RESEARCH ARTICLE
Outcome of Primary Management of Scleral Rupture without Vitrectomy Jakarta Eye Trauma Study
Gilbert W.S Simanjuntak1, 2, Biju Raju3, Golda A.M Simanjuntak1, Reinne Natali1, *
Article Information
Identifiers and Pagination:
Year: 2022Volume: 16
E-location ID: e187436412207220
Publisher ID: e187436412207220
DOI: 10.2174/18743641-v16-e2207220
Article History:
Received Date: 26/8/2021Revision Received Date: 18/1/2022
Acceptance Date: 23/2/2022
Electronic publication date: 22/09/2022
Collection year: 2022

open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
To report the outcome of primary management of scleral rupture without vitrectomy.
Methods:
Descriptive retrospective study of primary surgical management of scleral rupture located anterior to the equator. Initial and final visual acuity (FVA, intra ocular pressure, type of injury (sharp/blunt/projectile), wound length, time interval between the incident and primary repair and cause of injury were recorded. Encircling scleral buckle was placed in case of scleral laceration reaching muscle insertion. Patients who had a follow up of 3 months after the primary repair were included in the study .
Results:
There were 41 patients out of 78 who had scleral rupture anterior to the equator. The average age was 21.27 + 9.73 years (range 3-50 years). Thirty-three (80.4%) were males and eight (19.6%) were females. Rupture was located superiorly) in 28 (68.3%) patients, and inferiorly in 13 (31.7%) patients. Eight patients underwent encircling buckle. The time interval from the injury till the primary repair less than 8 hours (p 0.000) and 8-24 hours (p 0.000) were associated significantly with FVA improvements. Initial VA correlated with FVA improvement significantly (p 0.001). Two patients with initial VA of LP became NLP, and they had a wound length 11 mm and 12 mm respectively.
Conclusion:
The primary management of scleral rupture anterior to the equator, without vitrectomy, improves VA significantly. Time interval less than 24 hours and shorter wound length correlated with significant improvement of final VA.
1. INTRODUCTION
Open globe injury is a common cause of unilateral visual loss in the 20-45 years age group. Physical injuries to the eyes and periocular structures include lacerations, abrasions, foreign bodies, and open globe injuries, and can range from minor irritation to visual deterioration. Because they are in the productive age group, it’s important to manage visual impairment of open-globe injury properly. In a large study that included 5964 eyes out of 5799 patients, the average age was 35.5±21.8 years with a male-to-female ratio of 2.8:1. The most common age was in the 45-59 years age group [1]. Causalities of injury vary between each report and geographic area, but are mostly related to work, traffic accidents, playing/gaming, and others [1-5]. None of these studies focus on scleral rupture anterior to equator, which has a better prognosis compared to posterior sclera rupture.
The visual outcome varies between each report [1, 2, 6]. Severe open globe injury with a retained intraocular foreign body was associated with significant visual loss [7]. Familiarity with the various types of ocular and periocular injuries is important for all medical professionals and is critical to provide the most appropriate management [8].
It is important to clearly delineate the characteristics of patients who sustain open globe injuries anterior to the equator only, to better understand the associated factors related to visual outcome improvement and to ensure proper care. This study aimed to report the outcome of sclera tears anterior to the equator managed primarily without vitrectomy.
2. METHODS
This is a descriptive retrospective study done by collecting patients’ medical records with primary surgical management for scleral rupture, in a tertiary hospital in Jakarta from September 2018 to August 2020. The Christian University of Indonesia Institutional Ethics Committee approved this study following the tenets of the Declaration of Helsinki.
Slit lamp examination was done carefully to look for any significant anterior segment findings (conjunctiva tear, hyphema, afferent pupillary defect, and depth of anterior chamber). Initial and final Visual Acuity (VA) (improvement if final VA gains 2 lines or more), eye movement, intraocular pressure, type of injury (sharp/blunt/projectile), wound length, and cause of injury were recorded. If there were media opacities (severe corneal edema, cataract and/or vitreous hemorrhage) and suspicion of intraocular foreign body, a B-scan examination was done with minimal pressure to the eyeball and/or an orbital X-ray. Time intervals between injury, surgical management and follow-up duration were also recorded. Cases of scleral rupture anterior to the equator were included in this study. Cases with corneal rupture without scleral rupture or scleral rupture reaching the equator or/and extended posterior to the equator were excluded.
