All published articles of this journal are available on ScienceDirect.
Ophthalmic Surgical Cancellations in a Tertiary Hospital over a 10-year Period: Analysis of Patient Characteristics and Cancellation Reasons
Abstract
Objective:
To evaluate causes and demographic associations for ophthalmic surgical cancellations in a tertiary hospital in New Zealand over a 10-year period.
Methods:
All ophthalmic surgical cancellations were identified using electronic records between 1 Jan 2010 and 31 Dec 2019. The reasons for cancellations and association with the calendar year, patient age, gender, ethnicity, and driving distance to the hospital were analysed.
Results:
A total of 20,934 surgical bookings were identified over the 10-year period with overall cancellation and day-of-surgery cancellation (DOSC) rates of 21.2% (n=4447) and 6.8% (n=1416) respectively. The most common cancellation reasons included ‘Substitution/List Overrun’ (24.2%), ‘Not Specified’ (23.3%), and ‘Acute Illness’ (17.7%). Cancellations were reduced and total surgical bookings increased over the study period.
Māori accounted for 18.3% of bookings, with a total cancellation rate of 24.5% and a DOSC rate of 9.0%. Māori had a mean age of 54.2 years compared to 66.7 years for non-Māori.
Conclusion:
A large proportion of DOSCs were due to list overrun and substitution for emergency cases, consistent with reports from Australia, India, South Africa, and Hong Kong. Reducing surgical cancellations (particularly DOSCs) has the potential to significantly improve theatre utilisation and surgical capacity with minimal increases in costs.
Māori were underrepresented in surgical bookings, overrepresented in cancellations and DOSCs, and were significantly younger at the time of surgery than non-Māori. Targeted strategies to reduce cancellations for Māori will enable more equitable access to ophthalmic surgery.
1. INTRODUCTION
Healthcare systems are being stretched to keep up with the increasing demand for surgical services. This is common to most surgical specialties, including ophthalmology, and is fuelled partly by an ageing population with greater health needs [1-3].
Operating theatre efficiency is critical to maximise service provision within budgetary constraints. Factors commonly resulting in underutilised theatre time include delayed session start, sub-optimal case mix, delays in turnaround between cases, and short notice cancellations [4-7]. Operating theatre efficiency guidelines are nowcommonplace in most healthcare systems and typically employ a multi-pronged approach to efficient theatre management, with a focus on improving turnaround and start times and consideration for case-mix planning [8, 9].
Surgical cancellations are associated with inefficient use of operating theatre time and are a major source of inefficiency for healthcare systems worldwide [4-7]. At the patient level, unexpected cancellations are associated with patient distress and adverse clinical outcomes [6, 10]. Identifying the reasons for surgical cancellations is critical to understanding how operating theatre utilisation can be improved.
This study is a retrospective review of all ophthalmic surgical bookings at Waikato Hospital for the decade from 1 January 2010 to 31 December 2019. Waikato Hospital is based in Hamilton, New Zealand, and provides government-funded healthcare services to a geographic area of 21,000km2 and a population of over 435,000 [11]. The Waikato region includes subpopulations with high socioeconomic deprivation, rural location of domicile, and a relatively high proportion of people of (indigenous) Māori ethnicity. Māori face additional barriers to accessing healthcare in New Zealand and typically have poorer health outcomes, greater disease burden, shorter life expectancy and are known to present with more advanced ocular pathology at a younger age than non-Māori [12, 13].
2. MATERIALS AND METHODS
The study was initiated after it was reviewed and approved by the Waikato Hospital Clinical Audit Support Unit and adheres to the guidelines of the 1975 Declaration of Helsinki, as revised in 2013. All ophthalmic surgical bookings, theatre events, and cancellations at Waikato Hospital were reviewed for surgical procedures scheduled between 1 January 2010 to 31 December 2019. Records were extracted from the Waikato Hospital online theatre booking database. The analysis included all elective and acute bookings within the study period, with the exception of bookings identified as being made in error or those cases that were rebooked to an earlier date. Statistical analysis was completed using the R statistical software package and Microsoft Excel [14, 15].
