measures were collected at the last follow up visit as follows;
The primary outcome measure was the surgical success rate which is identified as the percentage of patients with absent manifest DVD at the final follow-up visit following the procedure.
Secondary outcome measure was the amount of residual latent deviation measured by prism cover test with distant fixation at the final postoperative follow up visit. It was graded as excellent correction (≤ 4 PD), good (5-9 PD), fair (10-14 PD) and poor correction (≥15 PD).
Any reported intraoperative or postoperative complications were also included in the data analysis process.
2.5. Statistical Analysis
The distribution characteristics of quantitative variables were determined by Shapiro–Wilk test; normally distributed data were described using mean (standard deviation(SD)), while non-normally distributed data were described using median (interquartile range (IQR)). Independent samples T-test was used for analysis of normally distributed variables, while heterogenous variables were analysed using Mann-Whitney test. Qualitative data were analysed using Pearson’s chi-squared test. In all the tests, a P value of ˂ 0.05 was considered significant. Data analysis was performed using Statistical Package of Social Services, version 25 (SPSS) (IBM, 2017).
3. RESULTS
A total of 66 patients fulfilling the inclusion criteria were included for data analysis: 29 patients were treated by combined recession-resection of the SR muscle (Group I: combined recession-resection group), 37 patients were treated by SR recession with posterior fixation suture or faden. (Group II: recession with faden). The mean follow-up period for all patients was 22.6 ±4.6 months.
Table 1 shows the preoperative data of both groups with no significant detected differences.
Table 2 shows the operative data in both groups with significant differences between both groups regarding the amount of muscle recession as less recession was performed in the faden group. The recorded surgical time was significantly shorter in the combined recession-resection group.
Table 3 shows the median postoperative deviation and the postoperative success rate based on the absence of manifest deviation at the last follow-up visit. No statistically significant difference was found between both groups regarding the success rate. Figs. (1 and 2) show the postoperative correction in both groups based on the residual latent deviation with no detectable significant difference in both groups with p-value of 0.4 for the right eye (Fig. 1) and 0.8 for the left eye (Fig. 2). A logistic regression analysis was performed to ascertain the effects of possible confounders like age, gender, previous surgery, BCVA and preoperative angle of deviation on the surgical success and to control for this effect if present. None of the included variables proved to have a significant effect on the surgical success in either group as seen in Table 4.
| Variables |
Combined recession-resection (n=29) |
SR recession with faden (n=37) | P |
| Age (years): ▪ Mean ± SD |
12.4 ± 5.8 | 11.9 ± 5.5 | 0.8 |
| Sex: ▪ Male ▪ Female |
13 (45%) 16(55%) |
16 (43%) 21(57%) |
0.9 |
| BCVA in Log MAR [median (IQR)]: ▪ OD ▪ OS |
0.2(0.5) 0.2(0.3) |
0.2(0.3) 0.2(0.3) |
0.7 0.8 |
| ▪ Presence of amblyopia | 16 (55 %) | 18 (49 %) | 0.6 |
| ▪ Positive history of previous surgeries | 19 (66%) | 24 (65 %) | 0.9 |
| Preoperative angle of deviation(PD) [median (IQR)]: ▪ OD ▪ OS |
15(10) 18(9) |
18(6.5) 18(6.5) |
0.8 0.8 |
| Variable |
Combined recession-resection (n=29) |
SR recession with faden (n=37) | P |
| Amount of superior rectus recession (mm) ▪ OD ▪ OS |
8.8 ± 1.3 8.5± 2.2 |
6 ± 2.2 6.4± 2.2 |
<0.001* <0.001* |
| ▪ Symmetrical surgery | 8 (28 %) | 9 (24 %) | 0.8 |
| ▪ Surgical duration (min) | 19.1± 2.6 | 28.3± 4.7 | <0.001* |
| ▪ Variable |
Combined recession-resection (n=29) |
SR recession with faden (n=37) | P |
| ▪ Motor outcome: ▪ Success ▪ Under correction |
22 (76%) 7(24%) |
27 (73%) 10 (27%) |
0.8 |
| ▪ Postoperative deviation (PD)[median(IQR)] ▪ OD ▪ OS |
4(3) 4 (3) |
4(4) 4 (2) |
0.6 0.8 |
| Variables | 95% Confidence interval | P value | |
| Age | 0.925 | 1.216 | 0.4 |
| Gender | 0.06 | 1.709 | 0.2 |
| BCVA | 0.113 | 2.16 | 0.5 |
| Preoperative angle of deviation OD OS |
0.783 0.762 |
1.064 1.083 |
0.3 0.1 |
| Previous surgeries | 0.04 | 1.709 | 0.2 |
 |
Fig. (1). Motor outcomes of the studied groups based on the latent deviation OD in the last follow up visit (percentage from total). |
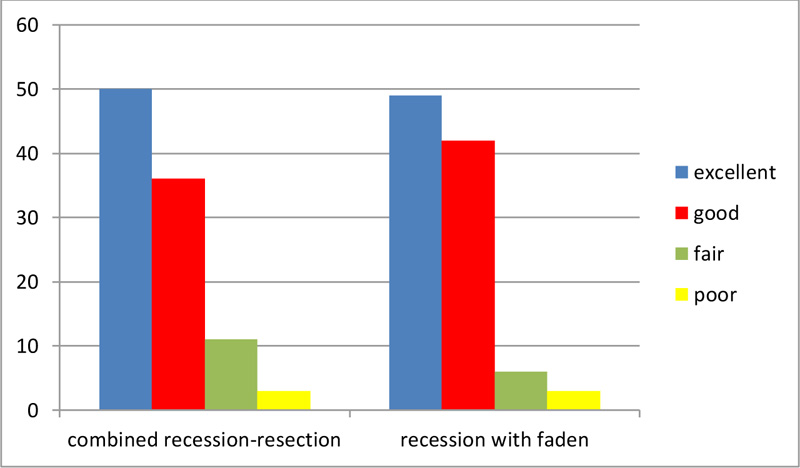 |
Fig. (2). Motor outcomes of the studied groups based on the latent deviation OS in the last follow up visit (percentage from total). |