Surgical management was done under general anesthesia once the patient was fit for surgery. Conjunctiva was incised to explore the length of scleral rupture. End-to-end length of the sclera rupture was measured using a caliper. Sclera and conjunctiva were sutured with 8.0 Vicryl. An encircling scleral buckle was placed if the scleral rupture extended posteriorly to the muscle insertion. All procedures were done after obtaining a thorough informed consent, including possibilities of evisceration or enucleation.
During the preparation for surgery, the eye was patched. Systemic Gentamycin was given intravenously and topical Gentamycin eye drops were instilled hourly in the affected eye. After surgery, the systemic antibiotic was continued for three days, and topical antibiotics along with topical steroids (Prednisolone Acetate) were started and gradually tapered off. Patients who completed the 3 months follow-up visit were included in the analysis. SPSS version 24.0 (SPSS, Inc., Chicago, IL) was used for all statistical analyses, and P < 0.05 was considered significant.
3. RESULTS
Among the 78 patients with scleral rupture, 30 patients were excluded as the tear extended posteriorly to the equator. None of the patients had a history of previous eye surgeries. 7 patients refused surgery. 41 eligible patients had scleral rupture not reaching the equator during surgical exploration; 33 (80.4%) male and 8 (19.6%) female. There were 25 (60.97%) patients with cornea-scleral wounds. None of the eligible subjects had a retinal detachment.
The average age was 21.27 + 9.73 years (range 3-50 years), and a total of 75.5% were aged 11-30 years. A total of 64.4% presented with initial visual acuity of less than 3/60. Blunt trauma was the cause of scleral rupture in 53.6% of cases, 43.2% due to sharp force trauma, and 12.3% from projectile trauma. The incidence of trauma at home was 43.9%, a more frequent occurrence than in other places, trauma in the workplace 29.3%, and from traffic accidents 26.8%. The incident in the workplace was in 58.3% due to fights/assault.
B-scan ultrasonography was carried out in 17 (41.5%) of cases with obscured optical media and showed vitreous hemorrhage in nine cases (21.9%) and subretinal hemorrhage in two cases (4.9%). In 37 (90.2%) cases with a suspected orbital fracture, X-ray examination was done but was negative.
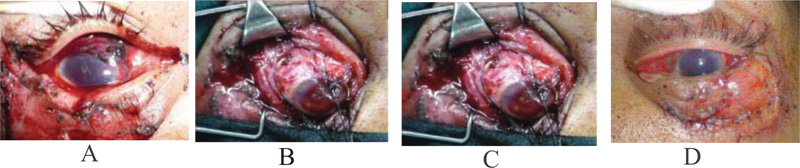
After conjunctival incision and wound exploration, the scleral rupture was seen superiorly (medial or temporal) in 28 (68.3%) patients, and inferiorly (medial or temporal) in 13 (31.7%) patients. Eight patients underwent encircling buckle, as the rupture extended posteriorly to muscle insertion. Cataract extraction was done in 15 cases. Wound length varied between 2-12 mm and the shape of the wound was mostly irregular. Wound length significantly correlated with improved final VA (p 0.01, CI 0.009 – 0.015). None of the cases underwent vitrectomy at the time of primary repair (Fig. 1).
Twenty-two patients (53.6%) underwent surgery less than 8 hours after the injury occurred, 15 (36.6%) underwent surgery 8 to 24 hours after the injury, and 4 (12.2%) were operated on more than 24 hours after the injury. Most of the patients came to the hospital less than 24 hours after injury (90%). Time interval (less than 8 hours and 8-24 hours) from the incident till the primary repair was associated significantly with final VA improvements (p 0.000 and 0.000 respectively). The average follow-up of patients was 23 weeks (range 12 – 43 weeks).