The extracted data included scheduled and actual surgery start and end date/time, procedure name, anaesthetic type, patient date of birth, domicile, and ethnicity. Additional data were collected for cancelled cases and included cancellation date/time, reason, and a free-text comment field (see supplement 1 for the de-identified dataset).
A surgical cancellation was defined as any case where a booking, for any reason, did not result in the intended surgery on the specified date. A day-of-surgery cancellation (DOSC) was defined as any cancellation that occurred on the intended surgery date itself.
The reasons for cancellation were categorised for analysis. Cancellations due to lack of available theatre time either by list overrun or by addition of an acute case were categorised as ‘Substitution/List Overrun’. Cancellations due to lack of availability of hospital staff including nurses, surgeons and anaesthetists were categorised as ‘Hospital Staff’. Cancellations due to cancellation of the entire theatre session, unavailability or malfunction of the necessary equipment, or where no inpatient bed was available postoperatively were categorised as ‘Hospital Systems’. Cancellations due to patient unavailability on the specified surgical date for non-medical reasons such as work/childcare commitments, unwell family members, or where transport was not available were categorised as ‘Transport/Logistical'. Cancellations categorised as ‘Inadequate Workup’ included those due to pending laboratory and radiology results, improper preoperative fasting, inadequate preoperative optimisation, unacceptable preoperative blood pressure or blood glucose levels, or due to antithrombotic medication issues. The remaining categories included: ‘Did Not Attend’, ‘Surgery No Longer Required’, and ‘Patient Acutely Unwell’. Cancellation categories were analysed by age, gender, ethnicity (with particular attention to outcomes for Māori), calendar year, and commute distance from patient domicile to Waikato Hospital.
3. RESULTS
3.1. Overview and Baseline Patient Characteristics for Bookings and Cancellations
A total of 21,592 ophthalmology surgical bookings were identified over the study period. Of these, 658 bookings were identified as being made in error or being rebooked to an earlier date and were excluded from analysis. The baseline patient characteristics of the remaining 20,934 bookings were noted with a comparison between cancelled and non-cancelled cases, as summarised in Table 1. The 4,447 cancellations (21.2% of all bookings) included 1,416 DOSCS (6.8% of all bookings).
| - | Cancelled | Not Cancelled | Total |
|---|---|---|---|
| n (%) | 4,447 (21.2%) | 16,487 (78.8%) | 20,934 |
| Sex, n (% of subgroup) | - | - | - |
| Male | 2,078 (46.7%) | 8,099 (49.1%) | 10,177 (48.6%) |
| Female | 2,369 (53.3%) | 8,388 (50.9%) | 10,757 (51.4%) |
| Ethnicity, n (% of subgroup) | - | - | - |
| Māori | 940 (21.1%) | 2,892 (17.5%) | 3,823 (18.3%) |
| Non-Māori * | 3,507 (78.9%) | 13,595 (82.5%) | 17,102 (81.7%) |
| Mean Age, years (SD) † | 64.6 (20.7) | 64.3 (21.2) | 64.4 (21.1) |
| Mean Commute Distance, km (SD) | 68.6 (93.0) | 64.0 (80.0) | 65.0 (82.9) |
†Patient age on the date of intended surgery.
The difference in mean age between cancelled and non-cancelled cases was not statistically significant by Welch Two Sample t-test (t = 0.9429, df = 7,145.3, p-value = 0.3458). The mean commute distance was 4.6km greater for cancelled cases in comparison to non-cancelled cases and was statistically significant by Welch Two Sample t-test (t=3.0321, df = 6,330.2, p-value = 0.002).
3,823 bookings (18.3%) were for Māori. Approximately 99,300 Māori reside in the Waikato District Health Board region and make up 22.8% of the population [11]. The proportion of bookings for Māori was significantly lower than expected based on population proportion (chi-squared = 252.44, df = 1, p-value <0.001).
