All published articles of this journal are available on ScienceDirect.
Pupillary Diameter Change and Dynamics in Different Refractive Error Groups after Implantation of a Collamer Lens with a Central Hole Without Viscoelastic Agent
Abstract
Background:
To investigate the pupillary diameter and dynamics in different refractive error groups after non-viscoelastic agent-assisted implantation of a collamer lens with a central hole, so as to evaluate the effect on the pupil of this type of surgery.
Methods:
Consecutive patients with a range of refractive errors who underwent non-viscoelastic agent-assisted implantation of a collamer lens with a central hole (ICL V4c) were analyzed. OPD-Scan III (NIDEK Japan)was used to measure the pupillary diameter preoperatively and 1 month postoperatively. Pupillary dynamics were assessed by calculating the scotopic pupillary diameter minus the photopic pupillary diameter. All variables were measured under photopic and scotopic conditions.
Results:
In 53 patients (medium-low myopia group 44 eyes, 23 patients, age 33.3±1.2 years and high myopia group 60 eyes, 30 patients, age 31.7±1.5 years), the postoperative photopic pupil was significantly smaller than preoperatively in both groups, and the postoperative pupillary size was significantly larger in the high myopia group under both the photopic and scotopic conditions. Besides, the high myopia group had a significantly larger photopic-scotopic change postoperatively and greater change in the pupillary dynamics.
Conclusion:
Implantation of a collamer lens with a central hole without viscoelastic agent assistance affected the pupillary diameter and dynamics at 1 month postoperatively in the medium-low and high myopia groups. The group with medium and low diopters had stronger changes in pupil diameter after surgery, while the group with high diopters was more likely to be affected by changes in visual quality.
1. INTRODUCTION
The implantable collamer lens (ICL) with a central hole (ICL V4c) (STAAR Surgical) has been proven to be a safe and effective method to correct myopia since its introduction in 2011 [1]. The newly designed central hole of 360 µm allows aqueous humor to flow without iridectomy [2], which further expands the indications of the lens.
The surgical technique of ICL implantation is also improving. The conventional implantation procedure was the viscoelastic agent-assisted technique [3]. However, intraocular pressure (IOP) elevation sometimes seen following the use of viscoelastics is usually transient. The IOP spike is generally seen within 6 to 24 hours postoperatively. In most cases, the IOP returns to normal within 72 hours postoperatively [4]. Without the use of viscoelastic agents can avoid the impact on the intraocular pressure, so non-viscoelastic agent-assisted implantation is increasingly being used [5].
It is well known that the pupillary diameter and response are closely related to the visual quality after ICL implantation. For example, many studies have shown that the dynamic pupillary light response plays a significant role in halo development after conditional ICL implantation [6, 7]. Halos cause many visual complications, especially while driving at night.
At the same time, to better investigate its effects, we grouped all patients according to their diopters, so the present study was performed to investigate the changes in pupillary light response to different light intensities before and after non-viscoelastic agent-assisted ICL V4c implantation, and compare the changes in pupillary diameter in patients with different diopters.
2. PATIENTS AND METHODS
The study was approved by the Ethics Committee of Beijing Anzhen Hospital. All relevant tenets of the Declaration of Helsinki were followed. Written informed consent was obtained from all participants.
2.1. Sample
This consecutive, observational, retrospective study included 53 patients who underwent ICL V4c implantation from August 2019 to January 2021 at Beijing Anzhen Hospital in China. All patients who received an ICL met the following surgical indications: age 20-40 years, stable refractive error for at least 1 year. The exclusion criteria were: any ocular or systemic disease or anomaly that might affect the pupillary diameter or light perception, history of the use of any medications that might affect iris mechanics, and previous ocular surgery.
2.2. Evaluated Variables
All patients underwent a comprehensive ophthalmologic examination before surgery to assess the following variables: (1) uncorrected distance visual acuity, best-corrected distance visual acuity, IOP (Topcon CT-80A Japan), endothelial cell density (Topcon SP-3000P Japan), slit lamp examination and funduscopic examination (2) spherical equivalent, anterior chamber depth, and central corneal thickness with the IOLMaster 700 (ZEISS German), (3) white-to-white diameter assessed with both the IOLMaster and ultrasound biomicroscopy. The ICL power and size were determined in accordance with the manufacturer’s recommendations using an online calculator. General history and medication history were also obtained.
