All published articles of this journal are available on ScienceDirect.
Conjunctival Balloon Cell Nevus in a Young Child: A Case Report
Abstract
Background:
Conjunctival balloon cell nevus is rare and often presents in young adults to middle-aged patients with a longstanding history of melanocytic lesion, suggestive of benign pathology. The main treatment modality is excisional biopsy. Tumor recurrence is very rare. Malignant transformation has never been reported.
Objective:
This study aimed to report a case of conjunctival balloon cell nevus with an atypical presentation in a preschooler.
Methods:
We describe a case of a 5-year-and-9-month-old girl who presented with a rapidly growing melanocytic conjunctival mass, which she had since birth. Ophthalmic examination showed two prominent feeder vessels, and the lesion straddled the limbus to overlie the peripheral part of the cornea. These findings raised an index of suspicion of malignant transformation. The lesion was completely excised with a 2-mm resection margin, superficial keratectomy, ethyl alcohol epitheliectomy, and cryotherapy.
Results and Discussion:
The histopathological examination and immunohistochemical study showed a compound conjunctival nevus of the conjunctiva with most of the cells as balloon cell type. There were no malignant changes found. Moreover, there were no signs of tumor recurrence at the last follow-up of 6 months.
Conclusion:
Clinically malignant characteristics have never been reported in balloon cell nevi in a preschooler of this age. Thorough physical examination, well-planned surgical procedure, and careful pathological examination all play vital roles in the management of patients with these lesions.
1. INTRODUCTION
Clear cell melanocytic lesions can be classified as balloon cells and sebocyte-like melanocytes by histopathological and immunohistochemical characteristics [1]. Balloon cell nevi are uncommon, mostly found in younger age groups, and usually present at the head and neck region followed by the trunk and extremities [1, 2]. The lesions are extremely rare in the conjunctiva. Pfaffenbach et al., in 1972, first described a balloon cell nevus in a 39-year-old female patient who presented with recurrent conjunctival melanocytic lesion from the age of 25 [3]. Thompson JM et al. in 2015 reported 3 cases of this entity and reviewed the literature [4]. They found 12 other reported cases of conjunctival or caruncular balloon cell nevi [5-13].
We searched PubMed and Scopus databases using the keywords “balloon cell,” “nevus or nevi,” and “conjunctiva,” and we found 4 additional cases [14, 15]. Therefore, there were only 20 previously reported cases of conjunctival or caruncular balloon cell nevi from different parts of the world.
From the previous studies, the age of presentation ranged from 6 to 44 years, with an average age of 20.1 years. The female gender was predominant. The main presenting symptom of conjunctival balloon cell nevus was a longstanding history of the partial pigmented mass at the bulbar conjunctiva. A light microscopic pathological examination has been the mainstay of the diagnostic tools.
Transmission electron microscopy of balloon cell nevus was reported by Hashimoto et al. in 1972 as the presence of varying sizes of vacuoles and cavities in the cytoplasm with some areas showing coalescence of small vacuoles. Non-melanized melanosomes were seen in these cells [16]. Similar features were noted in later reports of the conjunctival lesions [9, 17].
Conjunctival melanoma with balloon cell transformation was first reported in 1988 [18]. Atypical conjunctival nevi are rather difficult to diagnose from conjunctival melanoma. However, with the use of immunohistochemistry, the characteristics of melanoma were described, and it was considered an additional investigative procedure for the final pathological diagnoses [19]. The immunohistochemical stains were also shown to be helpful in the diagnosis of melanocytic lesions in the conjunctiva [11, 20].
Since balloon cell nevi of the conjunctiva are rarely found, the therapeutic approaches usually depend on the surgeons’ decisions. Mostly the nevi with benign presentation are treated with excisional biopsy [3, 4, 9, 10, 12, 13, 15]. Only one case has been reported to have multiple recurrences [3]. There have not been any reports of malignant transformation.
Herein, the authors report a case of balloon cell nevus of the conjunctiva in a young child with an atypical clinical presentation. The light microscopic pathological examination, as well as the immunohistochemical stains, are described.
