All published articles of this journal are available on ScienceDirect.
Laser Vitreolysis for Vitreous Opacities: A Prospective Study
Abstract
Aim:
The aim of this study is to evaluate the efficacy and safety of a YAG laser vitreolysis procedure used to remove bothersome vitreous opacities/floaters.
Methods:
The prospective clinical study included 42 eyes of 35 patients (age 32-81 years) with vitreous opacities generating visual disturbances. All patients were treated using the Ellex - Ultra Q Reflex YAG laser and underwent a complete eye examination before the laser vitreolysis and at 1, 3 and 6 months after the intervention. Changes in corrected distance visual acuity (CDVA), central retinal thickness (CRT), intraocular pressure (IOP) and patient’s subjective perception of disturbances were analysed.
Results:
The average number of laser shots was 118 (6 - 310 shots), with a total average energy of 3.8 mJ per laser shot (2.2 - 9 mJ). The laser intervention was performed only once in a total of 31 eyes (73.8%), whereas it was necessary to perform the intervention twice in 10 cases (23.8%). No significant differences in CDVA were detected during the whole follow-up (p>0.40). No significant changes were found either in CRT (p>0.32). Concerning IOP (p<0.001), it was reduced significantly immediately after the intervention, returning to the pre-intervention level afterwards. The analysis of the responses to the questionnaire revealed that there was a mean improvement in subjective visual symptoms according to patients of 71%. No complications were detected in the sample during the follow-up.
Conclusion:
Laser vitreolysis is a minimally invasive treatment, allowing a complete or partial elimination of vitreous opacities and leading to alleviation of patient’s disturbances.
1. INTRODUCTION
The vitreous body, under physiological conditions, is a transparent intraocular gel consisting of more than 98% water. Besides water, it contains a fine network of collagen fibrils of types II, V/XI, and IX, which maintains its gel-like structure. Other components are hyaluronic acid, NaCl, trace amounts of proteins and a small amount of hyalocytes in the vitreous cortex. With ageing, the vitreous body undergoes physiological changes. The vitreous liquifies (synchysis), and collagen fibrils aggregate into small bundles. Such vitreous changes might create an obstacle in the optical axis, leading to the perception of myodesopsias or “flying flies” that can be associated or not to posterior vitreous membrane detachment (PVD) [1]. Specifically, PVD is the result of the combination of vitreous liquefaction and weakened vitreoretinal adhesion, being present in more than 27% of patients over the age of 70 years and in 63% of patients over 80 years of age [2]. In PVD, a release of fibrous tissue around the optic nerve papilla can also be present, which forms an opacity in the shape of a ring or the letter C (the Weiss ring) [3]. In a large number of patients, this floater moves forward over time and descends in the vitreous cavity, resting finally at the bottom of the cavity and not causing visual disturbances. However, in a smaller number of patients, this opacity remains in the optical axis and casts a shadow on the retina, which can be strongly perceived by patients as a barrier to vision [3].
Vitreous opacities without PVD are caused by gradual synchysis and syneresis (collapse) of the vitreous body. At the age of 15-18 years, these changes have already occurred in approximately 20% of the vitreous volume, increasing up to 50% at the age of 80-90 years [4]. In myopic patients, this process is accelerated, with an aggregation of collagen fibrils in lacunae as a result of the loss of type IX collagen [5]. This leads to the formation of deposits inside the vitreous cavity, which, after reaching a certain size, can be perceived as bothersome dense vitreous opacities.