2.3. Operation Procedure
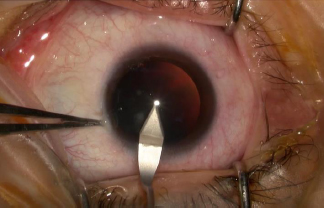
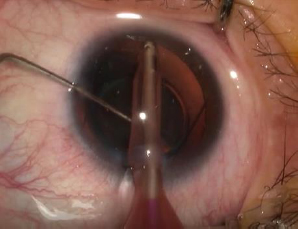
Patients were instructed to use levofloxacin eye drops for 3 days before surgery. All surgeries were performed by one experienced surgeon (ZSQ) in the same operation room. A mydriatic agent was applied three times in 1 hour before surgery to minimize the effects of the drug acting on the pupil. An ICL V4c was inserted through a 3.0 mm clear corneal incision (Fig. 1) without sodium hyaluronate use in the anterior chamber (Fig. 2). The ICL was then adjusted to the posterior chamber by irrigation with a balanced salt solution (Fig. 3). Pupils were naturally constricted without drugs after the surgery. Tobramycin and dexamethasone eye drops and recombinant bovine basic fibroblast growth factor eye drops were administered postoperatively three times daily for 1 week, then replaced by bromfenac sodium hydrate ophthalmic solution twice daily for 2 weeks.

2.4. Measurements of Pupillary Diameter and Pupillary Dynamics
OPD Scan was used to measure the pupillary diameter before and 1 month after ICL implantation. All examinations were performed by one clinician (WH) in the same room between 08:00 and 11:00 in the morning. Measurements were performed after 15 minutes of light adaption. The average pupillary diameters under two standardized illumination conditions were recorded after at least three consecutive measurements at each illumination level. The pupillary dynamics were assessed by subtracting the difference between the scotopic and photopic pupils (scotopic pupillary diameter minus the photopic pupillary diameter).
2.5. Statistical Analyses
All results were analyzed using the Statistical Package for the Social Sciences version 22.0 (IBM). Data are expressed as mean±standard deviation. The appropriate statistical analysis method was selected based on whether the data were normally distributed and had homogeneity of variance. P values <0.05 were considered statistically significant.
All patients were separated based on their refractive error into the medium-low myopia group (diopter -6D to 0D) or the high myopia group (diopter < -6D). The pre- and postoperative pupillary diameters in the photopic and scotopic conditions were compared between and within these two groups.
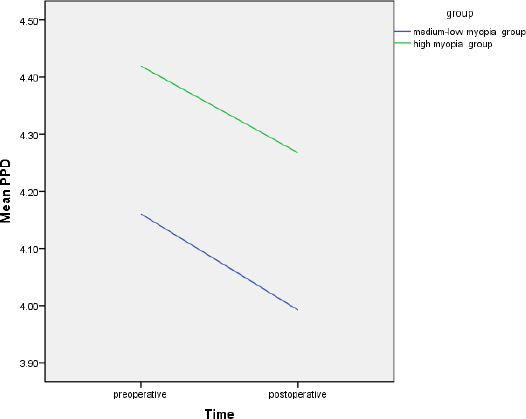
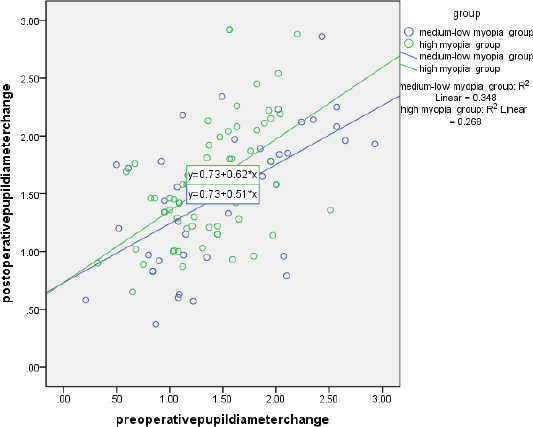
3. RESULTS
A total of 53 patients (104 eyes) were included. All patients were separated into medium-low myopia group and high myopia group in accordance with their preoperative spherical equivalent measurements. The medium-low myopia group comprised 44 eyes (23 patients, age 33.3±1.2 years, six men), while the high myopia group comprised 60 eyes (30 patients, age 31.7±1.5 years, five men). The patient and ocular characteristics are shown in Table 1. There were no significant differences between groups in age (P=0.59) and sex (P=0.31). Intragroup comparisons showed that the postoperative photopic pupil was significantly smaller than the preoperative one in both the medium-low myopia group (P=0.02) and the high myopia group (P=0.003). However, there was no significant change in the scotopic pupillary size (Table 2). Table 3 demonstrates that the preoperative pupillary size did not significantly differ between the two groups under both the photopic and scotopic conditions, but the postoperative pupillary size was significantly larger in the high myopia group than the medium-low myopia group under both the photopic and scotopic conditions. There is a decreasing tendency of pupil size under both photopic and scotopic conditions in medium-low myopia group after the ICL implantation, but an increasing tendency of scotopic pupil size in the high myopia group which is opposite to the photopic condition (Fig. 4). Table 4 shows the postoperative change in pupillary dynamics in the two groups; the high myopia group had a significantly larger change in pupillary dynamics postoperatively (1.59±0.53) versus preoperatively (1.39±0.44). In the high myopia group, the change in pupil diameter after the operation is more significantly correlated with that before the operation (Fig. 5).