Initial VA was 0.12 + 0.249 and final VA was 0.23 + 0.314 and improvement in Visual Acuity (VA) was statistically significant (p 0.001). There were 29 (70.8%) patients presenting with 6/60 or worse, and 9 (21.9%) patients with VA 6/6 to 6/60. Three (7.3%) patients presented with No Light Perception (NLP) their time to present to the emergency room varied from < 8 to 24 hours and the wound length varied from 2 to >10 mm. Two patients with initial VA of LP had an unfavorable outcome after primary repair with a final visual acuity of NLP. These 2 patients had a larger wound length - 11 mm and 12 mm respectively. In the final VA distribution, there were 21 (51.2%) patients with VA 6/60 or worse and 19 (46.3%) patients with VA 6/6 – 6/60. Presenting clinical characteristics, wound size and interval between the time of injury to surgical intervention are shown in Table 1.
| Presenting Clinical Characteristic | n | % |
| - Reduced VA | 39 | 95 |
| - Decreased IOP | 30 | 73.2 |
| - Hyphema | 25 | 61 |
| - Conjunctival chemosis | 10 | 24.4 |
| - Conjunctival rupture | 31 | 75.6 |
| - Traumatic cataract | 3 | 7 |
| Initial Visual Acuity | ||
| - 6/12 or better | 3 | 7.3 |
| - 6/15 to 6/60 | 6 | 14.6 |
| - 6/60 or worse | 29 | 70.8 |
| - No light perception | 3 | 7.3 |
| Wound length | ||
| - Less than 3 mm | 11 | 26.8 |
| - 3 -5 mm | 19 | 46.3 |
| - 6 -9 mm | 6 | 14.6 |
| - More than 10 mm | 5 | 12.3 |
| Interval between injury and surgery | ||
| - Less than 8 hours | 22 | 53.6 |
| - 8 – 24 hours | 15 | 36.6 |
| - More than 24 hours | 4 | 9.8 |
4. DISCUSSION
Serious eye injury is common in clinical practice, often causing great damage to visual function, resulting in poor visual and anatomic outcomes despite surgical intervention [9]. Scleral rupture is more common at younger age and mostly occurs among males. In this study, most patients were between the ages of 11-30 years (75.5%), the average age was 36 years and 84% were male. Male predominance is a universal characteristic and has been demonstrated in several studies in different countries [1, 5, 7, 10].
In this study, the domestic accident was found in almost half of the total patients, followed by the workplace accident. Though similar findings were reported from Malaysia, workplace-related injuries accounted for most of the ocular injuries (41.4%), followed by motor vehicle accidents (25.7%), domestic accidents (22.4%), assault (7.9%), sports accidents (2.0%), and school-related accidents (0.6%). In their study 39 patients (25.7%) sustained injuries associated with organic matter, and none were found in our subjects [11].
A thorough initial examination helps in the formulation of the primary management plan and to determine the prognosis. The open globe injury prognostic model demonstrated predictive accuracy and can be useful in counseling patients and making clinical decisions regarding open globe injury management [12]. Several other prognostic methods are also available such as the Ocular Trauma Classification Group, Regression tree analysis, and methods that perform intraocular cultures on open globes injury [12-14]. The Ocular Trauma Study (OTS) group evaluated more than 2500 ocular injuries associated with non-combat causes and formulate a methodology to predict the final visual outcome at the time of initial injury [15]. Whenever the eyeball cannot be salvaged on the operating table, evisceration or primary enucleation was performed [16]. In this study, thorough informed consent was obtained from all the patients, but none underwent evisceration or primary enucleation.
Initial visual acuity of NLP after ocular trauma does not mean permanent visual loss as reported in the past. Even in severe eyeball laceration, early intervention of vitrectomy combined with silicone oil tamponade to achieve retinal reattachment may make the severely traumatized eyes regain the VA of LP or better. Unfortunately, three eyes in our series that presented with NLP did not improve after primary management.