The perception of floaters due to vitreous opacities can disrupt or restrict everyday activities such as driving, working with the computer or reading. Thus, patients´ quality of life can be significantly impaired [6]. Until recently, two possible solutions were available for patients with significant disturbances due to floaters: adaptation to the opacity or undergoing pars plana vitrectomy [7-9], which is an invasive intervention with potential risk of complications, such as cataract progression in phakic patients, retinal detachment, or endophthalmitis [10, 11]. Laser vitreolysis is a relatively new option for removing vitreous opacities and solving the problem of floaters [12]. This technique is based on two principles: vaporization and mechanical disruption of opacities. The first effect – vaporization or photoplasmolysis – facilitates the conversion of fibrotic tissue into plasma. This conversion is possible thanks to the precise focusing of the laser beam into the target area, the vitreous, thus concentrating the maximum power in the area. This high power can exceed the ionisation threshold of the tissue, which then breaks down into ions and forms plasma. This is then resorbed during the circulation of the intraocular fluid, without leaving traces of opacities. The second effect mechanically disrupts the structure of the opacity, thus reducing its influence and the residues transfer to the periphery. In practice, a combination of both effects is applied [12]. Despite its potential benefit, this technique also some possible risks, although they are rare, including the development of cataracts or secondary glaucoma [13-15]. The aim of the current study was to evaluate the efficacy and safety of laser vitreolysis with a specific technology in a sample of patients of a public hospital with visual disturbances due to vitreous opacities.
2. MATERIALS AND METHODS
2.1. Patients
This was a prospective clinical study including 42 eyes of 35 patients with vitreous opacities generating visual disturbances. Specifically, only patients with visible vitreous opacities in the optical axis (Weiss ring or solitary dense opacities) were included, being the opacity was at a sufficient distance from the lens and retina. Exclusion criteria were the presence of asteroid hyalosis, opacity located at the periphery of the vitreous cavity or near one of the above-mentioned structures, and advanced cataract preventing optimal visualisation of the opacity. The study was conducted according to the tenets of the Declaration of Helsinki and was approved by the FNKV (hospital) ethics committee. All patients were informed about the nature of the study prior to their inclusion and signed an informed consent.
2.2. Clinical Protocol
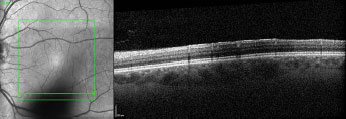
All the patients underwent a complete eye examination before the laser vitreolysis and at 1, 3 and 6 months after the intervention. At all visits, corrected distance visual acuity (CDVA) (ETDRS optotype), manifest refraction, central retinal thickness (CRT) and evaluation of the shadow generated by the opacity in the infrared fundus photography (OCT Spectralis, Heidelberg Engineering) (Fig. 1), and intraocular pressure (IOP) by contactless method (Auto Ref/Kerato/Tono/ Pachymeter TONOREF II, Nidek Co., LTD.) were measured. Likewise, IOP was also measured immediately after the intervention. Furthermore, at all visits, the anterior and posterior segment of the eye was examined using a slit lamp. Besides these tests, each patient completed a questionnaire (Appendix 1) to evaluate the patient’s subjective perception of the effect of the laser at each visit. Specifically, the patient had to assess the perception of opacities and how these were limiting for everyday activities. After the intervention, patients were also asked about the percentage of improvement in terms of the perception of opacities. Points were assigned to the items in the questionnaire for analysis purposes. The larger the number of points in the questionnaire, the greater the patient’s perception of the problem.
2.3. Laser Vitreolysis Procedure
All laser interventions were performed by one physician (Ernest A.) using an Ellex - Ultra Q Reflex YAG laser (Ultra Q Reflex-YAG, Ellex Medical, Australia). A contact lens, especially designed for this intervention (Singh MidVitreous, Volk optical) was used to correctly locate the opacity. The intervention was started by titrating the laser energy until an air bubble could be seen rising in the vitreous after hitting the opacity. This indicated that photoplasmolysis had been achieved, and the efficiency of the laser was at its highest. The total number of shots varied depending on the size and density of the opacity. The intervention was repeated whenever there was residual opacity in the optical axis. The intervention was performed on an outpatient basis, and no form of local therapy was applied to patients after the intervention.
2.4. Statistical Analysis
The STATISTICA program from StatSoft version 9.0 was used for data analysis. The Kolmogorv-Smirnov test was used first to confirm the normality of the data distributions. A paired t-test was used to statistically assess the significance of the change in CDVA and questionnaire scoring when variables were normally distributed. Otherwise, the Wilcoxon ranked test was used. A p-value <0.05 was considered as representative of statistical significance.