| - | Medium-low Myopia Group | High Myopia Group | P | |
|---|---|---|---|---|
| N(eyes, patients) | 44, 23 | 60, 30 | - | |
| Men, Female | 6, 17 | 5, 25 | 0.31Chi-Square Tests * | |
| Age(yr) | 33.3±1.2 | 31.7±1.5 | 0.59Mann-Whitney Test * | |
| spherical equivalent refraction(D) | -4.76±0.17(-1.75 to -6.00) | -10.12±0.33(-6.50 to -17.50) | - | |
| IOP(mmHg) | Before | 15.98±0.30 | 15.98±0.23 | - |
| after | 15.46±0.32 | 15.45±0.29 | ||
| P=0.27Wilcoxon Signed Ranks Test* | P=0.05Wilcoxon Signed Ranks Test* | - | ||
| Group | - | Puiple Size | P | ||
|---|---|---|---|---|---|
| before | after | ||||
| medium-low myopia group | Photopic condition | 4.16±0.09[3.12, 6.23] | 3.99±0.10[3.28, 7.09] | 0.02T-Test* | |
| scotopic condition | 5.63±0.13[3.92, 7.31] | 5.48±0.12[4.09, 7.69] | 0.06Wilcoxon Signed Ranks Test* | ||
| high myopia | Photopic condition | 4.42±0.10[3.26, 7.51] | 4.27±0.10[3.24, 6.56] | 0.003Wilcoxon Signed Ranks Test* | |
| scotopic condition | 5.81±0.84[4.30, 8.19] | 5.86±0.89[4.34, 7.88] | 0.32T-Test* | ||
| Pupil Size | Medium-low Myopia Group | High Myopia | P | |
|---|---|---|---|---|
| Before | Photopic condition | 4.16±0.09[3.12, 6.23] | 4.42±0.10[3.26, 7.51] | 0.13Mann-Whitney Test* |
| scotopic condition | 5.63±0.13[3.92, 7.31] | 5.81±0.11[4.30, 8.19] | 0.32 ANOVA* | |
| After | Photopic condition | 3.99±0.10[3.28, 7.09] | 4.27±0.10[3.24, 6.56] | 0.04Mann-Whitney Test* |
| scotopic condition | 5.48±0.12[4.09, 7.69] | 5.86±0.11[4.34, 7.88] | 0.03ANOVA* | |
| Pupil Dynamics | Medium-low Myopia Group | High Myopia | P |
|---|---|---|---|
| Before | 1.47±0.10 | 1.39±0.44 | 0.76Mann-Whitney Test* |
| After | 1.48±0.09 | 1.59±0.53 | 0.47Mann-Whitney Test* |
| P | 0.9T-Test* | 0.002T-Test* | - |
4. DISCUSSION
Viscoelastic agents are widely used in ICL implantation to maintain the anterior chamber and protect the corneal endothelium functions [8, 9]. However, viscoelastic agent residue may increase the postoperative IOP due to obstruction of the trabecular meshwork and the canal of Schlemm [10]. Niruthisard et al. [11] reported one patient in whom ICL implantation resulted in a fixed dilated pupil, which was thought to be related to the viscoelastic agent residue. Miao et al. [9] proposed a one-step technique for ICL V4c implantation in which a small amount of viscoelastic surgical agent is used to adjust the haptic resting in the anterior chamber. However, although the IOP of all eyes decreased to baseline value at 1 day postoperatively with routine postoperative medication, four eyes had an IOP of greater than 30 mm Hg (maximum 35 mm Hg) and required corneal paracentesis 3 hours postoperatively.