The reported complication was limited elevation without hypotropia in 5 patients (2 in group I (7%) and 3 patients in group II (8%)). This limitation was mild and temporary, it disappeared in all patients by the end of the third postoperative month. Statistical comparison revealed no significant difference regarding the complication rate in both groups (p= 0.8). No recorded intraoperative complications were encountered in either groups, such as scleral perforation or lost muscle.
4. DISCUSSION
As there is no widely accepted surgery for the correction of DVD, the optimum surgical technique remains a matter of surgeon’s preferences and experience.
Many strabismus surgeons are more familiar with SR recession with posterior –fixation suture (faden) in cases of DVD. However, this technique requires generous posterior exposure with a risk of fat prolapse during posterior dissection, a challenging retro-equatorial positioning of sutures and an increased risk of scleral perforation, haemorrhage and difficult reversibility. Moreover, the tight muscle-fixing (myopexy) sutures could lead to the rare event of muscle necrosis [15]. Combined recession-resection of the SR carries the theoretical advantages of less need for the risky posterior dissection, less intraoperative sutures mess and subsequently less surgical time.
The combined recession-resection technique was introduced by Scott AB for the correction of incomitant ocular deviation [16]. Scott combined it with adjustable sutures in his first cases and many surgeons adopted this technique with variable modifications in cases of vertical and horizontal incomitant strabismus with promising results [17, 19-24].
The exact mechanism of action for combined-recession resection of a rectus muscle remains a matter of speculations. One theory is based on inactivating part of the muscle by resecting it thus changing its functional insertion. Another suggested mechanism is the interruption of the centrally driven incomitance by extirpation of the proprioceptive signals at the severed myotendinous junction [19, 25].
Creating a nomogram for combined recession-resection procedures was the main debate for many researchers. Due to variable indications of the procedure, no single nomogram was found to be reproducible for different conditions. The original technique performed by Scott recommended resection in an amount exceeding the recession [16]. On the other hand, Bhaskaran et al., Thacker et al., Roper-Hall and Cruz, suggested that the resection amount should be half that of the recession [19, 21, 26].
In esotropia with near distance disparity, the combined recession-resection of the medial rectus muscle was adopted by many surgeons with some modifications of the previously suggested amounts. While Somer et al and Ghali MA performed only a 2.5 mm resection with a recession amount based on the near angle of deviation [20, 24], Fermont et al. made an 8 mm recession with 6 mm resection of the medial rectus muscle [27].
No clear nomograms were found for this technique in cases of DVD. In this study, we chose to perform a 2.5 mm resection of the SR muscle combined with a recession based on the DVD angle. These measurements were based on the authors experience with the technique -unpublished data- and the results were satisfying to a great extent.
The effect of the combined recession-resection technique was believed to be more prominent in the medial and inferior recti [19], however, we found that the technique could be effective in the SR muscle, too with a success rate of 76% that is comparable to that of the superior rectus recession with faden (73%) and with no significant difference in the rate of complications. In the current study, the recorded surgical time was significantly shorter in recession- resection group with no need to increase posterior exposure to take the myopexy sutures. In our experience, using a single type of sutures in a combined recession-resection procedure made it technically easier and cost effective in comparison to SR recession with faden; a point of importance in low-income countries.
To the best of our knowledge, this is the first study to compare the results of combined recession –resection of the SR muscle in cases of DVD with those of SR recession with posterior fixation suture. The main limitation of the study is its retrospective design. Future prospective studies would offer more data regarding the possible surgical nomograms and the factors that could affect the final outcomes.
LIST OF ABBREVIATIONS
| SR | = Superior Rectus |
| DVD | = Dissociated Vertical Deviation |
| BCVA | = Best-Corrected Visual Acuity |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the research ethics committee of El-Fat’h Eye Hospital. Informed consent was obtained from all patients or their parents prior to surgery
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.