3.2. Age Differences between Gender and Ethnicity Subgroups
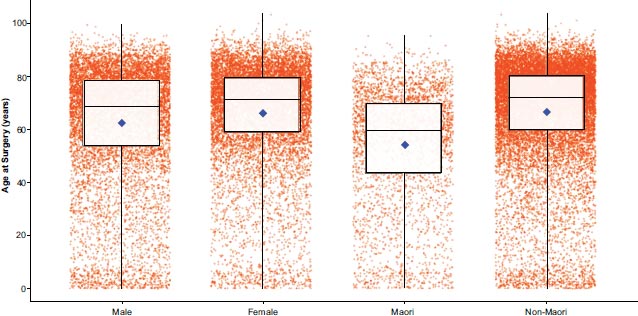
The mean age at the time of intended surgery among Māori was 54.2 years and the median age was 59.7 years, compared to a mean age of 66.7 years and a median age of 72.1 years among non-Māori. The difference in mean age between Māori and non-Māori was statistically significant by Welch Two Sample t-test (t = -32.252, df = 5366.6, p-value < 2.2e-16). 10,177 bookings were for Males with a mean age at the time of intended surgery of 62.5 years and a median age of 68.4 years. 10,757 bookings were for Females with a mean age of 66.2 years and a median age of 71.3 years. The difference in mean age between Males and Females was statistically significant by Welch Two Sample t-test (t = -12.811, df = 20,379, p-value < 2.2e-16). The age distribution of bookings by gender and ethnicity group are shown in Fig. (1).
3.3. Annual Changes in Cancellation Rates
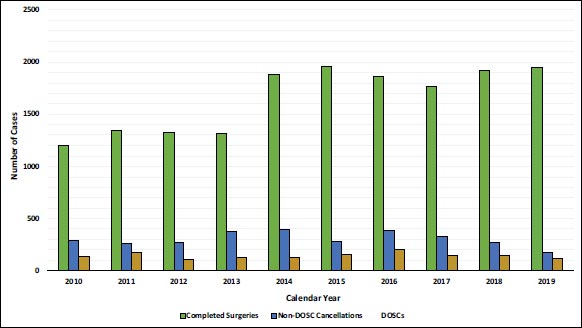
The annual cancellation rates and DOSC rates decreased over the study duration with the cancellation rate falling from 26.0% to 12.8% (chi-squared=109.01, df=1, p value < 0.001) and the DOSC rate falling from 8.2% to 5.1% (chi-squared=15.49, df=1, p value <0.001) between 2010 and 2019. Surgical bookings increased by 38% and the total number of completed surgical procedures increased by 62% over the study duration as outlined in Fig. (2).
3.4. Reasons for Cancellations and Day of Surgery Cancellations
The most common reasons for all cancellations were ‘Substitution/List Overrun’ (n= 1,078, 24.2% of all cancellations), ‘Not Specified’ (n= 1,035, 23.3%) and ‘Acute Illness’ (n= 787, 17.7%), followed by ‘No Longer Required’ (n= 597, 13.4%), ‘Hospital Staff’ (n= 312, 7.0%) and ‘Incomplete Workup’ (n= 219, 4.9%). Only 29 cases (0.65%) in the ‘Incomplete Workup’ category were cancelled due to anticoagulant or antiplatelet-related issues, while a further 29 cases were cancelled due to blood pressure-related concerns. A total of 12 cases (0.27%) were cancelled due to blood glucose-related concerns. In total; anti-thrombotic, blood pressure and blood glucose-related issues accounted for 1.6% of all cancellations. ‘Did Not Attend’ resulted in 152 cancellations (3.4%) while ‘Hospital Systems’ resulted in 134 (3.0%) and ‘Transport/Logistics’ resulted in 133 (3.0%) cancellations.