In our study, the non-viscoelastic agent implantation method was adopted for ICL implantation, and the creation of an incision with good tightness was an important step. The intraoperative ICL position was adjusted underwater flow surrounded by a balanced salt solution, which not only maintained the anterior chamber space but also avoided the adverse effects caused by incomplete viscoelastic agent removal. None of the patients had an IOP of more than 21 mmHg on reexamination performed 1 day after surgery.
The pupillary changes in our study (decreased pupillary diameter after surgery) are consistent with most previous study findings. Keuch et al. [7, 11] used a pupillograph to assess pupillary constriction after the implantation of an ICL without a central port (model V4) and found that the pupillary diameter was significantly smaller at 2 weeks postoperatively than before surgery (P < 0.01). Lim et al. [12] used a WaveScan aberrometer to evaluate the pupillary size before and 6 months after surgery under mesopic conditions (50 l×) and found a significant decrease in 64% of eyes, an increase in 20%, and
no change in 16%. However, other studies have reported different results. Gonzalez-Lopez et al. [13] used Fourier-domain anterior segment optical coherence tomography to perform dynamic pupillometry under photopic and scotopic conditions before and 4 months after surgery. Their results showed the mean pupillary diameter at 4 months postoperatively was larger than the mean pupillary diameter before surgery, under both photopic and scotopic conditions. Zhu et al. [14] investigated the pupillary diameter change after ICL implantation in highly myopic eyes and found no changes in the high-myopia group but a significant decrease under all illumination conditions in the super-high-myopia group at 1 and 3 months postoperatively. Although our study did not distinguish between high-myopia and super-high-myopia, this differs from the significant decrease in pupillary size under the photopic condition found in the high myopia group in our study. This intergroup difference may be due to the routine postoperative constriction using 0.01% (w/v) acetylcholine applied by Zhu et al.
There are few reports on the pupillary dynamic changes after ICL implantation. Our study is the first to compare the pupillary diameter changes under photopic and scotopic conditions to evaluate the pupillary dynamics in different diopter groups. Totsuka et al. [15] assessed the pupillary light reflex after ICL implantation in patients with diopter values ranging from -3.25D to -11.80D using the infrared pupillometer Iriscorder C7364 (Hamamatsu Photonics) but found no significant change in pupillary dynamics at 6 months after implantation. Kato et al. [16] used anterior segment optical coherence tomography to examine dynamic pupillary changes under photopic and scotopic conditions and found that the pupillary size was significantly smaller during accommodation (3.88 ± 0.64 vs. 4.10 ± 0.61 mm, P < 0.001). These discrepancies between studies may be due to variations in surgical methods, grouping methods, and observation times.
There is no clear theory as to why pupil activity is affected with viscoelastic-free use, and this experiment speculates that it may have something to do with factors such as whether ICL lens implantation partially reduces the posterior chamber space, thereby affecting atrial water circulation, or whether the crystal loops in the ciliary sulcus may partially affect the root of the iris, thereby affecting pupillary light-reflective dynamics, or even whether surgical manipulation of an open eye alone alters the micro-environmental balance of a portion of the eye, thereby affecting the pupil. environmental balance and thus affect the pupil. These issues need to be further investigated and explored.
Our study had some limitations. The postoperative observation time was only 1 month, which is relatively short. We will continue to monitor the long-term postoperative pupillary changes. Moreover, the small sample size makes it impossible to accurately analyze the data and draw more definite conclusions. We will continue to expand the sample size and perform relevant studies.
4.1. Value Statement
4.1.1. What was Known
1. Previous studies have found that ICL implantation can significantly reduce pupil size in the short term after surgery.
2. There are few studies on dynamic changes in pupils during ICL surgery.
4.1.2. What this Paper Adds
1. This is the first study to compare the changes in pupil diameter and dynamic changes in different diopter groups.
2. This study is the first to study pupil changes in ICL surgery without viscoelastic agent implantation.
3. In this study, it was found for the first time that the pupils of different diopter groups showed different changes after ICL implantation.
CONCLUSION
This study attempts to compare the influence of ICL implantation on the pupil of people with different diopters and to study the relationship between the pupil change response and diopter, so as to provide a certain research basis for the influence of visual quality brought by the pupil.
LIST OF ABBREVIATIONS
| ICL | = Implantable Collamer Lens |
| IOP | = Intraocular Pressure |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the ethics committee of Beijing Anzhen hospital.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information is available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