3. RESULTS
The sample that was evaluated consisted of 42 eyes of 35 patients with a mean age of 65 years (range 32-81 years). According to gender, the sample included 22 women (62.9%) and 13 men (37.1%). A total of 17 eyes (40.5%) were pseudophakic, and 25 eyes (59.5%) were phakic. Concerning the type of vitreous opacity, the presence of Weiss ring caused by PVD was found in 39 eyes (92.9%), with only 3 eyes (7.1%) showing dense vitreous opacities.
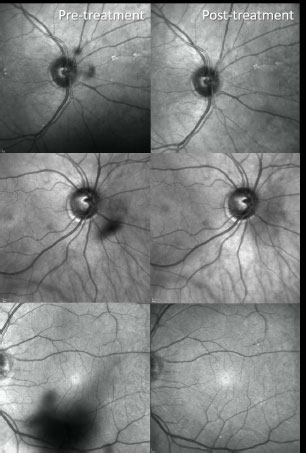
The laser intervention was performed only once in a total of 31 eyes (73.8%), whereas it was necessary to perform the intervention twice in 10 cases (23.8%) due to the presence of remaining opacities after the previous treatments. In one case, the intervention had to be performed thrice. The average number of laser shots was 118 (6 - 310 shots), with a total average energy of 3.8 mJ per laser shot (2.2 - 9 mJ). Using the infrared fundus image obtained with the optical coherence tomography system, a complete or partial reduction of the shadow generated by the opacity was found in all eyes (Fig. 2). In one of the patients, after several laser shots, the Weiss ring was located in the periphery of the vitreous cavity, no longer bothering the patient and, therefore, not programming more laser sessions. During the intervention and the entire follow-up period of 6 months after the intervention, no complications were detected in the sample.
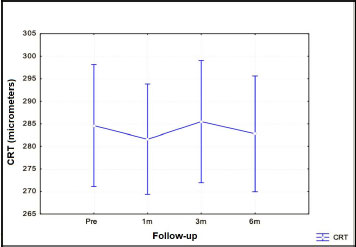
The mean pre-intervention CDVA was 83.2 ETDRS letters, changing to a mean post-intervention value at 6 months of 83.8 ETDRS letters. No significant differences in CDVA were detected during the whole follow-up (p>0.40). No significant changes were found in CRT (p> 0.32), as shown in Fig. (3). Concerning IOP, it was reduced significantly immediately after the intervention (p<0.001). However, a significant increase in IOP was observed at 1 month after the intervention (p<0.001), with no significant changes afterwards (p>0.22).
The analysis of the response of the questionnaire revealed that there was a mean improvement in subjective visual symptoms according to patients of 71%. In one case, there was no change in perceived symptoms, and no worsening was reported by any of the treated patients. The average number of points in the questionnaire before the treatment was 9.5, changing to 6.9 after the intervention. This change was statistically significant (p<0.001).
4. DISCUSSION
The presence of vitreous opacities significantly disrupts and limits the everyday activities of patients, which generates a negative impact on their quality of life.6 It is not uncommon that vitreous opacities lead to significant visual complaints, although the visual acuity is excellent, as in our sample (mean value of 82.9 letters). According to Wagle et al. [16] patients usually perceive vitreous opacity-related problems similar to patients who suffer from asymptomatic human immuno- deficiency virus (HIV) or colon cancer. Likewise, patients with vitreous opacities are willing to take risk, including 11% risk of death, a 7% risk of blindness, or give up one out of ten years of life to get rid of these problems [16]. Frequently, some patients are forced to leave their profession or take antidepressants permanently to alleviate the problem [17]. This was also confirmed in our series, with 8 out of 35 patients (23%) taking antidepressants or anxiolytics as a consequence of the problem of perception of floaters.