The most common reasons for DOSCs were ‘Substitution/List Overrun’ (n= 433, 30.6% of all DOSCs) and ‘Acute Illness’ (n= 273, 19.3%) followed by ‘Not Specified’ (n= 146, 10.3%), ‘Hospital Staff’ (n= 146, 10.3%), ‘No Longer Required’ (n= 140, 9.9%), ‘Did Not Attend’ (n= 119, 8.4%), ‘Incomplete Workup’ (n= 108, 7.6%), ‘Hospital Systems’ (n= 28, 2.0%) and ‘Transport/Logistics’ (n= 23, 1.6%). Within the ‘Incomplete Workup’ group, only 21 DOSCs (1.5%) were due to antiplatelet/anticoagulant concerns, while only 26 (1.8%) were due to blood pressure and only 8 (0.57%) due to blood glucose.

| - | Bookings, n | Cancellations, n (rate) | DOSCs, n (rate) |
|---|---|---|---|
| Male | 10,177 | 2,078 (20.4%) | 702 (6.9%) |
| Female | 10,757 | 2,369 (22%) | 714 (6.6%) |
| Māori | 3,832 | 940 (24.5%) | 343 (9.0%) |
| Non-Māori* | 17,102 | 3,507 (20.5%) | 1,073 (6.3%) |
| Total | 20 934 | 4 447 (21.2%) | 1 416 (6.8%) |
*Non-Māori group defined as all patients not identifying as New Zealand Māori.
3.5. Cancellation Rates between Demographic Subgroups
Total bookings, total cancellations, cancellation rates, total DOSCs, and DOSC rates for gender and ethnicity subgroups are detailed in Table 2 below. Females had a significantly higher cancellation rate than Males (chi-squared = 8.04, df = 1, p-value < 0.05) though the DOSC rate between Males and Females was not significantly different (chi-squared = 0.562, df = 1, p-value = 0.453). Māori had a significantly higher Cancellation rate (chi-squared = 35.57, df = 1, p-value < 0.001) and DOSC rate (chi-squared = 30, df = 1, p-value < 0.001) than non-Māori.
3.6. Comparison of Cancellation Reasons between Māori and Non-Māori
Māori had significantly higher overall cancellation rate than non-Māori due to ‘Acute Illness’ (5.27% vs. 3.42%, chi-squared= 29.64, df=1, p <0.001), ‘Did Not Attend’ (1.72% vs. 0.50%, chi-squared= 64.59, df=1, p <0.001) and ‘Incomplete Workup’ (1.38% vs. 0.97%, chi-squared= 5.14, df=1, p< 0.03). Māori also had significantly higher DOSC rate than non-Māori due to ‘Acute Illness’ (2.35% vs. 1.07%, chi-squared= 39.76, df=1, p <0.001), ‘Did Not Attend’ (1.33% vs. 0.40%, chi-squared= 48.24, df=1, p <0.001) and ‘Not Specified’ (1.02% vs. 0.63%, chi-squared= 6.95, df=1, p< 0.01). Cancellation and DOSC rates due to all other reason categories were not significantly different between Māori and non-Māori, as outlined in Fig. (3).
| - | GA Bookings, n | GA Cancellations, n (rate) | GA DOSCs, n (rate) |
|---|---|---|---|
| Māori | 1,284 | 279 (21.7%) | 94 (7.3%) |
| Non-Māori* | 3,944 | 700 (17.8%) | 236 (6.0%) |
| Total | 5,228 | 979 (18.7%) | 330 (6.3%) |
*Non-Māori group defined as all patients not identifying as New Zealand Māori.
3.7. Cancellation Rates for General vs. Local Anaesthetic Cases
Of the 20,934 surgical bookings during the study period, 5,228 (25.0%) were planned/completed under general anaesthetic (GA). GA bookings, cancellations and DOSCs are listed in Table 3. The overall cancellation rate for GA cases was 18.7% while the DOSC rate was 6.3%. The overall cancellation rate for local anaesthetic (LA) cases was 22.1% while the DOSC rate was 6.8%. The overall cancellation rate was significantly lower for GA cases compared to LA cases (chi-squared= 26.384, df=1, p <0.001). This trend was also found when comparing GA cases and LA cases among Māori (chi-squared= 8.185, df=1, p= 0.0042) and among non-Māori (chi-squared= 23.918, df=1, p <0.00001). There was no statistical difference in the overall DOSC rate between GA cases and LA cases (chi-squared= 1.543, df=1, p =0.214) or between GA and LA cases among Māori (chi-squared= 2.859, df=1, p=0.091) or among non-Māori (chi-squared= 0.735, df=1, p=0.391).