2. CASE PRESENTATION
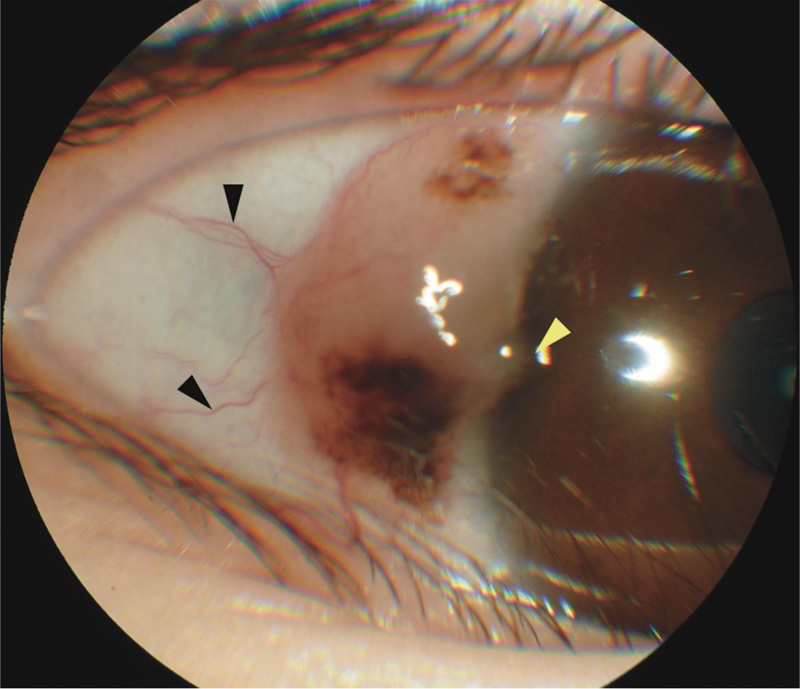
A 5-year-and-9-month-old healthy female of Chinese descent presented with a history of a small pigmented conjunctival mass at the temporal limbus of the right eye since birth. The mass increased its size rapidly within a month prior to presentation. Ophthalmic examination showed a translucent velvety conjunctival mass measuring 8 mm in length, 4 mm in width, and 2 mm in thickness, with dark brown patches at the superior and inferior parts. There was no cystic component in the mass. Two prominent feeder vessels were seen at the temporal bulbar conjunctiva. There was a small area at the temporal limbus showing corneal epithelial involvement of the lesion (Fig. 1).
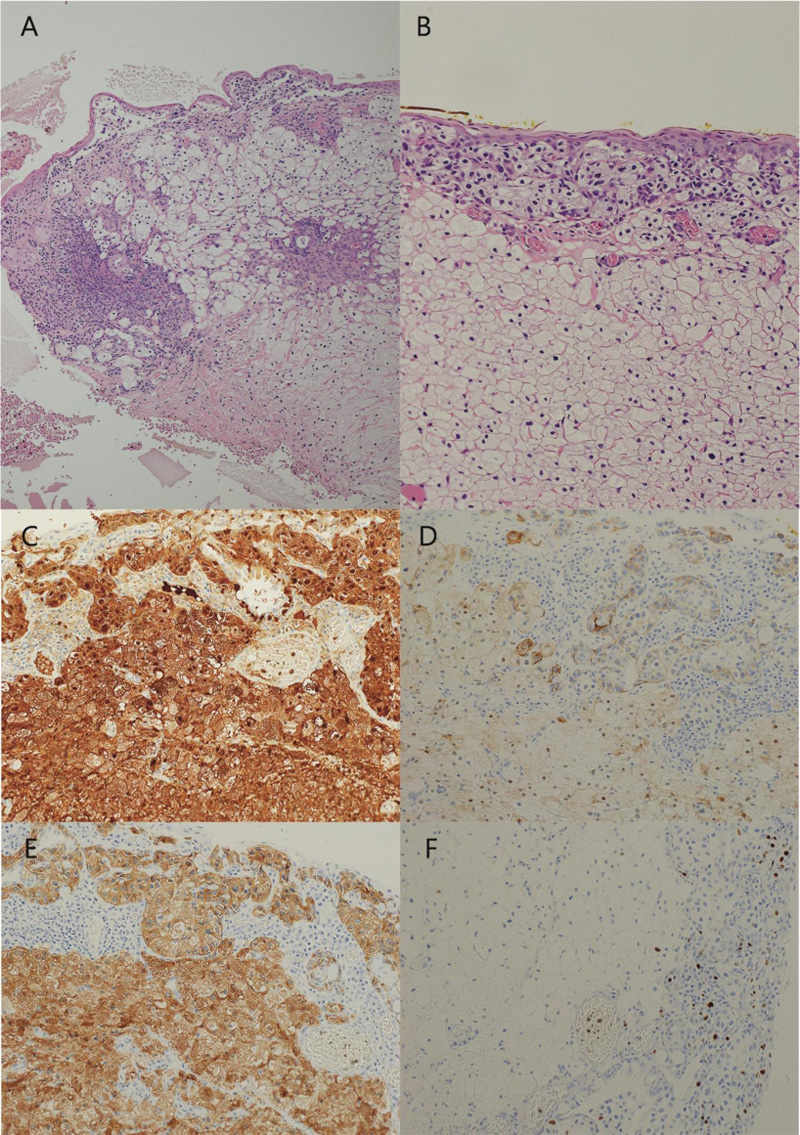
Due to clinical history of rapid growth, presentation of prominent feeder vessels, and corneal involvement, the diagnosis of conjunctival malignancy could not be ruled out. After discussion with the patient’s parents, conjunctival mass excisional biopsy with a 2-mm resection margin, superficial keratectomy, ethyl alcohol epitheliectomy, and cryotherapy were performed under general anesthesia. Pathological examination showed the presence of nevus nests at the epithelium to substantia propria junction and in the substantia propria. Multiple small conjunctival epithelial inclusion cysts were observed in the substantia propria. Numerous balloon cells, without significant cellular atypia nor nuclear atypia, occupied most of the stromal part of the lesion. Mitotic figures were rarely seen. The immunohistochemical stains showed that the balloon cells were strongly positive with S-100 protein, faintly positive with HMB-45, moderately positive with Melan-A, and negatively stained with Ki-67 (Fig. 2).
The histopathology examination concluded that the lesion was a compound conjunctival nevus, presenting as a balloon cell type. The lesion was totally excised. Follow-up examination at 6 months showed conjunctival scar without tumor recurrence. The patient’s follow-up scheme is to visit the clinic for a thorough slit-lamp biomicroscopic examination every 6 months.
3. RESULTS AND DISCUSSION
Balloon cell nevi of the conjunctiva are uncommon, mostly occurring in young adults to middle-aged patients [3-15]. The presentation, in this case, is relatively rare as it was in a preschooler, yet the clinical appearance could not exclude malignant changes. In this setting, a thorough examination and a well-planned surgical procedure should always be considered. The pathological examination played an important role in this case and finally showed the benignity of the lesion.