Until recently, pars plana vitrectomy was the only method to remove vitreous opacities [7-9]. However, it is an invasive procedure which poses potential risks. In a group of 47 patients operated on for vitreous opacities by 27 gauge pars plana vitrectomy, Lin et al. [7] reported complicated cases ofthe procedures, a case of endophthalmitis in 1 patient (2.1%) and also, retinal detachment in 1 patient (2.1%). De Nie et al. [9] operated on by vitrectomy bothersome vitreous opacities via 23 and 25-gauge pars plana vitrectomy. These authors found that retinal detachment occurred in 4.5% of operated eyes, epiretinal membrane formation occurred in 3.6% of cases, and cystoid macular edema occurred in 5.5% [9]. According to Schulz-Keye et al. [11], 60% of phakic patients after 20 gauge pars plana vitrectomy for vitreous opacities were also operated on for cataracts (with an average follow-up period of 37 months). In a sample of 64 patients who underwent pars plana vitrectomy for vitreous opacities, Hahn et al. [10] reported the occurrence of complications in 8 patients in the postoperative period: peri-operational crack in 6 patients (3.8%) and retinal detachment in 2 patients (1.28%). In our sample, laser vitreolysis was used for the management of floaters, with no complications occurring during the 6-month follow-up.
A complete or partial reduction of the floaters was found in all eyes, as confirmed by the infrared fundus image obtained with the optical coherence tomography system. Similar techniques were also used by other authors [3, 13, 18-21]. Specifically, Sun et al. [19] demonstrated that the quantification of floater shadow areas on infrared fundus photography could serve as an objective index for assessing the treatment efficacy of laser vitreolysis. The efficacy for the reduction of complete elimination of floaters in the current series was similar to that reported by several previous studies [13,18-20,22]. Luo et al. [13], in a sample of 30 eyes from 30 patients, (13 men, 17 women) undergoing YAG laser vitreolysis found that vitreous opacities partially or completely disappeared after the treatment, as confirmed by anterior segment photography. Nunes et al. [22] confirmed that vitreolysis efficacy observed at 6 months of follow-up was maintained until the eighteenth month, with no late adverse effects noted.
This partial or complete elimination of floaters with laser vitreolysis in our series was associated with a significant subjective improvement in symptoms. A self-developed questionnaire was used to investigate the impact on the subjective disturbances of patients. As expected, according to the research conducted earlier [6, 9, 10], a significant improvement in the scoring of the questionnaire was observed after the intervention, with a mean improvement of 71% as reported by patients. Janeková et al. [23] found that after laser vitreolysis, a total of 42% of patients reported a subjective improvement, where 9% of them were considered a complete success and 33% as a significant success. Luo et al. [13] found in the series that 75% of the patients reported significant improvement after laser vitreolysis, and 25% reported moderate improvement. In our series, the most significant improvement was observed in patients with small solitary opacities on the optical axis. By contrast, the smallest difference before and after the laser intervention was reported by patients with dense opacities, in whom, even objectively, there was always a small residue of opacity, which could not be removed by an additional application of the laser. These residues could be clearly identified using the infrared fundus image.
Besides all these benefits of laser vitreolysis, it should be considered that some possible risks with this technique have been described, although they are rare [13-15]. Shields et al. [24] described two cases of retinal problems after laser vitreolysis for the treatment of floaters: a case of vitreous haemorrhage and subsequent branch retinal vein occlusion from laser damage to a major retinal venule and a full-thickness retinal break in the posterior pole. In our series, no significant changes were observed in central retinal thickness after the intervention. Luo et al. [13] did not find significant changes during a 6-month follow-up after the intervention in the thickness of the retinal nerve fibre layer. Koo et al. [14] observed in their series cataract formation in 2 patients after laser vitreolysis. Cataract formation may be affected by excessive applied energy or inappropriate opacity location – opacities too close to the lens. In our series, the formation of cataracts after surgery was not observed in any case. Cowan et al. [15] published the results of the treatment with laser vitreolysis of three eyes of two patients with an elevation of IOP requiring local or surgical anti-glaucoma therapy after the intervention. In our sample, no IOP elevation was observed in any patient during the follow-up period. On the contrary, immediately after the intervention, a statistically significant decrease in IOP was found. This may be attributed to the potential massage of the bulb when the laser contact lens was used. More research is still needed to confirm the safety in the long term of this therapy for the treatment of floaters.