4. DISCUSSION
Surgical cancellations result in underutilised theatre time, reduced surgical throughput, and reduced patient access to surgical services [8, 9]. Reducing cancellations (particularly DOSCs) is a cost-effective strategy to improve efficiency and accommodate the increasing demand for surgery. This retrospective study analysed all ophthalmic surgical bookings and cancellations including DOSCs at a government-funded tertiary hospital over a 10-year period prior to the effects of the Covid-19 pandemic. Reasons for cancellation, anaesthetic type, and patient demographics including ethnicity and commute distance were analysed.
The findings of the current study are likely generalisable to other similar government-funded healthcare systems such as the National Health Service in the United Kingdom but may have reduced applicability to other healthcare systems. Despite this, many findings in the current study are consistent with trends in other healthcare systems. Surgical bookings increased over the duration of the study with a reduction in cancellations and DOSCs. Similar increases in surgical demand and throughput have been noted in Australia, UK, and USA [3, 16, 17]. The most common reasons for cancellations and DOSCs in the current study were ‘Substitution/List Overrun’, ‘Acute Illness’, and ‘Not Specified’. This trend is consistent with findings in studies in Australia, India, South Africa, and Hong Kong [4, 5, 18, 19].
Surgical cancellations (particularly DOSCs) decrease operating theatre efficiency and can cause significant disruption for patients. In most cases, DOSCs require rescheduling which consumes administrative resources and causes considerable inconvenience for patients [8, 9]. Last-minute cancellations are associated with significant patient anxiety and psychological distress [6, 10]. Patients requiring elective surgery often have to wait several months and make arrangements at home and work, and in some cases alterations to medications and diet, to prepare for surgery. In the current study, the most common reason for DOSCs, accounting for one in four cancellations, was ‘Substitution/List Overrun’. Methods to accommodate acute cases without cancelling elective cases, such as staffing arrangements and overtime pay structures that enable afternoon theatre lists to run late if acute cases are added would provide a more patient-centred solution. However, variable staff availability and the increased costs associated with such an approach must also be considered [20].
Suboptimal control of blood pressure, blood glucose and anticoagulant medications accounted for a relatively small number of cancellations in the current study. This contrasts with the findings of a similar study in Kuwait [21]. There is currently no consensus on evidence-based guidelines for acceptable thresholds for pre-operative blood pressure, blood glucose, and anticoagulant levels for ophthalmic surgery. Several studies have reported no reduction in operative or systemic complications from withholding anticoagulants, optimising blood pressure, or blood glucose prior to surgery [22-25]. Although postoperative cystoid macular oedema is more common in diabetics that may have suboptimal blood glucose control, this can be managed with post-operative topical non-steroidal anti-inflammatory (NSAID) medication. The use of topical NSAIDs may be preferable to rapid glycaemic correction for patients with poorly controlled diabetes as rapid improvements in glycaemic control have been associated with the progression of diabetic retinopathy and maculopathy [24, 26-28]. A lower cancellation rate among GA cases suggests greater attention to preoperative workup and optimisation in such cases compared to LA cases.