Though vitrectomy was not part of the primary repair in this case series, Vitrectomy was still needed in cases of non-clearing vitreous hemorrhage as seen in several cases. The timing to do vitrectomy is debatable; some surgeons prefer to do it between 10 - 14 days; waiting for vitreous detachment can simplify the surgical procedure.
At presentation, 95% of patients had decreased VA and 73.2% of patients had decreased IOP. The most common cause of a decreased VA in eye trauma was myopic shift due to lens thickening and anterior chamber shallowing, which recovers spontaneously as time passes. Therefore, conservative management would be a good choice for managing eyes with blunt trauma in an emergency department, especially when there is no suspicion of eyeball rupture [17-22]. In this study, the initial VA was mostly below 6/60 (70.8%) and there were three cases (7.3%) with NLP vision. The defective vision was either due to the structural damage to the anterior segment including hyphema in 25 cases (61%), and traumatic cataract in 3 cases (7%); or because of posterior segment disorders such as vitreous hemorrhage in 9 cases (21.9%), and subretinal bleeding in 2 cases (4.9%). Other notable clinical presentations were the presence of conjunctival chemosis (24.4%) and conjunctival rupture (75.6%).
By the ocular ancillary examination, there were 21.9% of patients with vitreous hemorrhage, without intraocular foreign body. Other studies showed that the presence of intraocular foreign body and retinal detachment are poor prognostic indicators [10, 12]. Although the presence of an IOFB alone was not a statistically significant prognostic factor, retained IOFB in combination with posttraumatic endophthalmitis was associated with a particularly poor visual outcome [14, 22-24].
In this study, 73.1% of cases had a wound size of 5 mm or less. This was similar to zone II the Ocular Trauma Classification Group and was related to a better prognosis than zone 3. Zone 3 injuries involved full-thickness scleral defects more than 5 mm posterior from the limbus. The wound location and size described the extent of damaged tissue and were associated with the prognosis [3, 7, 12]. There were two cases with 11-12 mm wide wounds that came with LP vision that became NLP after the primary management. Wounds that are longer than 10 mm for example, even if did not reach the rectus muscle insertion, can be a poor prognostic factor. The possibility of giving steroids to suppress the inflammation may be considered, in order to prevent total blindness and phthisical eye in such eyes.
In this study, the interval between injury and surgery was less than 8 hours in 53.6% of cases. Some studies suggested that the delay in primary repair increases the risk of post-traumatic endophthalmitis. Studies on post-traumatic endophthalmitis showed the following as protective factors: early primary repair, intraocular tissue prolapse, and self-sealing wound [1, 11, 14]. There were 4 cases (9.8%) who underwent surgery after more than 24 hours, but none had endophthalmitis. The incidence of endophthalmitis can be reduced by the administration of intravenous antibiotics before surgery [15, 21]. Sympathetic ophthalmia (SO), which is a devastating, though uncommon, bilateral granulomatous pan uveitis following uveal trauma to one eye. The prevalence of SO after eye injury is estimated to be between 0.1% and 0.3%. Due to its very low incidence, it is controversial whether SO can be prevented by removing the eye after trauma. The prevention of SO by evisceration or enucleation is controversial [20, 22, 25].
In the setting of a severely ruptured or lacerated globe with gross prolapse and/or loss of retinal and uveal tissue, primary enucleation is a valid alternative to primary repair with anticipated secondary enucleation. Considerations include the status of the fellow eye, the opportunity for patient and/or family counseling and consent, and the patient’s medical status [15, 18, 19, 25].
LIST OF ABBREVIATIONS
| VA | = Visual Acuity |
| OTS | = Ocular Trauma Study |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The Christian University of Indonesia Institutional Ethics Committee granted approval for this study.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research. All the humans used were in accordance with the Helsinki Declaration of 1975.
CONSENT FOR PUBLICATION
Informed consent has been obtained from the participants involved.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.