A pathological diagnosis of balloon cell nevus of the conjunctiva is rather difficult due to the rarity of the disease and the appearance of the cells. It should be differentially diagnosed with other clear cell melanocytic tumors [1]. Balloon cell types may also preclude pathologists from the differentiation between benign nevus cells and malignant melanoma. In the present case, the appearance of type-B nevus cells in the vicinity of balloon cells, lack of atypia, rarity of mitosis, and immunohistochemical stains were helpful with the diagnosis.
Transmission electron microscopy was used to demonstrate rarified melanosomes in balloon cells but could not signify the benignity or malignancy of the lesion [9, 17, 18]. We would not recommend its use due to low cost-effectiveness and because the instrument is not readily accessible in general settings.
Treatment modalities varied from case to case in reported literature, with an excisional biopsy as the main option. In our case, the lesion mimicked malignant transformation; thus, an excisional biopsy with a 2-mm resection margin, superficial keratectomy, ethyl alcohol epitheliectomy, and cryotherapy was performed. There was no recurrence of the lesion at the latest visit.
CONCLUSION
We report a case of compound balloon cell conjunctival nevus presenting with an atypical presentation in a very young child. Thorough ophthalmic examination, well-planned surgery, prudent histopathological examination, and comprehensive selection of immunohistochemical stains are essential for optimal patient care.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was exempted from ethics review by the Institutional Review Board, Faculty of Medicine, Chulalongkorn University, Certificate of Exemption number 022/2021.
HUMAN AND ANIMAL RIGHTS
No animals were used in the studies that are the basis of this research. All the humans used were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient’s parents.
STANDARDS OF REPORTING
CARE guidelines and methodologies were follwed in this study.
AVAILABILITY OF DATA AND MATERIALS
The authors confirm that the data supporting the findings of this study are available within the article, and further information is available from the corresponding author, [W.T.], on special request.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We thank Ms. Sranya Phaisawang and the English editing service, Research Affairs, Faculty of Medicine, Chulalongkorn University, for assistance in the manuscript preparation.