Unexplained non-attendance at preoperative and surgical appointments is a preventable source of cancellations and DOSCs both in this study and in other healthcare systems [29, 30]. Other authors have proposed measures to reduce non-attendance including additional text, phone or email reminders prior to appointments as well as changing the content of text reminders to include information such as cost to the healthcare system for a missed appointment or surgery [6, 31, 32]. Other simple prevention strategies include calling patients two or three days prior to planned surgery to check wellness and intention to proceed with surgery, allowing early identification of patients who are acutely unwell or who no longer plan to attend. Machine learning models have demonstrated effectiveness in predicting patient non-attendance in New Zealand and other healthcare systems [33, 34]. By employing such models, patients at high risk of non-attendance could be identified, enabling departments to employ tailored prevention strategies targeted toward these patients. Another suggested strategy is to perform a preadmission workup at the time of listing for surgery and to ensure every patient has clear written instructions on preoperative investigations, medications, and fasting protocols. This has previously been demonstrated to reduce cancellations due to incomplete work-up [35]. Transport difficulties were attributed to only a small percentage of cancellations in the dataset. However, the significantly greater mean commute distance among cancellations suggests that transport difficulties may have contributed to cancellations that were recorded under other reasons such as unexplained non-attendance.
Māori in the current study were underrepresented in ophthalmic surgical bookings, had a significantly higher cancellation and DOSC rate, and were significantly younger on average than non-Māori. These findings are consistent with published trends in Māori health outcomes [12, 13]. Higher rates of cancellation due to acute concurrent illness in the current study were likely due to the greater comorbid disease burden among Māori while significantly higher non-attendance-related cancellations for Māori are in line with findings from previous studies assessing attendance at outpatient clinics [12, 36, 37]. Factors underlying disparities between Māori and non-Māori outcomes in the current study are likely similar to those identified by previous authors and include lower socioeconomic status, poorer health literacy, and poorer access to resources among Māori. Further complex factors may include cultural and historic effects of colonisation, racism, and marginalisation which present additional barriers to healthcare access [38-40]. Any interventions aimed at reducing cancellations due to acute illness and non-attendance will likely be of particular benefit in reducing cancellation rates for Māori. The healthcare system continues to work in active partnership with Māori to accommodate Māori cultural practices (Tikanga) with the aim of achieving more equitable outcomes [41, 42].
The current study was not without limitations. The data were collected retrospectively from electronic theatre records. Different staff members may have coded the cancellation reasons inconsistently when multiple factors led to a cancellation. In some cases, a specific reason for cancellation was not documented, though the majority of cancellation reasons were retrievable through free-text fields, and a specific cancellation reason was found in the vast majority of cases.
CONCLUSION
Surgical cancellations are a major source of inefficiency, consume health resources, and have significant negative consequences for patients. Improved strategies to accommodate acute cases, the most common reason for cancellations, would provide better patient-centred care. Māori are underrepresented in surgical bookings despite generally presenting with more advanced pathology and are also overrepresented in cancellations and DOSCs, particularly due to non-attendance and concurrent acute illness. Interventions to reduce cancellations and DOSCs will improve access for Māori, though targeted strategies will likely be needed to achieve a more equitable outcome. Interventions aimed at reducing surgical cancellations and DOSCs due to avoidable factors such as non-attendance and the establishment of evidence-based guidelines for the management of blood pressure, blood glucose, and anticoagulant medications may reduce unexpected cancellations and significantly increase theatre utilisation, surgical capacity, and patient access to surgery with little to no increase in resource requirements.
LIST OF ABBREVIATIONS
| DOSC | = Day-of-surgery Cancellation |
| NSAID | = Non-steroidal Anti-inflammatory |
| DOSCs | = Day of Surgery Cancellations |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was initiated after it was reviewed and approved by the Waikato Hospital Clinical Audit Support Unit.
HUMAN AND ANIMAL RIGHTS
No animals were used for this study. This study did not involve any active human participants. Passive human participation in the form of accessing retrospective patient records was conducted in accordance with the ethical standards of the Waikato Hospital Clinical Audit Support Unit which approved the study and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
No identifiable patient data has been included in this publication and therefore specific patient consent for publication does not apply.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
STANDARDS OF REPORTING
STROBE guidelines were followed.
CONFLICT OF INTEREST
The authors report no conflict or competing interests to declare (financial or otherwise).
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors and this research was not part of any author’s paid employment duties.
ACKNOWLEDEGMENTS
Declared none.
SUPPLEMENTARY MATERIAL
Original Excel dataset with all patient-identifiable information removed.