Despite the advantages and disadvantages mentioned of laser vitreolysis, it is necessary to consider carefully its indication. According to our experience, pars plana vitrectomy may be the method of choice for removing diffuse dense vitreous opacities or opacities in the periphery of the vitreous cavity, as well as in patients with asteroid hyalosis. Alternatively, vitrectomy is indicated in patients when sufficiently broad artificial mydriasis cannot be induced to adequately visualize opacities. Laser vitreolysis is the method of choice to remove minor opacities, especially the Weiss ring or its parts on the optical axis. It should be considered that the individual patient characteristics and the type and location of opacities may influence the treatment outcome, therefore, a strict patient selection is essential for obtaining optimal results and avoiding complications. Another indisputable advantage of laser vitreolysis is the short recovery time after the intervention. After the mydriasis subsides, patients are completely unrestricted. Future studies should confirm the most adequate indications of laser vitreolysis in order to establish evidence-based clinical protocols for the management of vitreous opacities.
This study has several limitations that should be acknowledged. First, the sample size was limited requiring more studies with larger samples to confirm the outcomes obtained in the current series. Second, this was not a controlled study, without the control group or randomization and therefore, some level of bias may be associated with the outcomes obtained. In any case, it should be noted that the trends found in the current series were compatible with those obtained in other previous studies evaluating the safety of laser vitreolysis for the management of floaters. Third, a non-validated questionnaire was used to assess the subjective impact of the intervention. A validated symptom questionnaire should be used in future studies in order to extract more consistent conclusion about the subjective benefit of this type of treatment.
CONCLUSION
To sum up, laser vitreolysis is a minimally invasive treatment. With adequate titration of the energy applied and adherence to the basic rules of laser application, this therapy is an effective and safe method for solving bothersome vitreous opacities, thus enabling partial or complete reduction of opacity in the optical axis.
LIST OF ABBREVIATIONS
| PVD | = Posterior vitreous membrane detachment |
| CRT | = Central retinal thickness |
| OCT | = Optical coherence tomography system |
| HIV | = Human immuno-deficiency virus |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the FNKV (hospital) ethics committee.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or Research Committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
All patients were informed about the nature of the study prior to their inclusion and signed an informed consent.
AVAILABILITY OF DATA AND MATERIALS
The data supporting the findings of the article is available on reasonable request [D.P] to the author.
FUNDING
None.
CONFLICT OF INTEREST
The authors have no conflict of interest related to the material involved in this manuscript.
ACKNOWLEDGEMENTS
The authors are grateful to Dr. Ian McColl, MD, Ph. D., for assistance with the manuscript.
DISCLOSURE
The authors have no proprietary or commercial interest in the medical devices that are involved in this manuscript.
APPENDIX 1
Questionnaire: Evaluation of perception of vitreous opacities - before and after laser vitreolysis
Name ................................................................................
Side: OD / OS
Date ............................
1. Do you perceive vitreous opacities?
[a] Not at all
[b] Sometimes I perceive these opacities
[c] Usually I perceive these opacities
[d] Always I perceive these opacities 3
2. What is the influence for daily activities such as driving car, watching television?
[a] I do not perceive these opacities during these activities
[b] I perceive opacities, but they are not disturbing
[c] I perceive opacities and they are sometimes disturbing
[d] I perceive opacities and they are usually disturbing
[e] I am not able to perform these activities due to opacities 4
3. What is the influence for activities such as reading, work with computer?
[a] I do not perceive these opacities during these activities
[b] I perceive opacities, but they are not disturbing
[c] I perceive opacities and they are sometimes disturbing
[d] I perceive opacities and they are usually disturbing
[e] I am not able to perform these activities due to opacities 4
4. What is the effect of the laser? Is there any improvement?
0-100%


